Translate this page into:
Vulvar and vaginal anatomical variations in Indian women – A cross-sectional study
*Corresponding author: Mishu Mangla, Department of Obstetrics and Gynecology, All India Institute of Medical Sciences, Bibinagar, Hyderabad, India. mishusingla83@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mangla M, Garg P, Yoga Purini P, Paul S, Kaur H, Rathod SR, et al. Vulvar and vaginal anatomical variations in Indian women – A cross-sectional study. J Cutan Aesthet Surg. doi: 10.25259/ jcas_41_24
Abstract
Objectives:
The appearance and morphology of the vulva are dependent on race, ethnicity, age, hormonal status, parity, and body mass index (BMI). The present study was planned to obtain a nomogram of vulva and vagina measurement in the Indian population and to find the correlation between the measurements of female external genitalia with various demographic parameters.
Material and Methods:
This multi-centric and cross-sectional study included the recruitment of 1562 women from across four different tertiary care centers in India. Genital measurements were taken in the lithotomy position. Measurements were recorded as mean ± SD and centiles for age and BMI were prepared. The correlation of genital measurements with age, height, weight, BMI, parity, and the frequency of sexual intercourse was studied with the help of Spearman’s rank correlation coefficient.
Results:
The mean length and width of labia majora are 9.7 ± 1.8 cm and 3.7 ± 0.8 cm, respectively. Labia minora measures 5.7 ± 1.5 cm in length and 1.9 ± 0.7 cm in width. The mean length of the clitoris is 13.2 ± 4.5 mm and the mean width is 7.7 ± 3.1 mm. The perineal body measures 2.5 ± 0.7 cm. The average total vaginal length is 8.9 ± 1.4 cm. Most of the female external genital measurements, except the clitoris, showed a positive correlation with the BMI (P < 0.05).
Conclusion:
The nomograms presented in the study can be used as a reference range for counseling women undergoing surgery on external genitalia, including cosmetic gynecology surgeries, to guide them about normality and expected outcomes following surgery. The centile curves can be used as reference ranges for women of different ages and BMI.
Keywords
Genital measurements
Vulva and vagina
Genital anatomy
Anatomical nomogram
INTRODUCTION
Female external genitalia, also referred to as the “Vulva” comprises the mons pubis, labia majora, labia minora, clitoris, urethra, vulva vestibule, vestibular bulbs, Bartholin’s glands, Skene’s glands, vaginal opening.1,2 Although the functions, blood and nerve supply, and even the histological anatomy of all these, are well documented in anatomy textbooks, the normal morphology of the vulva is still a matter of debate, as most of the medical textbooks lack data regarding the normal measurements of the vulva.3 The appearance of female external genitalia is dependent on several factors such as race, ethnicity, age, hormonal status, parity, and body mass index (BMI). Ultrasound studies, also, have shown significant differences between the pelvic organs of white and black females.4 Most of the literature on this is available from the Caucasian population and there is a paucity of data from Asian women.
Nomograms for measurements are currently not available. Accurate knowledge of anatomical measurements of the female external genitalia, including the vulva and vagina, is required for a variety of reasons. First, it is needed for designing and shaping medical and surgical equipment such as speculum, douche, intrauterine devices, uterine sound, endometrial biopsy curette, vaginal dilators, vacuum-assisted delivery devices, catheters, menstruation products, and vaginal retractors,3 required for examination and surgical procedures. Second, some surgical procedures require the removal or shortening of a part of the external genitalia. Accurate and reproducible knowledge regarding normality, too would be beneficial to the operating surgeon in counseling the patients regarding what to expect as the outcome in the postoperative period. Third, there has been a rising concern regarding the appearance of external genitalia in recent years, as evident by a rising number of consultations in the field of cosmetic gynecology.5,6
At present, the most extensive and best data set available surveyed 657 white women aged 15–84.7 This data set is by far the best available resource due to its large sample size and the variety of measurements collected. However, the raw data from this study was not published, so the measurements and distributions could not be stratified by someone without direct access to the study’s results. Another limitation to the utility of the data collected, as acknowledged by the paper, is that the study population was ethnically and geographically homogeneous. Accurate data regarding the dimensions of the vulva and vagina are required for the Indian subset of the population as, at present, we rely predominantly on data from Western countries. The present study was, therefore, planned with the objective of preparation of nomogram regarding measurements of the vulva and vagina in the Indian population and to find the correlation between the measurements of female external genitalia in our population and their BMI, age, parity, and frequency of sexual intercourse.
MATERIAL AND METHODS
This multi-centric and cross-sectional observation study was carried out in the department of obstetrics and gynecology in four tertiary care institutes in India over a period of 1 year from July 2022 to July 2023. All India Institute of Medical Sciences (AIIMS), Bibinagar, Hyderabad (South India), AIIMS Mangalagiri (South India), AIIMS Kalyani (East India), and AIIMS Bathinda (North India) were the participating sites. The Institute Ethical Committee approval was sought at all the institutes. Women were recruited from the outpatient department of obstetrics and gynecology by opportunistic screening. All participants were explained in detail regarding the protocol of examination and written informed consent was taken from each of the study participants.
The sample size was calculated using OpenEpi, Version 3, an open-source calculator. For calculating the sample size, it was assumed that there is a population of individuals where some proportion, p, has the normal measurements of external genitalia which is widely different from the normal population. Thus, to estimate p in the population, a sample of n individuals could be taken from the population, and the sample proportion, p̂, calculated for sampled individuals who have grossly different normal measurements. Since the population proportion is unknown, it was taken to be 50%.
At 95% confidence intervals and a margin of error of 5%, the sample size came out to be 384 for each center. (At P = 50%, CI = 95%, margin error 5%, n comes out to be 384). Therefore, it was planned to include at least 384 women from each center by convenient sampling.
All the patients attending the gynecology outpatient department (OPD) for various reasons were explained to participate in the study, and their written informed consent was taken. Women not willing to participate in the study, age <18 years, women with any history suggestive of surgery or radiotherapy in the genital region that could modify the normal measurements of the external genitalia, women with genital prolapse, chronic vulval disease, and women with congenital malformation of the external genitalia and lower reproductive tract were excluded from the study.
A semi-structured pro forma was used to collect information regarding age, occupation, education status, parity, and frequency of coitus. A record was made of their height, weight, and BMI. Genital measurements were taken in the lithotomy position. External genital measurements were done using a reusable metal caliper with graduations, which could measure to 1/10 mm by the gynecologists. The principal investigator ensured standardization of the measurements by supervising the first 10 measurements done by each of the co-investigators. The measurements following the template are shown in Table 1. Labia minora and majora length and width were measured bilaterally and a mean value of the two was taken for analysis.
| Parameter | Starting point | Ending point |
|---|---|---|
| Labia majora length | Skinfold at the root of the clitoris | Mucocutaneous junction |
| Labia majora width | Sulcus nympho-labialis* | Borderline without pubic hair or up to the skinfold |
| Labia minora width | Sulcus nympho-labialis* | The apex of labia minora or the widest lateral prominence. |
| Labia minora length | Clitoral glans | The junction of the skin and mucosa |
| Clitoral glans width | The greatest transverse diameter of the clitoral glans | - |
| Clitoral glans length | Longest craniocaudal length of the clitoral glans after retracting the prepuce. | - |
| Clitoral prepuce length | Length of the skin fold on the clitoris | - |
| Clitoris to urethra | The mid-clitoral glans | 12 o’clock point on the urethral orifice |
| Perineal body length | The mucocutaneous junction at the posterior fourchette. | The mid-anal orifice |
Statistical analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) version 15.0 software (SPSS Inc., Chicago, IL, USA). Continuous variables are presented as mean values, standard deviations, median, and interquartile range, while the qualitative ones are by their frequency and percentage. Determination of the normality of the distribution of continuous variables was performed by the Shapiro–Wilk test. If the distribution of continuous data was normal, a comparison of arithmetic means of two independent samples was performed by Student’s t-test for independent samples, and if it was not, the Mann–Whitney U-test was performed. Comparison of absolute frequencies of categorical variables was performed by the Chi-square test and its variants concerning the size of samples. The correlation between age, height, weight, BMI, parity, and the frequency of sexual intercourse was studied with the help of Spearman’s rank correlation coefficient.
RESULTS
A total of 1562 women were recruited from all the study sites (439 from AIIMS Mangalagiri, 493 from AIIMS Bathinda, 390 from AIIMS Bibinagar, and 250 from AIIMS Kalyani). The diagnosis of the patients (for which they visited gynecology outpatient department) included in the present study included abnormal uterine bleeding (61.65%), white discharge per vaginum (23.49%), women visiting for routine cervical cancer screening (6.14%), infertility (including both primary and secondary) (4.8%), hirsutism, or breast complications such as lump, nipple discharge, or galactorrhea (2.56%). We also included 20 (1.3%) patients, who visited OPD for consultation only, as they were asymptomatic patients with incidentally diagnosed conditions on ultrasound, such as fibroid and simple ovarian cysts [Supplementary Table 1].
The baseline characteristics of the study population are listed in Table 2. About 10.7 % of the study population was nulliparous, 21.3% primiparous, and the remaining 70% was multiparous. More than 98% denied any tampon use during menstruation.
| Baseline characteristic | No. of cases | Percentage |
|---|---|---|
| Age group | ||
| <25 | 115 | 7.4 |
| 25–35 | 537 | 34.4 |
| 35–45 | 618 | 39.6 |
| 45–55 | 230 | 14.7 |
| >55 | 62 | 4.0 |
| BMI group | ||
| <18.5 | 93 | 6.0 |
| 18.5–22.9 | 423 | 27.1 |
| 23–24.9 | 228 | 14.6 |
| >25 | 818 | 52.4 |
| Education level | ||
| Illiterate | 359 | 23 |
| Primary | 257 | 16.5 |
| Secondary/Sen-secondary | 630 | 40.33 |
| Graduate/post-graduate | 316 | 20.23 |
| Parity | ||
| P0 | 167 | 10.7 |
| P1 | 333 | 21.3 |
| P2 | 781 | 50.0 |
| P3 | 223 | 14.3 |
| P4 or higher | 58 | 3.7 |
| Using Vaginal Tampon during menstruation | ||
| No | 1537 | 98.4 |
| Yes | 25 | 1.6 |
| Type of delivery | ||
| Both Cesarean and Vaginal deliveries | 70 | 4.5 |
| Cesarean delivery only | 500 | 32.0 |
| None | 167 | 10.7 |
| Vaginal delivery only | 825 | 52.8 |
| Number of vaginal deliveries | ||
| One | 210 | 13.4 |
| Two | 480 | 30.7 |
| Three | 164 | 10.5 |
| Four | 36 | 2.3 |
| Five or more | 13 | 0.8 |
| None | 659 | 42.2 |
BMI: Body mass index
Table 3 lists the average external genital measurements of the study population and the normative data regarding the 5th, 25th, 50th, 75th, and 95th centiles. Reference nomograms for the study population are depicted in Figure 1. Reference nomograms for women ethnic to the southern, northern, and eastern parts of India were analyzed separately to compare regional variations and are mentioned in the supplementary material [Supplementary Tables 2-4 and Supplementary Figure 1].
| Mean±SD | Centiles | |||||
|---|---|---|---|---|---|---|
| 5th | 25th | 50th | 75th | 95th | ||
| Labia majora length (Right) in cm | 9.7±1.8 | 7.0 | 8.5 | 9.5 | 11.0 | 13.0 |
| Labia majora length (Left) in cm | 9.7±1.8 | 7.0 | 8.5 | 9.5 | 11.0 | 13.0 |
| Labia majora width (Right) in cm | 3.7±0.8 | 2.2 | 3.0 | 3.8 | 4.0 | 5.0 |
| Labia majora width (Left) in cm | 3.7±0.9 | 2.2 | 3.0 | 3.8 | 4.0 | 5.0 |
| Labia minora length in cm (Right) | 5.7±1.5 | 3.4 | 4.5 | 5.8 | 7.0 | 8.0 |
| Labia minora length in cm (Left) | 5.7±1.5 | 3.4 | 4.5 | 5.8 | 7.0 | 8.0 |
| Labia minora width in cm (Right) | 1.9±1.5 | 1.0 | 1.5 | 2.0 | 2.5 | 3.0 |
| Labia minora width in cm (Left) | 1.9±0.7 | 1.0 | 1.5 | 2.0 | 2.4 | 3.0 |
| Clitoris length (In mm) | 13.2±4.5 | 8.0 | 10.0 | 12.0 | 15.0 | 22.0 |
| Clitoris width (In mm). | 7.7±3.1 | 3.0 | 5.0 | 8.0 | 10.0 | 12.0 |
| Length of introitus in cm | 2.8±1.5 | 1.0 | 1.5 | 2.5 | 4.0 | 5.5 |
| Length of the perineal body in cm | 2.5±0.7 | 1.5 | 2.0 | 2.5 | 3.0 | 4.0 |
| Clitoris to urethral length in mm. | 23.3±7.4 | 10.0 | 20.0 | 23.0 | 30.0 | 35.0 |
| Urethra to vagina length in mm | 18.0±9.0 | 5.0 | 10.0 | 18.0 | 22.0 | 35.0 |
| Total vaginal length in cm. (only for married or sexually active females) | 8.9±1.4 | 7.0 | 8.0 | 9.0 | 10.0 | 11.2 |
SD: Standard deviation
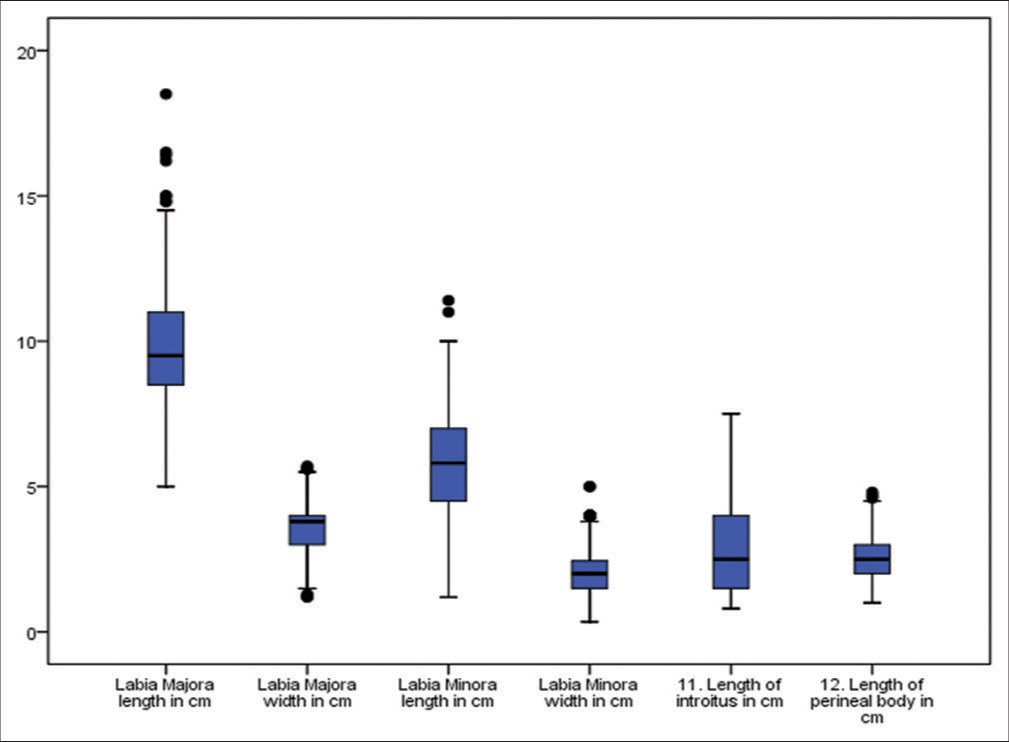
- Reference nomograms of anatomical measurements of Vulva the study population.
The Spearman correlation coefficient for various genital measurements and demographic characteristics of the study population are presented in Table 4. Most of the female external genital measurements, except the clitoris, showed a positive correlation with the BMI (P < 0.05). Apart from clitoris to urethra length and urethra to vagina length, the only genital measurements that showed a significant positive correlation with parity were labia majora length, length of introitus, and total vaginal length. The reference nomograms of anatomical measurements of Vulva in the study population, with respect to parity, are given in Supplementary Table 5.
| Correlations | Spearman’s | Labia Majora length in cm | Labia Majora width in cm | Labia Minora length in cm | Labia Minora width in cm | Clitoris length (In mm) | Clitoris width (In mm). | Length of introitus in cm | Length of perineal body in cm | Clitoris to urethra length in mm. | Urethra to vagina length in mm | Total vaginal length in cm. (only for married or sexually active females) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | Correlation coefficient | 0.066 | 0.088 | 0.204 | 0.073 | 0.050 | −0.026 | 0.123 | 0.088 | 0.030 | 0.012 | −0.026 |
| P-value | 0.009 | 0.001 | 0.001 | 0.004 | 0.049 | 0.306 | 0.000 | 0.000 | 0.236 | 0.639 | 0.302 | |
| BMI | Correlation coefficient | 0.056 | 0.133 | 0.189 | 0.166 | −0.054 | −0.139 | −0.078 | 0.272 | 0.114 | 0.145 | −0.036 |
| P-value | 0.026 | 0.001 | 0.001 | 0.001 | 0.033 | 0.001 | 0.002 | 0.001 | 0.001 | 0.001 | 0.154 | |
| Height in cm | Correlation coefficient | 0.130 | 0.107 | 0.112 | −0.037 | 0.093 | 0.099 | 0.249 | −0.056 | 0.045 | −0.087 | 0.065 |
| P-value | 0.001 | 0.001 | 0.001 | 0.143 | 0.001 | 0.001 | 0.001 | 0.027 | 0.072 | 0.001 | 0.011 | |
| Weight | Correlation coefficient | 0.117 | 0.184 | 0.242 | 0.157 | −0.012 | −0.089 | 0.019 | 0.261 | 0.145 | 0.118 | −0.002 |
| P-value | 0.001 | 0.001 | 0.001 | 0.001 | 0.638 | 0.001 | 0.463 | 0.001 | 0.001 | 0.001 | 0.940 | |
| Parity | Correlation coefficient | 0.115 | 0.037 | 0.030 | 0.005 | 0.008 | 0.046 | 0.101 | −0.018 | 0.071 | 0.138 | 0.063 |
| P-value | 0.001 | 0.140 | 0.238 | 0.835 | 0.760 | 0.069 | 0.001 | 0.470 | 0.005 | 0.001 | 0.013 | |
| Number of vaginal deliveries | Correlation coefficient | 0.075 | 0.069 | 0.180 | 0.038 | 0.046 | 0.037 | 0.248 | 0.001 | 0.066 | 0.074 | 0.003 |
| P-value | 0.003 | 0.006 | 0.001 | 0.134 | 0.068 | 0.141 | 0.001 | 0.975 | 0.009 | 0.003 | 0.916 |
BMI: Body mass index
DISCUSSION
The demand for female cosmetic gynecological procedures has been increasing day by day. According to American Esthetic Plastic Surgery National Data bank 2020, the total revenue for female genital cosmetic surgery was over nine billion dollars despite the coronavirus pandemic when surgical procedures were restricted for mainly emergencies. A total of 13,697 labiaplasties were performed during this time.8 This number demonstrates an increase compared to 12,903 and 9945 labiaplasties completed in 2019 and 2015, respectively. A study conducted in India also revealed a significant increase in the demand for esthetic vaginal procedures, rising from 3.9% in 2012 to 28.97% in 2015.9,10 However, it is important to understand that these numbers may be misleading and an actual underestimate because women seeking surgeries at private centers may not be reported. It is important to have a well-informed decision for cosmetic surgery considering the pros and cons of the procedure. Genital or cosmetic gynecological surgery risks disruption of nerves and blood vessels of the perineal region, which may later impair sensation in the genital area and even affect the future capacity for sexual pleasure.11,12 Female genital cosmetic surgery should only be undertaken with a clear understanding of the variation in normal appearance and in cases that differ markedly from the average. It is also important to rule out other psychological disorders in women seeking female genital cosmetic surgery. An article published by Veale et al. in 2014 reported a significantly greater frequency of avoidance, safety-seeking behaviors, and a high incidence of body dysmorphic disorder in these women.13
In general, the goals of genital cosmetic surgery14 are a symmetrical labia minora that do not protrude beyond the labia majora in the standing position, a clitoral hood with few folds, short and not protruding, and full labia majora such that they are not excessively fat and without excess lax skin and a close-fitting vagina with improved vaginal sensations during sexual intercourse.15 Labia minora hypertrophy has been variably defined as maximal labial width exceeding 5 cm4 4 cm5 or 3 cm6 and more recently, even 2 cm has been proposed by some cosmetic surgeons because it is at this point that “the inner vaginal lips generally start to be visible outside the shelter of the labia majora.”16 It is important to note that these goals of surgery are all subjective and the image of “an ideal vulva” would, therefore, vary from one patient to another and even from one doctor to another. There are very few studies in the literature that provide normative data regarding genital measurements. The authors have tried to compile these normal female external genital measurements published in the past few years [Table 4]. Before this study, the largest study was published by Kreklau et al. on 657 women.7 The major limitation of this study was that the population they studied was homogenous.
The present study is probably the first multi-centric study with a large sample size to publish the average measurements of labia majora and labia minora in the Indian population. There is another study for the north Indian population.17 where authors studied anatomical measurements of genitalia. These data are fundamental because racial and ethnic factors significantly impact the measurements of the vulva and vagina for a given population sample. These data will be instrumental in counseling the patients seeking medical advice for ‘abnormal Vulva’ or ‘Vulval abnormalities’. Practicing gynecologists can use this as a reference range to guide women and young girls regarding normality. Further, many patients also have concerns about whether the outcome was esthetically favorable after any surgical procedures on the vulva, such as labial cyst excision or simple or radical vulvectomy. Normative datasets are also helpful when planning reconstructive or transgender surgery. The authors have also attempted to compare the normal anatomical measurements of the Indian population with global data by comparing the results of the present study with those of the previously published ones [Table 5].18-22 We found that although most of the measurements are comparable, there was a significant difference in the dimensions of the clitoris glans. The mean length and width of the glans clitoris were 6.89 ± 4.96 mm and 4.62 ± 2.53 mm for the white women; the respective mean measurements for the Indian population were 13.2 ± 4.5 mm and 7.7 ± 3.1 mm, respectively. Ethnic variations can be a reason, but before making any definite conclusions regarding this significant ethnic variability, we have to keep in mind that this could be due to inter-observer variability as, till now, there is no standardized technique or measuring instrument that can rule out this bias.
| The present study | Kreklau et al., 20187 | Agarwal et al. 202217 | Widschwendter et al. 201918 | Krissi et al. 201519 | Lloyd et al. 200520 | Basaran et al. 200821 | Cao et al. 201422 | |
|---|---|---|---|---|---|---|---|---|
| Study population | Women ≥18 years | White women aged 15–84 years | Indian Women aged >18 years | 18–50 years | premenopausal women aged 20–51 years | Pre-menopausal women aged ≥18 years | 50 premenopausal and 50 post -menopausal | 18 to 64 years Chinese women |
| Sample size | 1562 | 657 | 400 | 200 | 32 | 50 | 100 | 319 |
| Measuring device used | Metallic measuring scale | Disposable paper measure | Disposable surgical ruler | - | Disposable tape measure | Disposable tape measure | - | - |
| Labia majora length | 9.7±1.8 cm | Left- 79.99±15.44 mmRight-79.71±15.25 | 7.6±1.04 cm | 9.3 [1.3] cm | 87.4±13.4 | 75.71±5.216 | ||
| Labia majora width | 3.7±0.8 cm | 1.4±0.52 cm | - | 20.53±4.108 | ||||
| Labia minora width | 1.9±0.7 cm | Left- 14.15±7.64 mmRight – 13.4±7.87 mm | 2.6±0.74 cm | Median -19.0 mm (interquartile range (12.6–27.5) | Right –1.49±1.03 cmLeft1.45±0.87 cm | 21.8 [9.4] | 17.9±4.1 | Left - 19.92±8.462Right - 21.26±8.709 |
| Labia minora length | 5.7±1.5 cm | Left – 42.97±16.29 mmRight – 42.1±16.35 mm | 4.8±1.03 cm | median 35.5 mm (interquartile range (27.8–48.9). | Right – 3.47±1.42Left – 3.82±1.33 | 60.6 [17.2] | 55.7±11.9 | 47.99±5.821 |
| Clitoral glans width | 7.7±3.1 mm | 4.62±2.53 mm | 3.1±0.74 mm | 0.39±0.17 cm | 5.5 [1.7] | 10.2±5.2 | 4.14±1.222 | |
| Clitoral glans length | 13.2±4.5 mm | 6.89±4.96 mm | 5.2±1.43 mm | 1.13±0.67 cm | 19.1 [8.7] | 17.7±10.6 mm | 5.04±1.742 | |
| Clitoral prepuce length | - | - | - | - | 25.66±4.415 | |||
| Clitoris to urethra | 23.3±7.4 mm | 22.63±7.66 mm | 2.1±0.57 cm | 3.17±0.98 cm | 28.5 [7.1] | 29.2±8.0 | 24.95±4.366 | |
| Perineal body length | 2.5±0.7 cm | 2.3±0.60 cm | 31.3 [8.5] | 30.1±9.9 | 24.56±4.203 | |||
| Vagina to perineum | - | 13.82±2.286 | ||||||
| Vaginal length | 8.9±1.4 cm | 9.44±1.33 cm | 9.6 [1.5] | 90.3±14.8 | ||||
| Length of Introitus | 1.3±0.59 cm | - |
This is by far the largest data set, with a sample size of 1562, published to date on the normal anatomical measurements of the vulva. The female external genital measurements have varied widely across the study population. This might be because this multicentric study included women from three different geographic regions of India and each region is expected to have a population of different ethnicity, culture, and religion. The range for all the measurements is significantly large, again highlighting the fact that perception of normality is varied. Lloyd et al.20 and Krissi.19 also confirmed in their studies that these measurements are highly variable, but they did not find any significant variation in dimensions with changing age, parity, ethnicity, and history of sexual activity. In their meta-analysis, Hayes and Temple-Smith23 concluded that there are sufficient studies on dimensions of labia minora, and it can be added to medical texts so that clinicians understand the physiologic diversity from the graduation period.24 They concluded that the length of labia majora ranges from 5 to 100 mm, while the width ranges from 1 to 60 mm, and these can safely be used as standard.
Study limitations
Although the present study is the first multi-centric study to provide a large database for the Indian population, it had certain limitations. The results from this study cannot be applied to the whole Indian population as the sample size is small, and the sampling technique is not designed to apply to the entire population. This is a hospital-based study, where only patients visiting the gynecology outpatient department due to any gynecological complaint were included for data collection. Studies with larger sample sizes in the community with structured tools assessing the actual perceptions of women, their external genitalia, and their corresponding measurements can be helpful in the future.
CONCLUSION
The nomograms presented in the study can be used as a reference range for counseling women undergoing any surgery on external genitalia, including cosmetic gynecology surgeries. Knowing normal anatomical variations of external genitalia might be helpful in counseling women regarding their expectations of normality and surgical outcomes. The centile curves can be used as reference ranges for women with different ages and BMI.
Acknowledgment
The authors wish to thank Miss Arshia Singla, for her valuable support in preparation of images for this article.
Authors’ contributions
Mishu Mangla: Concept, design, data collection or processing, analysis or interpretation, literature search, writing, review and approval to the final version of the manuscript. Priyanka Garg: Design, data collection or processing, analysis or interpretation, literature search. writing, review and approval to the final version of the manuscript. Priyanka Yoga Purini: Design, data collection or processing, analysis or interpretation, literature search, writing, review and approval to the final version of the manuscript. Sayanti Paul: Design, data collection or processing, analysis or interpretation, literature search, writing, review and approval to the final version of the manuscript. Harpreet Kaur: Analysis or interpretation, literature search, writing, review and approval to the final version of the manuscript. Sandhya Rani Rathod: Data Collection or Processing, review and approval to the final version of the manuscript. Poojitha Kanikaram: Data Collection or Processing, review and approval to the final version of the manuscript. Sevala Kavya Sree: Data Collection or Processing, review and approval to the final version of the manuscript. Aparna Jarathi: Data Collection or Processing, review and approval to the final version of the manuscript. Nabnita Patnaik: Data Collection or Processing, review and approval to the final version of the manuscript. Sharmila Vijayan: Data Collection or Processing, review and approval to the final version of the manuscript.
Ethical approval
The research/study was done after due approval from the institutional ethics committee of all of the four participating institutes, (AIIMS Bibinagar vide letter no AIIMS/BBN/ IEC/DEC/2021/136 amended dated 09/04/2022; AIIMS Bathinda vide letter number IEC/AIIMS/BTI/300 dated 21/11/2022; AIIMS kalyani vide letter no. IEC/AIIMS/Kalyani/ Meeting/2022/55 dated22/07/2022 and AIIMS Mangalagiri vide letter no. AIIMS/MG//IEC/2022-23/220 dated 28/11/2022.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Anatomy, abdomen and pelvis: Female external genitalia In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK547703 [Last accessed on 2024 May 03]
- [Google Scholar]
- Anatomy of the vulva and the female sexual response. Obstet Gynecol Clin North Am. 2016;43:27-44.
- [CrossRef] [PubMed] [Google Scholar]
- The normal vulva in medical textbooks. J Obstet Gynaecol. 2013;33:648-50.
- [CrossRef] [PubMed] [Google Scholar]
- Racial differences in female urethral morphology and levator hiatal dimensions: An ultrasound study. Neurourol Urodyn. 2012;31:502-7.
- [CrossRef] [PubMed] [Google Scholar]
- Women's perception of their vulvar appearance in a predominantly low-income, minority population. Female Pelvic Med Reconstr Surg. 2017;23:417-9.
- [CrossRef] [PubMed] [Google Scholar]
- Interest in cosmetic vulvar surgery and perception of vulvar appearance. Am J Obstet Gynecol. 2012;207:428.e1-7.
- [CrossRef] [PubMed] [Google Scholar]
- Measurements of a “normal vulva” in women aged 15-84: A cross-sectional prospective single-centre study. BJOG. 2018;125:1656-61.
- [CrossRef] [PubMed] [Google Scholar]
- Aesthetic plastic surgery national databank statistics 2020. Available from: https://cdn.surgery.org/media/statistics/aestheticplasticsurgerynationaldatabank-2020stats.pdf [Last accessed on 2021 Jul 21]
- [Google Scholar]
- Audit of female genital aesthetic surgery: Changing trends in India. J Obstet Gynaecol India. 2018;68:214-20.
- [CrossRef] [PubMed] [Google Scholar]
- Cosmetic gynecology-An emerging field for the dermatologist. J Cosmet Dermatol. 2023;22:111-8.
- [CrossRef] [PubMed] [Google Scholar]
- Should we encourage exclusive breastfeeding at all cost. ? Lancet. 2003;362:247-8.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of clitoral surgery on sexual outcome in individuals who have intersex conditions with ambiguous genitalia: A cross-sectional study. Lancet. 2003;361:1252-7.
- [CrossRef] [PubMed] [Google Scholar]
- Psychological characteristics and motivation of women seeking labiaplasty. Psychol Med. 2014;44:555-66.
- [CrossRef] [PubMed] [Google Scholar]
- Female aesthetic genital surgery In: Nahai F, ed. The art of aesthetic surgery-principles and techniques (2nd ed). St. Louis: Quality Medical Publishing Inc; 2011. p. :3097-124.
- [Google Scholar]
- An acquired sensation of wide/smooth vagina: A new classification. Eur J Obstet Gynecol Reprod Biol. 2011;158:97-100.
- [CrossRef] [PubMed] [Google Scholar]
- The anatomical measurements of vulva in Indian women: A cross-sectional prospective study. Int J Gynaecol Obstet. 2022;158:153-61.
- [CrossRef] [PubMed] [Google Scholar]
- Perception of labial size and objective measurements-is there a correlation? A cross-sectional study in a cohort not seeking labiaplasty. J Sex Med. 2020;17:461-9.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomical diversity of the female external genitalia and its association to sexual function. Eur J Obstet Gynecol. 2016;196:44-7.
- [CrossRef] [PubMed] [Google Scholar]
- Female genital appearance: “Normality” unfolds. BJOG. 2005;112:643-6.
- [CrossRef] [PubMed] [Google Scholar]
- Characteristics of external genitalia in pre-and postmenopausal women. Climacteric. 2008;11:416-21.
- [CrossRef] [PubMed] [Google Scholar]
- Measurements of female genital appearance in Chinese adults seeking genital cosmetic surgery: A preliminary report from a gynecological center. Int Urogynecol J. 2015;26:729-35.
- [CrossRef] [PubMed] [Google Scholar]
- What is the anatomical basis of labiaplasty? A review of normative datasets for female genital anatomy. Aust New Zeal J Obstet Gynaecol. 2021;61:331-8.
- [CrossRef] [PubMed] [Google Scholar]







