Translate this page into:
Extracted Hair Follicle Outer Root Sheath Cell Suspension for Pigment Cell Restoration in Vitiligo
Address for correspondence: Dr. Somesh Gupta, Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi, India. E-mail: someshgupta@hotmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Vitiligo surgery has come up a long way from punch skin grafts to epidermal cell suspension and latest to the extracted hair follicle outer root sheath cell suspension (EHF-ORS-CS) transplantation. The progressive development from one technique to the other is always in a quest for the best. In the latest development- EHF-ORS-CS, which is an enriched source of follicular inactive melanocyte (melanocyte stem cells), seems to be a good addition to the prevailing cell-based therapies for vitiligo; however, need to be explored further in larger, and preferably randomized blinded studies. This review discusses the principle, technical details, and stem cell composition of hair follicular outer root sheath cell suspension.
Keywords
Cell transplantation
EHF-ORS-CS
FUE (follicular unit extraction)
vitiligo
INTRODUCTION
Both non-surgical and surgical therapies have been employed in the management of vitiligo.[1] Surgical therapies are useful when disease is recalcitrant to medical therapies and stable for at least 1 to 2 year (s).[2] Tissue grafts can treat only a small area; therefore, cellular grafts, like basal cell layer-enriched epidermal suspension, are preferred over tissue grafts when large area is to be treated. Tissue grafting procedures include transplantation of minigrafts, thin and ultra-thin split thickness grafts (STSG), and suction blister epidermal grafts (SBEG). Cellular grafting techniques include transplantation of non-cultured basal cell-enriched epidermal suspension (NCES) and cultured melanocytes (CM) or cultured epidermis (CE).[3–8] The major advantage of non-cultured cell suspension and culture-expanded cell suspension is that they permit the treatment of the affected area many folds larger than the donor area.[9–11] However, culture techniques employed for the expansion of the cell number are time consuming, expensive, and also require trained manpower and well-equipped tissue culture laboratory. In addition, there are concerns about the safety of the techniques owing to the xenobiotic properties of some of the additives in the culture medium.[12]
These limitations of culture-expanded cells were sorted out with the introduction of the non-cultured cellular grafting techniques in 1992 by Gauthier and Surleve-Bazeille[12] and followed by several other vitiligo surgery groups. Non-cultured cell transplant can cover larger vitiliginous areas (8- to 10-fold size of donor skin), and the procedure can be completed in few hours on an outpatient basis. In summary, cultured cell transplants are technically more challenging and expensive than non-cultured epidermal cell suspension; hence, the latter provides a simple, effective, and aesthetically more suitable treatment option.[45913–19]
Non-cultured cell transplantation in vitiligo
Since the introduction of the non-cultured cell transplantation technique by Gauthier and Surleve-Bazeille[13] in 1992, the field of vitiligo surgery has progressed a lot. However, most of the surgeries done till date focus mainly on taking the skin biopsy by one or the other way and preparing the cell suspension and finally transplantation. The method of taking the skin biopsy and the processing the tissue to obtain the cell suspension is being revised rapidly to achieve a concentrated pigment cell population for transplantation.[20] As melanocytes reside in the basal layer of the skin, it is always preferred to have a cell suspension from the basal layer of the skin. Apart from the providing an enriched population of pigment cell, the basal layer also contains the skin stem cells, which further gives a practical boost to the basal layer cell enrichment method.
The culture expansion of the follicular cells has been tried in vitro.[21–23] The feasibility of follicular progenitor cell culture and differentiation into melanocytes, neuronal cells, smooth muscle cells,[24] and corneal epithelial[25] speaks about the multi-lineage differentiation potential of these cells. This indicates the competitive nature of these follicular progenitor cells in comparison with skin progenitor cells, which are more established in culture in terms of expansion, differentiation, and transplantation.[2627] Recent research outcome in this area highlights the potential of these hair follicle ORS cells in regenerative medicine.
Hair follicle melanocytes and role in vitiligo re-pigmentation
Role of hair follicle in the pigmentation of the vitiliginous lesion has been well proven in the landmark paper by Cui et al.[28] In conjunction with previous reports by Starrico,[29–31] they observed that some DOPA-negative “inactive” melanocytes (proposed to be melanocyte stem cells) were found to reside in the outer root sheath and bulge areas of the hair follicle. These melanocytes did not produce melanin under normal conditions, but became active to produce melanin when stimulated either by ultraviolet radiation or by dermabrasion. This was a landmark study, which proposed the hair follicle to be the reservoir of “inactive” melanocytes (or the so-called melanocyte stem cells). It was also observed that in vitiliginous lesions, there was destruction of only the active (DOPA-positive) melanocytes, whereas the inactive melanocytes in the ORS of the hair follicle were undamaged. These melanocytes were proposed to be responsible for re-pigmentation in vitiligo by dividing and migrating upward along the surface of hair follicle to the nearby epidermis where they continued to move radially and lead to re-pigmentation of surrounding skin as observed by Cui et al.[28] The finding that not only did melanocyte stem cells reside in hair follicles but could also, in addition, migrate to surrounding skin was another landmark observation.
These findings suggested that inactive melanocytes in the ORS of the hair follicle divide proliferate and mature during the process of re-pigmentation in the vitiligo and may be potentially harvested and cultivated for therapeutic purposes in vitiligo. The findings of the Cui et al. have been proved by several groups, and the inactive melanocytes are now taken as melanocyte stem cells.[2332–41]
Transplantation of hair follicle unit to restore pigmentation
All these developments in the knowledge pool of the hair follicle biology encouraged follicular transplant in the treatment of vitiligo. Na et al.[42] observed peri-follicular re-pigmentation around the grafted hairs within 2 to 8 weeks in 71% patients. The diameter of the spreading pigmentation ranged from 2 to 10 mm during a 12-month follow-up period. In cases of generalized vitiligo, peri-follicular pigmentation was seen in 25% patients, whereas it was 82% in patients with localized/segmental vitiligo.
The re-pigmentation has been achieved with equal frequency with established surgical methods of vitiligo surgery. The re-pigmentation process is delayed in the follicular unit transplant as compared with other surgical modalities, but the color match is much more acceptable.[42–46]
Transplantation of hair follicle ORS cell suspension
In a quest to further concentrate pigment cell population in the non-cultured cell suspension for transplantation in vitiligo, the major breakthrough came with the paper of Vaenscheidt et al.,[47] in a small case series, they have used single cell suspension of ‘plucked’ hair follicles in the treatment of vitiligo. They found almost complete (>90%) re-pigmentation in 3 of 5 patients with vitiligo, around 50% re-pigmentation in 1 patient and less than 10% re-pigmentation in 1 patient. Their technique is simple, non-invasive and allows easy, immediate, and repeated application. However, the cell yield is less in case of plucked hair follicles, and optimization of cell harvest from the hair follicular unit needs to be standardized for optimum yield.
Our group[1] has modified the method of obtaining the follicular tissue by the FUE (follicular unit extraction) method. Figure 1 shows the stepwise methodology of hair follicle ORS cell suspension preparation. We used autologous EHF-ORS-CS for transplantation in vitiligo patients. This method resulted in significant re-pigmentation in the majority of the patients [Figures 2a and b]. Three of our patients had less than 1 year of disease stability, and none of them had >75% re-pigmentation while 9 out of 11 patients with at least 1-year stability had >75% re-pigmentation.
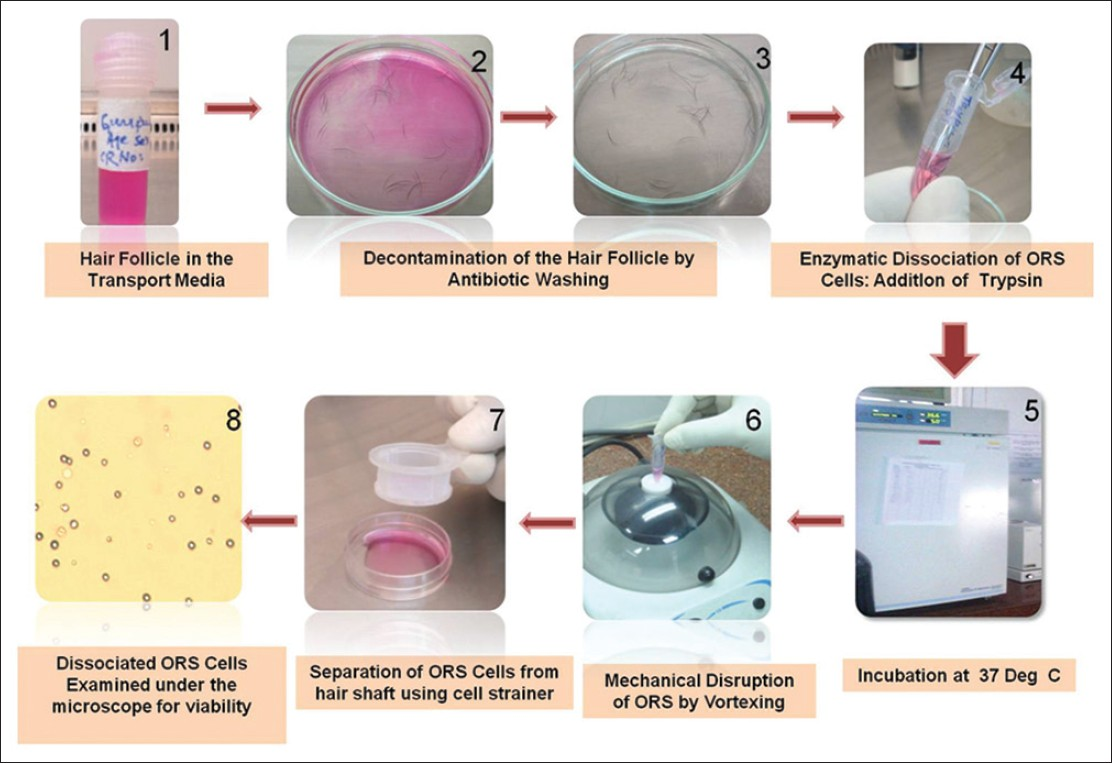
- Steps of preparation of hair follicle ors cell suspension
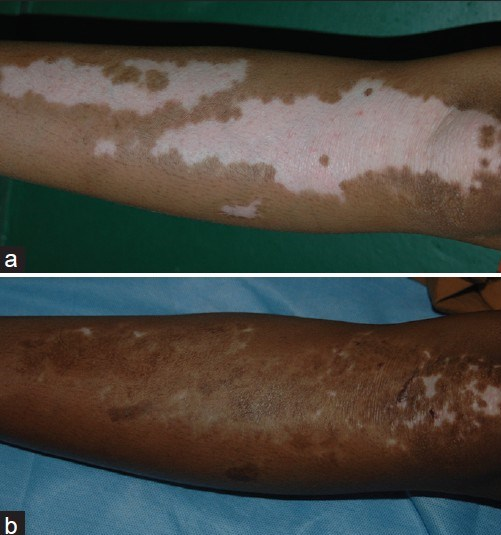
- (a) Vitiligo Patch prior to transplantation. The upper half was transplanted with multiple sessions of suction blister epidermal grafting, and the lower half was transplanted with single session of extracted follicular outer root sheath cell suspension transplantation. (b) Good re-pigmentation on both the transplanted sites
DISCUSSION
Vitiligo surgery using the hair follicle ORS cell transplant is a newer technique, needs to be explored further and employed in the treatment of stable vitiligo. Transplantation of hair follicle in vitiligo uses the scalp biopsy from occipital area in a similar way as it is being in use for strip method of hair transplantation. It leaves a visible scar on the donor site-scalp. The scalp biopsy tissue is cut into smaller pieces, each containing a single hair follicle unit. The individual hair follicle units are then transplanted onto the vitiligo patch. The resultant pigmentation of the vitiliginous area covered is again very small due to transplantation of the intact hair follicle. These two limitations of the hair transplant in vitiligo encouraged us to look for some other alternatives. As a result, we have developed hair follicle ORS cell transplant. Only two groups, as per the literature search, - Vaenscheidt et al.[47] and our group,[1] have reported this technique, so this technique is at a very nascent stage. It needs to be tried and tested by several investigators and physicians worldwide to arrive at any conclusion. In both the studies, very few cases have been done, and their follow-up time is also not very long. In addition, comparative trials need to be done to compare follicular suspension transplantation with the conventional and more widely-used technique of non-cultured epidermal suspension transplantation. Nevertheless, the initial outcome of the study suggests its significant potential in pigment cell restoration.
Vaenscheidt et al.[47] have used the plucking as a method of follicular harvest, whereas our group [1] has used the FUE method. We have used this method not by chance but by choice. We have found that the cell suspension prepared from hair follicles, obtained by FUE method, contains more CD200+ cells (a marker for hair follicle bulge stem cells) as compared to plucked hair (unpublished observation). This is further supported by the fact that transplantation of plucked hair doesn’t result in hair growth; however, transplantation of extracted follicular unit is promptly accepted by the recipient site with resulting hair growth.[2148]
We have achieved satisfactory re-pigmentation in most of our patients, indicating that the procedure is working for patients. It can be used to cover larger depigmented areas. Average number of hair follicles on scalp is 100,000, and the procedure involves removal of only a tiny proportion of it. On an average, 15–25 follicular units provide between 300,000 and 2 million cells comprising of a large number of melanocytes and heavily melanized keratinocytes, which is sufficient to treat up to 20 cm2 of recipient area.
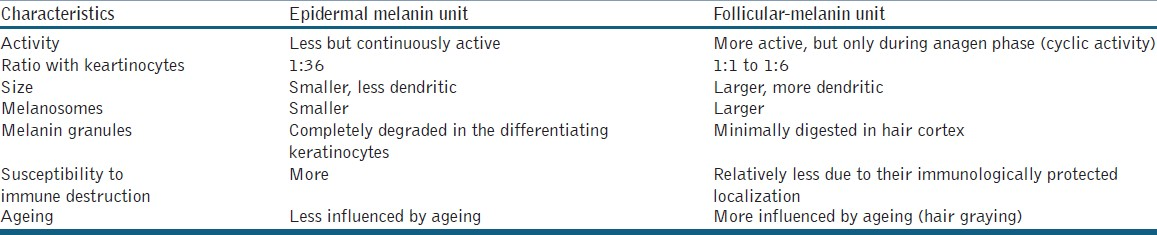
Literature search shows that as compared to epidermal cell suspension, hair follicle ORS suspension is more enriched with pigment cells. In follicular melanin unit, there is 1 melanocyte for every 5 keratinocytes in the hair bulb,[3649] which is much higher than the epidermal melanin unit, which has one melanocyte for every 36 keratinocytes. In comparison to epidermal melanocytes, anagen hair bulb melanogenic melanocytes are larger, more dendritic, with more extensive golgi and rough endoplasmic reticulum, and produce larger melanosomes.[49] Hair melanocytes have remarkable synthetic capacity, and a relatively small number of melanocytes can potentially produce sufficient melanin to pigment up to 1.5 m of hair shaft.[34] All these properties make hair melanocytes a more attractive source than epidermal melanocytes for cell-based therapies in vitiligo. Table 1 appended below is a comparison of epidermal and follicular melanin unit.[49]
There are several differences in the conventional technique of preparation of cell suspension from shave biopsy and preparation of ORS cell suspension from extracted follicular unit samples. In the conventional method, the shave biopsy from buttock is incubated in 5 ml of 0.2% w/v trypsin solution, for 45 minutes at 37°C. After this, the action of trypsin is neutralized with trypsin inhibitor, and the epidermis is separated from the dermis and transferred to a test tube containing 2 ml of Dulbecco’s Modified Eagle Medium: Nutrient Mixture F-12 (DMEMF/12) and vortex mixed for 15 seconds. The epidermis is further broken into smaller pieces and finally transferred to a test tube containing DMEM F/12 medium and centrifuged. The supernatant is discarded, and the pellet was re-suspended in a 1 ml insulin syringe.[50] The donor site on buttock heals with superficial visible scarring.
In contrast, hair follicle ORS cell suspension preparation is relatively simple, as it does not require separation of epidermis from dermis, and manual breaking of epidermal samples into small pieces. ORS cells are easily separated when incubated with trypsin. Furthermore, the tiny scars of FUE on scalp are invisible and insignificant. The procedure of FUE involves removal of much less volume of tissue in comparison to scalp biopsy (strip). The healing time is much less as compared to conventional strip method. Even donor site dressing is not required after FUE. This makes it a potential method of choice to treat large areas of stable vitiligo in a quick time. However, one limitation is that extraction of intact follicular units requires skill in order to obtain complete hair follicles while avoiding transection of the hair follicle during extraction.
In conclusion, though, this procedure can serve as a novel, minimally invasive, scar-less technique with good yield of melanocytes, melanocyte stem cells, and other stem cells (keratinocyte stem cells, and mesenchymal stem cells in the surrounding dermis and dermal papilla). It results in excellent pigmentation with no visible residual scarring of the donor area.
Epidermal stem cells isolated from hair follicles can also serve a good source for restoration of unrelated tissue such as nerves and cornea.[5152] Thus, cell suspension prepared from extracted hair follicles provides an excellent, relatively less invasive source for stem cells and/or melanocytes for vitiligo surgery.
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Non-cultured extracted hair follicle outer root sheath cell suspension for transplantation in vitiligo. Br J Dermatol. 2011;164:1241-6.
- [Google Scholar]
- Study of clinical, biochemical and immunological factors determining stability of disease in patients with generalized vitiligo undergoing melanocyte transplantation. Br J Dermatol. 2012;166:1230-6.
- [Google Scholar]
- Classification of surgical therapies for vitiligo. In: Gupta S, Olsson M, Kanwar A, Ortonne JP, eds. Surgical Management of Vitiligo. Oxford: Blackwell Publishing; 2007. p. :59-68.
- [Google Scholar]
- Modified technique of suction blistering for epidermal grafting in vitiligo. Int J Dermatol. 1999;38:306-9.
- [Google Scholar]
- Autologous melanocyte transfer via epidermal grafts for lip vitiligo. Int J Dermatol. 2006;45:747-50.
- [Google Scholar]
- Pigment cell transplantation for treatment of vitiligo: A progress report. J Am Acad Dermatol. 1994;30:591-7.
- [Google Scholar]
- Autologous cellular suspensions and sheets in the treatment of achromic disorders: The need for future controlled studies. Dermatology. 2001;202:158-61.
- [Google Scholar]
- Repigmentation of vitiligo by transplantation of cultured autologous melanocytes. Acta Derm Venereol. 1993;73:49-51.
- [Google Scholar]
- Repigmentation of vitiligo by transplantation of autologous melanocyte cells cultured on amniotic membrane. Br J Dermatol. 2008;158:1168-71.
- [Google Scholar]
- Autologous epidermal cultures and narrow-band ultraviolet B in the surgical treatment of vitiligo. Dermatol Surg. 2005;31:155-9.
- [Google Scholar]
- A review of Non-cultured epidermal cellular grafting in vitiligo. J Cutan Aesthet Surg. 2011;4:17-22.
- [Google Scholar]
- Autologous grafting with noncultured melanocytes: A simplified method for treatment of depigmented lesions. J Am Acad Dermatol. 1992;26:191-4.
- [Google Scholar]
- Suction blister epidermal grafting versus punch skin grafting in recalcitrant and stable vitiligo. Dermatol Surg. 1999;25:955-8.
- [Google Scholar]
- Comparison of melanocytes transplantation methods for the treatment of vitiligo. Dermatol Surg. 2004;30:1400-5.
- [Google Scholar]
- Transplant of cultured autologous pure melanocytes after laser-abrasion for the treatment of segmental vitiligo. J Dermatol. 2000;27:434-9.
- [Google Scholar]
- Transplantation of autologous cultured melanocytes for treatment of large segmental vitiligo. J Am Acad Dermatol. 2001;44:543-5.
- [Google Scholar]
- Inoculation of a cultured autologous epidermal suspension containing melanocytes in vitiligo. Arch Dermatol. 1993;129:785-6.
- [Google Scholar]
- Transplantation of in vitro-cultured epidermis bearing melanocytes for repigmenting vitiligo. J Am Acad Dermatol. 1989;21:257-64.
- [Google Scholar]
- Modified procedure of noncultured epidermal suspension transplantation: Changes are the core of vitiligo surgery. J Cutan Aesthet Surg. 2011;4:44-5.
- [Google Scholar]
- Human follicular stem cells: Their presence in plucked hair and follicular cell culture. Br J Dermatol. 2004;150:860-8.
- [Google Scholar]
- Bulge cells of human hair follicles: Segregation, cultivation and properties. Colloids Surf B Biointerfaces. 2006;47:50-6.
- [Google Scholar]
- Isolation and culture of amelanotic melanocytes from human hair follicles. Pigment Cell Res. 2004;17:668-73.
- [Google Scholar]
- Isolation of a novel population of multipotent adult stem cells from human hair follicles. Am J Pathol. 2006;168:1879-88.
- [Google Scholar]
- Corneal limbal microenvironment can induce transdifferentiation of hair follicle stem cells into corneal epithelial-like cells. Stem Cells. 2009;27:642-52.
- [Google Scholar]
- Cultured melanocytes: From skin biopsy to transplantation. Cell Transplant. 2008;17:351-60.
- [Google Scholar]
- A study of autologous melanocyte transfer in treatment of stable vitiligo. Indian J Dermatol Venereol Leprol. 2005;71:393-7.
- [Google Scholar]
- Role of hair follicles in the repigmentation of vitiligo. J Invest Dermatol. 1991;97:410-6.
- [Google Scholar]
- Amelanotic melanocytes in the outer sheath of the human hair follicle. J Invest Dermatol. 1959;33:295-7.
- [Google Scholar]
- Activation of the amelanotic melanocytes in the outer root sheath of the hair follicle following ultra violet rays exposure. J Invest Dermatol. 1962;39:163-4.
- [Google Scholar]
- Mechanism of migration of melanocytes from the hair follicle into the epidermis following dermabrasion. J Invest Dermatol. 1961;36:99-104.
- [Google Scholar]
- Mechanisms of hair graying: Incomplete melanocyte stem cell maintenance in the niche. Science. 2005;307:720-4.
- [Google Scholar]
- Characterization and isolation of stem cell-enriched human hair follicle bulge cells. J Clin Invest. 2006;116:249-60.
- [Google Scholar]
- The cell biology of human hair follicle pigmentation. Pigment Cell Melanoma Res. 2011;24:75-88.
- [Google Scholar]
- Distinct stem cell populations regenerate the follicle and interfollicular epidermis. Dev Cell. 2005;9:855-61.
- [Google Scholar]
- Hair follicle stem cells: Their location, role in hair cycle, and involvement in skin tumor formation. J Invest Dermatol. 1993;101:16S-26S.
- [Google Scholar]
- Melanocyte stem cells: A melanocyte reservoir in hair follicles for hair and skin pigmentation. Pigment Cell Melanoma Res. 2011;24:401-10.
- [Google Scholar]
- Dominant role of the niche in melanocyte stem-cell fate determination. Nature. 2002;416:854-60.
- [Google Scholar]
- Single hair grafting for the treatment of vitiligo. J Am Acad Dermatol. 1998;38:580-4.
- [Google Scholar]
- Repigmentation of vitiligo patches by transplantation of hair follicles. Int J Dermatol. 1999;38:237-8.
- [Google Scholar]
- Surgical treatment for vitiligo through hair follicle grafting: How to make it easy. Dermatol Surg. 2001;27:685-6.
- [Google Scholar]
- Transplantation of hair follicles for vitiligo. In: Gupta S, Olsson M, Kanwar A, Ortonne JP, eds. Surgical Management of Vitiligo. Oxford: Blackwell Publishing; 2007. p. :123-7.
- [Google Scholar]
- Single-hair follicular unit transplant for stable vitiligo. J Cutan Aesthet Surg. 2011;4:41-3.
- [Google Scholar]
- Repigmentation by outer-root-sheath-derived melanocytes: Proof of concept in vitiligo and leucoderma. Dermatology. 2009;218:342-3.
- [Google Scholar]
- Graying: Gerontobiology of the hair follicle pigmentary unit. Exp Gerontol. 2001;36:29-54.
- [Google Scholar]
- Autologous non-cultured basal cell-enriched epidermal cell suspension transplantation in vitiligo: Indian experience. J Cutan Aesthet Surg. 2011;4:23-8.
- [Google Scholar]
- Corneal epithelial-like transdifferentiation of hair follicle stem cells is mediated by pax 6 and beta-catenin/Lef-1. Cell Biol Int. 2009;33:861-6.
- [Google Scholar]
- Isolation and characterization of neural crest stem cells from adult human hair follicles. Folia Biol (Praha). 2010;56:149-57.
- [Google Scholar]






