Translate this page into:
Alternative Nipple Suspension Technique in the Treatment of Inverted Nipple: Reverse S-Shaped Design
Address for correspondence: Dr. Umut Tuncel, Department of Plastic Reconstructive and Aesthetic Surgery, Faculty of Medicine, Gaziosmanpasa University, Tokat - 601 00, Turkey. E-mail: drumuttuncel@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The primary aim in the treatment of inverted nipple is to achieve a satisfactory and permanent projection of the nipple. The drawbacks of reported techniques include sensory disturbance of the nipple, marked scarring of the nipple and areola, destruction of breast function and incomplete correction. In the present study, the authors introduced a new modification of using two opposite nipple-based areolar dermal flap in the treatment of grades 2 and 3 inverted nipple cases. Nipple-based areolar flaps designed at 3 o’clock and 9 o’clock were raised by two linear incisions and the tip of each flap was sutured on the base of the nipple close to the base itself in a reverse S shape at 6 and 12 o’clock. Successful outcome was obtained due to a strongly suspending effect of the design of the flaps. The mean follow-up period was 6 months. The patients were satisfied with the result and the scars were minimal. The authors recommend the use of the technique that is a simple, reliable and with minimal scars for correcting grades 2 and 3 inverted nipples.
Keywords
Inverted nipple
suspension
reverse S-shaped design
INTRODUCTION
Inverted nipple may cause various cosmetic, psychological, breast feeding and hygienic problems.[12] Providing a symmetrical nipple shape and position with permanent projection is essential when correcting the deformation. Many surgical and nonsurgical techniques have been introduced in the literature. Nonsurgical treatments include breast shells, breast pumps and syringe techniques.[345] However, the beneficial and permanent effects of these treatments are controversial.
In the Teimourian technique which is the one of the most commonly used surgical technique, all the lactiferous ducts are cut and the dermal flaps are used as supportive bulk under the nipple for correcting moderate and severe nipple inversion.[6] In the present study, we aimed to make a new modification of the Teimourian method. We used two opposite nipple-based areolar dermal flaps. After the release of the nipples, the flaps were tunnelised beneath the nipple and the tip of each flap was fixed to the nipple base in reverse S-shaped design. The modified design of the traditional triangular dermal flap procedure provides much more suspension effect as well as filling dead space under the nipple. It represents simple and reliable surgical technique to avoid the recurrence of inversion and to provide satisfying shape and projection of the nipple with minimal scar.
Patients and surgical technique
Three nipples of two female patients treated with the reverse S-shaped fixation method are presented. According to the criteria of Han and Hong,[7] the nipples were classified as grades 2 and 3 [Figure 1]. The cases were congenital without previous surgery.
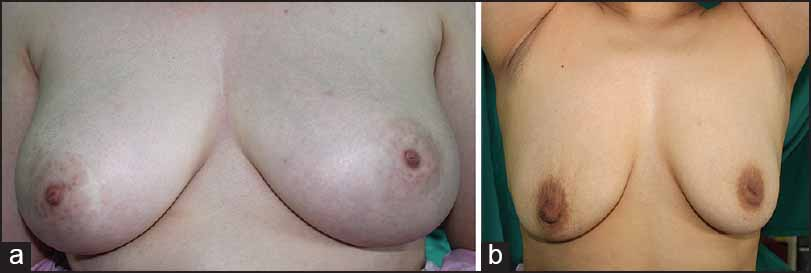
- (a) Preoperative view of the bilateral case. (b) Preoperative view of the unilateral case
The operation was performed under local anaesthesia. First, the nipple was everted by a traction suture. Two opposite linear incisions at 3 and 9 o’clock on the two sides of the everted nipple were made within the range of the areola. Afterwards, the areolar skin was dissected and the epidermis was separated from the dermis over the planned flap area. The base width of the flaps was determined as equal to radius of the nipple. On the two sides of the triangles with no epithelium, the incisions were deepened into the subcutaneous fatty tissue. Two conic shape areolar dermal flaps were created [Figure 2].
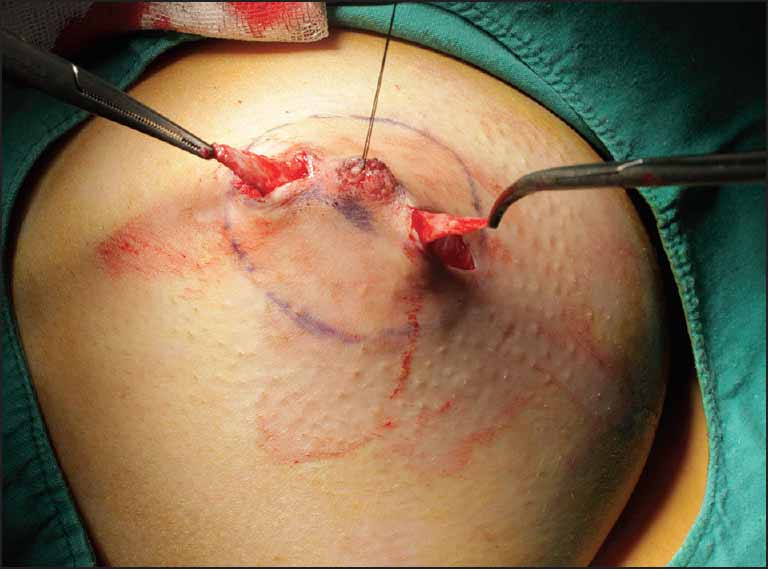
- On the two sides of the triangles with no epithelium, two conic shape areolar dermal flaps were created
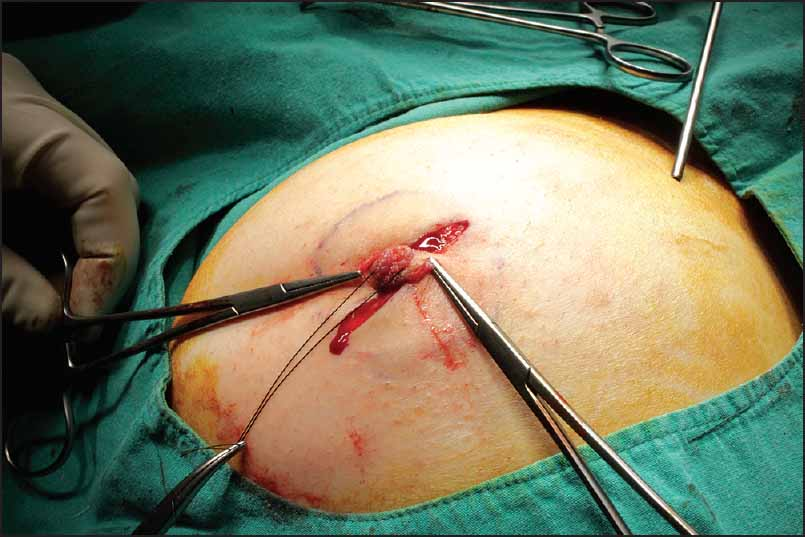
The retracting ducts and fibrous bands beneath the nipple were released with blunt dissection. If the nipple was still not free after these dissections, all the retracting ducts were transected so as not to restrict the nipple. The conic shape triangular flaps on both sides of the inverted nipple were turned down and advanced through the tunnel beneath the nipple as the filling tissue for the dead space [Figure 3]. The tip of each flap was sutured to the nipple base where any incision was not made at 6 and 12 o’clock, also next to the base itself in reverse S shape [Figure 4]. Because the length of the flap is shorter than the diameter of the areolar external circle, the fixations of the flaps provided a strongly suspending effect and the flaps was completely able to fill out the dead space beneath the nipple. The donor areas were closed in two layers. A dressing was applied to avoid compression of the nipple. Continuous traction of the nipple was continued for 2 weeks [Figure 5]. Any complication was not observed and the patients recovered uneventfully during the follow-up period.

- The conic-shape triangular flaps on both sides of the inverted nipple were turned down and advanced through the tunnel beneath the nipple as the filling tissue for the dead space
- The tip of each flap was sutured to the nipple base where any incision was not made at 6 and 12 o’clock, also next to the base itself in reverse S shape

- Early postoperative view of the patient
RESULTS
During the postoperative follow-up period, surgical complications such as traction pain, infection, haematoma, permanent numbness, or skin necrosis were not observed. Follow-up examinations were performed at 3 to 9 months (average, 6 months) and revealed no evidence of recurring inversion.
DISCUSSION
Inverted nipple can simply be defined as nipples that lie on a lower plane than the areola due to shortened lactiferous ducts embedded in short fibrous bands. The grading system by Han and Hong is commonly used to determine the grade of deformation.[7] According to the grading system, in grade 2 cases, the nipples can be pulled out but cannot maintain projection and have strongly tendency to go back again. These nipples are thought to have moderate fibrosis beneath the nipple. Blunt dissection for surgical release should be performed until the inversion does not recur without traction. The lactiferous ducts are mildly retracted and do not need to be cut for the release of fibrosis in the majority of the patients. A temporary traction suture with a suitable dressing is generally preferred after surgery for 2 weeks. In grade 3 cases, the nipple can hardly be pulled out manually due to the severe fibrosis. For correcting grade 3 cases, the fibrotic bands and lactiferous ducts are widely dissected and cut. Two or three deepithelialised dermal flaps should be used to make up for soft tissue deficiency after the release of fibrotic bands and a traction suture is also applied postoperatively.
There are numerous surgical and nonsurgical techniques introduced in the literature[8910] and among these, the incision-release and local flap methods are generally used in the treatment of grades 2 and 3 nipple inversion cases. Many of the flap descriptions over the last two decades are designed on the Teimourian technique. In these techniques, two or three triangular flaps tunnelled and approximated below the nipple are used to fill the dead space and achieve eversion.[12111213] The presented method can also be suggested as a modification of the Teimourian method and the technique presented by Kim et al.[14] In this study, we introduced a new nipple suspension technique using nipple-based dermal flaps for correcting moderately and severely inverted nipples. The most significant difference of the recommended method is in its geometrical design as compared to similar surgical methods using dermal triangular flaps. In our procedure, because two triangular dermal nipple-based areolar flaps are fixed on the opposite side of the nipple base, their geometrically design was called reverse S shape. As a consequence of this design, the reverse S-shaped fixation of triangular flaps provides more traction effect to keep the nipples in protruded position after they are released. The other advantages and differences of our technique is as follows:
-
Linear incision is used to create the triangular flaps on the areola, thus the scar is more uneventful and minimal;
-
The operation time is relatively shorter because the flaps are raised without deepithelialisation;
-
The triangular dermal flaps provide enough bulk beneath the inverted nipple;
-
The size of the triangular flap is slightly shorter than the diameter of the areola, the flaps cause an efficiently suspending effect under the released nipple; and
-
The lactiferous ducts can be preserved in grade 2 cases or if the women particularly hope to breast feeding.
The technique introduced is not to be able to preserve the lactiferous tubules. However it is well-known that these functional units beneath the nipple areolar complex may already be absent in grade 2 and especially grade 3 inverted nipple cases. Optimal surgical procedure in the treatment of the moderate or severe nipple inversion cases should provide a satisfying shape, sufficient projection and preserve ductal function when required. In conclusion, as an alternative nipple suspending method, the reverse S-shaped fixation method of triangular flaps is recommended to be used in any kind of nipple inversion with satisfying results and minimal scar.
ACKNOWLEDGEMENT
The authors disclose that they don’t have any conflict of interest or funding.
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- Correction of inverted nipples by strong suspension with areola-based dermal flaps. Plast Reconstr Surg. 2007;120:1483-6.
- [Google Scholar]
- Correction of inverted nipples with twisting and locking principles. Plast Reconstr Surg. 2006;118:1526-31.
- [Google Scholar]
- Correction of the inverted nipple with an internal 5-point star suture. Ann Plast Surg. 2004;53:293-6.
- [Google Scholar]
- A contemporary correction of inverted nipples. Plast Reconstr Surg. 2001;107:511-3.
- [Google Scholar]
- Using a disposable syringe to treat inverted nipples. Can Fam Physician. 1997;43:1517-8.
- [Google Scholar]
- Simple technique for correction of inverted nipple. Plast Reconstr Surg. 1980;65:504-6.
- [Google Scholar]
- The inverted nipple: Its grading and surgical correction. Plast Reconstr Surg. 2000;105:1576.
- [Google Scholar]
- A new surgical technique for the correction of the inverted nipple. Aesthetic Plast Surg. 1999;23:371-4.
- [Google Scholar]
- Correction of the severely inverted nipple: Areola-based dermoglandular rhomboid advancement. J Plast Reconstr Aesthet Surg. 2011;64:e297-302.
- [Google Scholar]
- Scar-free technique for inverted-nipple correction. Aesthetic Plast Surg. 2010;34:116-9.
- [Google Scholar]
- A new procedure for correction of severe inverted nipple with two triangular areolar dermofibrous flaps. Aesthetic Plast Surg. 2008;32:641-4.
- [Google Scholar]
- A new method for correction of inverted nipple with three periductal dermofibrous flaps. Aesthetic Plast Surg. 2003;27:301-4.
- [Google Scholar]
- Recurrent inverted nipple: A reliable technique for the most difficult cases. Ann Plast Surg. 2012;69:24-6.
- [Google Scholar]
- Correction of inverted nipple: An alternative method using two triangular areolar dermal flaps. Ann Plast Surg. 2003;51:636-40.
- [Google Scholar]






