Translate this page into:
Use of monopolar and bipolar radiofrequency probes for treatment of cutaneous leiomyoma
*Corresponding author: Sushama Sushama, Department of Dermatology, All India Institute of Medical Sciences, Bathinda 151005, Punjab, India. singh.sushama@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bansal S, Sushama S, Brar AK, Rana MK. Use of monopolar and bipolar radiofrequency probes for treatment of cutaneous leiomyoma. J Cutan Aesthet Surg. doi: 10.4103/JCAS.JCAS_78_23
Abstract
Cutaneous leiomyomas are tumors of smooth muscle origin which appear as erythematous papules and nodules that are mostly painful to touch. Although surgical excision is the gold standard treatment, other destructive methods such as electrodessication, cryotherapy or carbon-dioxide laser may also be done for cure. Our patient presented with painful cutaneous leiomyomas which resolved well with radiofrequency ablation done with two different techniques using monopolar and bipolar radiofrequency probes. There was no recurrence at 8 months follow-up.
Keywords
Bipolar
Intralesional
Leiomyoma
Radiofrequency
Treatment
INTRODUCTION
Cutaneous leiomyomas are rare, sporadic, or inherited tumors of smooth muscle origin. Clinically they appear as erythematous papules and nodules which are mostly painful to touch, cold, pressure, or emotion.1 Although surgical excision is the gold standard treatment,2 other destructive methods such as electrodesiccation, cryotherapy, or carbon dioxide laser may also be done for cure.3 Our patient presented with painful cutaneous leiomyomas which resolved well with radiofrequency ablation done with two different techniques and no recurrence at 8 months follow-up.
CASE
A 50-year-old male patient presented to us with the complaint of a painful, reddish lesion on the right side chest [Figure 1]. On examination, there were translucent, erythematous, tender, papules and nodules on the right side chest [Figure 1a]. Histopathological examination of the hematoxylin and eosin-stained section of the biopsy specimen confirmed the clinical diagnosis of segmental leiomyoma [Figure 2]. Surgical excision of the lesions was not feasible because of the relatively wide distribution of lesions. A decision to treat with radiofrequency ablation of the lesions was taken. To anesthetize the area, a field block was done with 2% lignocaine with the help of a lumbar puncture needle. Intralesional radiofrequency ablation was done with the help of a cannula (20G) in coagulation mode (DIVLABS RF machine, Divlabs Healthcare Pvt. Ltd., India) [Figure 3a]. The plastic sheath of the cannula was cut and a window of bare metal area was made at the proximal end. After inserting the tip of the cannula inside the lesion, the metal part of the window created on the cannula was touched with the radiofrequency probe to deliver the electric current until blanching was seen. The intact plastic part of the cannula near the lesion provides insulation and prevents damage to the skin at the entry point. Intralesional RF damages the dermal and subdermal structures and hence helps in the ablation of lesions. However, lesions of larger size showed recurrence of growth at 4 months follow-up [Figure 1b]. For the sessile larger lesions, we also used a bipolar probe for the ablation of the lesion.
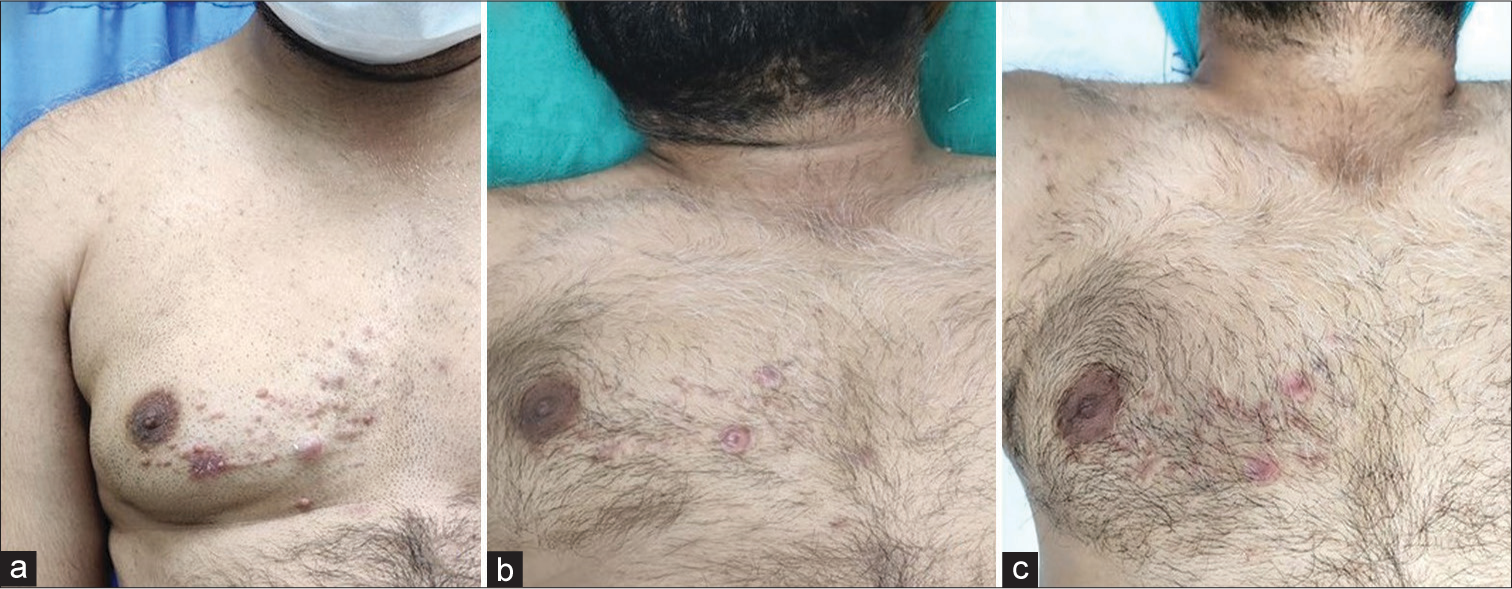
- (a) Erythematous, tender, papules and nodules on the right side chest. (b) Follow-up at 4 months: resolution of smaller lesions after intralesional radiofrequency ablation. Larger lesions persisting. (c) Follow-up at 6 months: the resolution of larger lesions after radiofrequency ablation with bipolar probe.
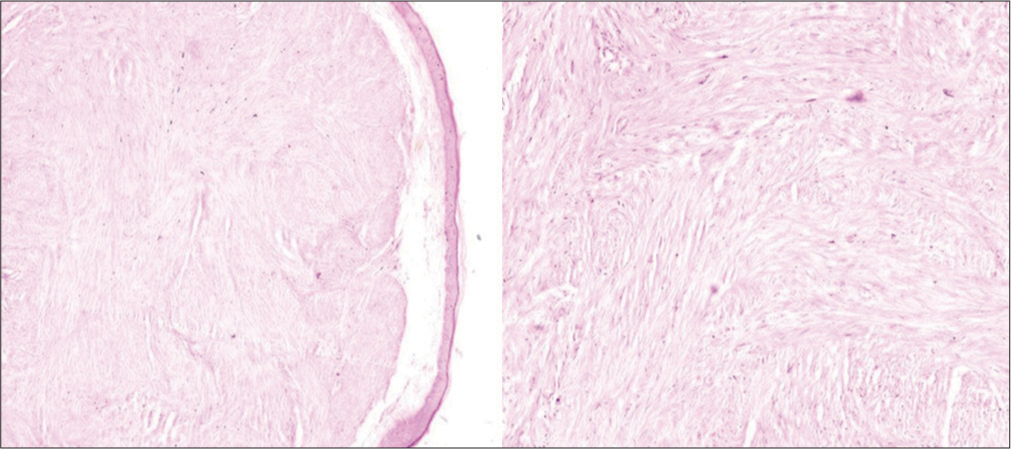
- Neoplastic cells with features of smooth muscles seen in the reticular dermis in the section of biopsy specimen (hematoxylin and eosin stain; 100×).
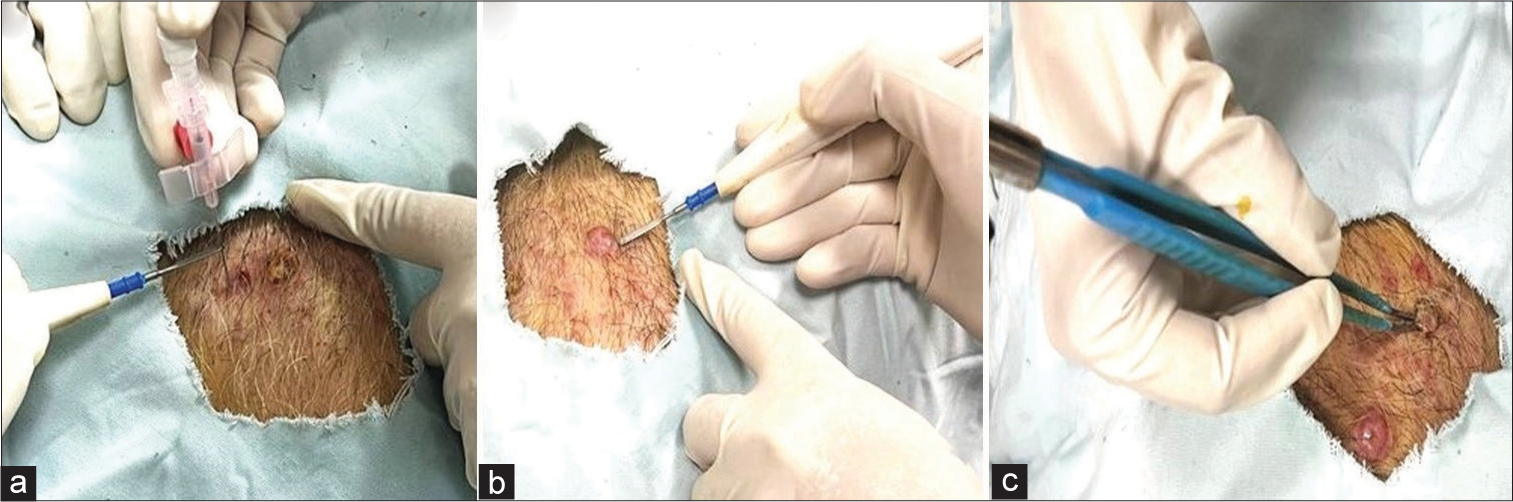
- (a) Intralesional radiofrequency ablation with 20G cannula. (b) Tunnels on the wall of the lesion made with monopolar radiofrequency probe. (c) Two poles of the bipolar probe inserted into two adjacent tunnels at a time.
Multiple tunnels (4–6) were made at a distance of 5 mm on the wall of the lesion circumferentially through a monopolar radiofrequency probe in cutting mode [Figure 3b]. Through the tunnels created, two poles of bipolar probe were inserted into two adjacent tunnels at a time [Figure 3c]. Ablation was done with a bipolar probe till blanching was seen. Thereafter, the lesion was completely cut with the monopolar probe in cutting mode. The lesions responded well and resolved within 2 weeks [Figure 1c]. No recurrence was seen at the site of ablation at 8 months follow-up.
DISCUSSION
Most of the piloleiomyomas are painful for which the patient seeks treatment. Surgical excision is the gold standard for cure.2 However, surgical excision is cumbersome in patients with multiple lesions. Other methods include destruction via electrodessication, cryotherapy, or carbon dioxide laser.3 Post-procedure hypopigmentation may be a side effect of cryotherapy whereas cost is an issue with carbon dioxide laser therapy. In our case, since the lesions were widely distributed on the upper back, excision was not a feasible option. Intralesional radiofrequency ablation being a minimally invasive procedure with a good safety profile,4 gave desirable results without afflicting much pain to the patient in smaller lesions. For the sessile, larger lesions the use of bipolar mode helped in bloodless ablation of the lesions. Not only the use of a bipolar probe help in quick resection, but also causes less collateral damage due to the flow of energy being confined between the two poles of the probe.5
LEARNING POINTS
Surgical excision, although considered a gold standard treatment modality, is not a feasible option for widespread lesions of cutaneous leiomyoma.
Intralesional radiofrequency ablation with a monopolar probe can be done for smaller leiomyoma lesions.
Larger-sized lesions of cutaneous leiomyoma may have a tendency to recur.
Radiofrequency ablation with a bipolar probe can be done for larger lesions.
Radiofrequency ablation is a simple, less time-consuming procedure that can be done in resource- poor settings for the treatment of cutaneous leiomyoma without long-term recurrence.
CONCLUSION
Radiofrequency ablation is a simple, effective, less time-consuming procedure with minimal blood loss and acceptable cosmetic outcome which can be done in resource-poor settings for the treatment of cutaneous leiomyoma without long-term recurrence
Authors’ Contributions
All the authors equally contributed to the research study. Shivani Bansal: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review. Sushama Sushama: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review. Arwinder Kaur Brar: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review. Manjit Kaur Rana: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Leiomyoma cutis: A focused review on presentation, management, and association with malignancy. Am J Clin Dermatol. 2015;16:35-46.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous smooth muscle neoplasms: Clinical features, histologic findings, and treatment options. J Am Acad Dermatol. 2002;46:477-90.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of multiple cutaneous leiomyomas with CO2 laser ablation. Dermatol Surg. 2000;26:319-22.
- [CrossRef] [PubMed] [Google Scholar]
- Intralesional radiofrequency ablation for nodular angiolymphoid hyperplasia on forehead: A minimally invasive approach. Indian J Dermatol Venereol Leprol. 2014;80:419-21.
- [CrossRef] [PubMed] [Google Scholar]
- Monopolar electrosurgical tunnelling combined with bipolar coagulation for bloodless resection of benign sessile skin lesions. J Am Acad Dermatol. 2021;85:e5-6.
- [CrossRef] [PubMed] [Google Scholar]






