Translate this page into:
Uses of Tangential Lighting for Skin Examination: A Clinical Pearl
Address for correspondence: Dr. Muhammed Mukhtar, Mukhtar Skin Centre, Katihar Medical College Road, Katihar 854105, Bihar, India. E-mail:drmmukhtar20@gmail.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Dear Editor,
Many small superficial skin and hair lesions, such as fine and gray hair of alopecia areata, vesiculo-papules of eruptive syringoma, and mini vesiculo-pustules on tinea incognito margins are not properly visible in the clinic light. Their examinations, however, are critical for better diagnosis, prognosis, treatment, and follow-up. Side (tangential) lighting has been used to improve visualization of leukotrichia (a poor prognostic factor) on vitiliginous skin,[1] identification of biopsy sites,[2] epilumiscence microscopy evaluation of pigmented lesions,[3] examination of white dysplastic melanocytic naevi,[4] and cellulite photography.[5] In this study, we proposed routinely the use of direct/tangential lighting for the visualization and diagnosis of fine, small, and whitish, hypopigmented lesions or structures on the skin’s surface.
Tangential lighting is direct light that is focused at a very low angle on the skin’s surface. To inspect superficial, small lesions or structures of skin and their appendages on the skin’s surface, a pencil torch, a general torch, or even a mobile light can be used. The distance between the light source and the lesion is determined by the angle of projection, size, and power of the torch or light source. The torch should be kept at a distance of 2 to 4 inches in general, and it can be adjusted during the examination depending upon size and intensity of light source. The angle of projection should be the primary focus. Tangential light, when focused on the relatively flat skin surface, highlights the extremely fine, small, and hypopigmented lesions and structures by producing larger dark shadows that are easily visible to the naked eye. In tangential lighting, there is no need to turn off the room light for skin inspection. Dermoscopy can easily reveal these lesions. In a busy clinic, however, performing dermoscopy on each and every patient is both impossible and time-consuming. Dermoscopy should be performed in cases of confusion to better inspect the morphology of the lesions. Furthermore, when inspecting the skin and hair under tangential lighting, light reflection is negligible, and as a result, visualization of the structure is superior to room light within the clinic [Figure 1,Figure 2,Figure 3]. Thus, using tangential light to examine skin lesions on a regular basis may be a good idea for better and faster diagnosis of skin and hair lesions.

- Scalp surface and fine hair grown of alopecia areata of scalp hair in room and tangential lighting
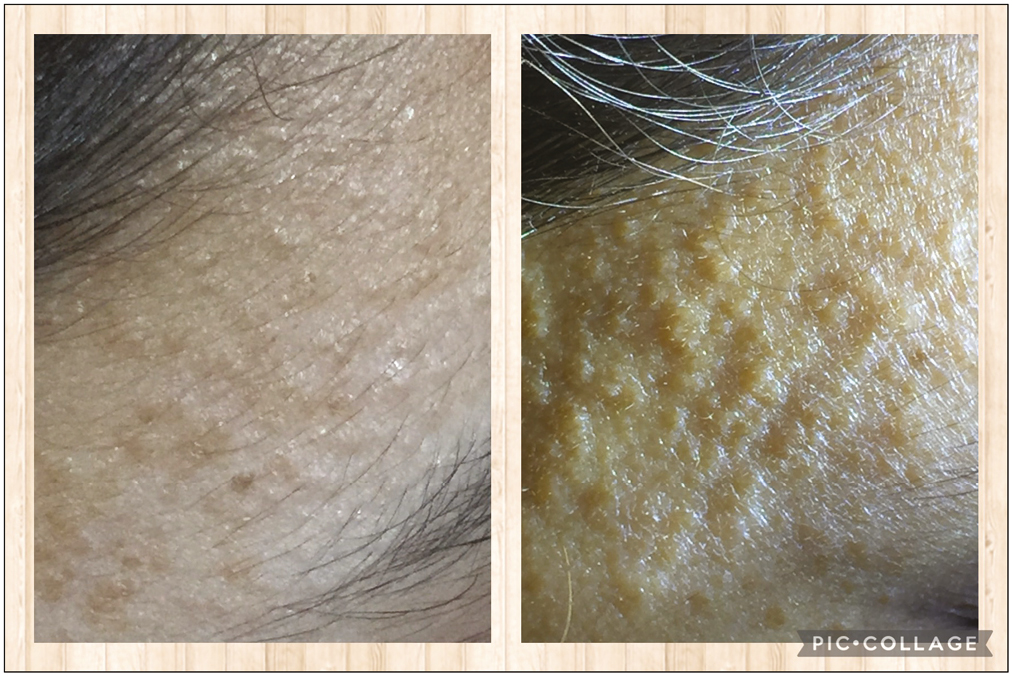
- Surface of eruptive syringoma over face in room and tangential lighting
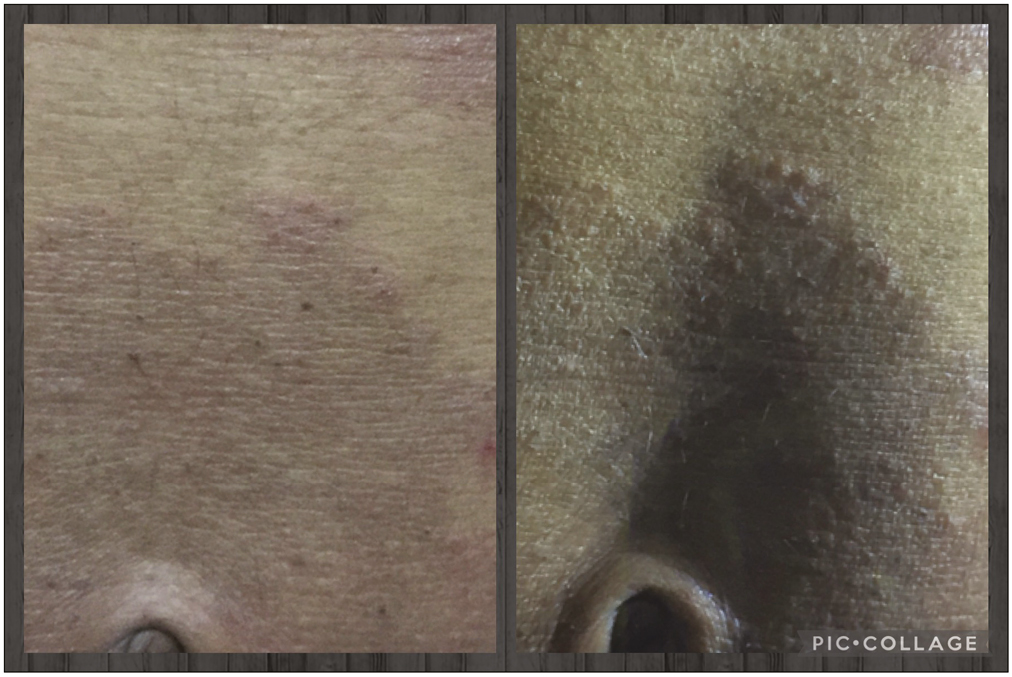
- Margins of tinea incognito over abdomen in room and tangential lighting
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support
Not applicable.
Conflict of interest
There are no conflicts of interest.
REFERENCES
- Side lighting to enhance the visualization of leukotrichia in vitiligo. 2022. J Am Acad Dermatol. doi: 10.1016/j.jaad.2022.02.058
- [Google Scholar]
- Tangential lighting aids in the identification of biopsy sites. Dermatol Surg. 2011;37:292-3.
- [Google Scholar]
- Digital epiluminescence microscopy in the evaluation of pigmented lesions: A brief review. Semin Surg Oncol. 1993;9:198-201.
- [Google Scholar]
- A two-center, double-blinded, randomized trial testing the tolerability and efficacy of a novel therapeutic agent for cellulite reduction. J Cosmet Dermatol. 2005;4:93-102.
- [Google Scholar]





