Translate this page into:
Treatment of a Non-Healing Diabetic Foot Ulcer With Platelet-Rich Plasma
Address for correspondence: Dr. Deepak H Suresh, No 878, First Floor, 14th Cross, Indiranagar, Bangalore - 560 038, Karnataka, India. E-mail: deepakhurkudli@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Lower extremity ulcers and amputations are an increasing problem among individuals with diabetes. Among diabetes mellitus-related complications, foot ulceration is the most common, affecting approximately 15% of diabetic patients during their lifetime. The pathogenesis of diabetic ulcer is peripheral sensory neuropathy, calluses, oedema and peripheral vascular disease. Diabetic ulcer is managed by adequate control of infections and blood sugar levels, surgical debridement with various dressings and off loading of the foot from pressure. In spite of these standard measures, some recalcitrant non-healing ulcers need additional growth factors for healing. Autologous platelet-rich plasma is easy and cost-effective method in treating diabetic ulcers as it provides necessary growth factors which enhance healing.
Keywords
Diabetic ulcer
post-amputation
non-healing
platelet-rich plasma
INTRODUCTION
Chronic non-healing leg ulcer is a major health problem. Chronic wounds come with cost and morbidity for the patients and society also. Over 85% of lower limb amputations are preceded by foot ulcers and diabetes remains a major cause of non-traumatic amputation across the world with rates being as much as 15 times higher than in the non-diabetic population.[1] Conventional therapies such as dressings, surgical debridement and even skin grafting cannot provide satisfactory healing since these treatments are not able to provide necessary growth factors that can modulate the healing process.[2] Autologous platelet-rich plasma (PRP) is an inexpensive method used in treating non-healing ulcers as it provides growth factors which enhance healing.
CASE REPORT
A 57-year-old diabetic male presented with a non-healing wound over the left foot since 4 years. Four years back he had hot water spillage on his left great toe which got secondarily infected and resulted in gangrene. He underwent amputation of great toe (up to metatarsal) for gangrene which left an ulcer over the amputated site. Three months following the amputation, split thickness graft was done for the ulcer. But there was graft failure resulting in a non-healing ulcer. A second split thickness graft was done one year later in January 2012, but the ulcer did not heal [Figure 1]. Since then the chronic non-healing ulcer was managed by debridement and regular dressing without much improvement. On examination, there was a solitary non-tender ulcer over the medial aspect of left foot measuring 5 × 4 × 0.4 cm (width × length × depth) with a well-defined margin covered by granulation tissue and slough surrounded by macerated skin and calluses. Area and volume of the ulcer was 15 cm2 and 6.3 cm3. Wound area was calculated using the formula for an ellipse: Length × width × 0.7854 (an ellipse is closer to a wound shape than a square or rectangle that would be described by simple length × width). The use of an ellipse for calculating wound measurement has been used in randomised controlled trials in wound healing literature.[3] The ulcer was foul smelling. His blood sugar levels were under control. His routine investigations were within normal limits. His baseline platelet count was 2.19 lakhs/cumm.
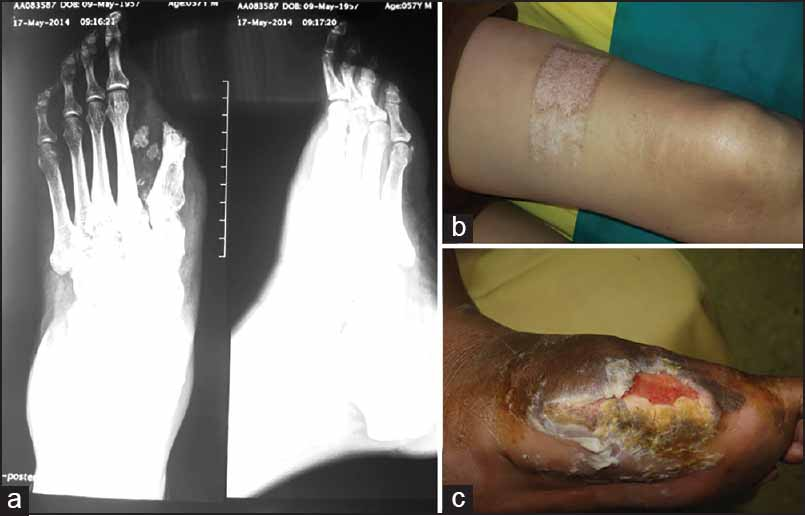
- (a) The X-ray of left foot amputation. (b) The healed donor site of split thickness graft. (c) The non-healing diabetic foot ulcer
20 ml of venous blood was taken and anticoagulated by acid citrate dextrose and PRP was prepared by double centrifugation method. The first spin used was hard spin (5000 rpm for 15 minutes) which separates into three layers: Plasma, buffy coat and red blood cells. The plasma and buffy coat was aspirated into a sterile test tube without an anticoagulant and subjected to a second spin (2000 rpm for 5 minutes). The second spin (soft spin) allows the precipitation of the platelets to 0.8 ml to 1.5 ml to fall onto the bottom. 1 ml of PRP was aspirated and activated with 10% calcium chloride (0.3 ml for 1 ml of PRP) and injected to the ulcer and the edge of the ulcer and covered by paraffin gauze and sterile gauze.[4] The dressing was covered by Dynoplast® [Figure 2]. The dressing was opened on the third day and PRP was repeated once weekly. After 1 week, there was reduction in area and the volume of the ulcer to 12.5 cm2 and 3.75 cm3. After six sittings of PRP, the ulcer healed completely in 7 weeks [Figure 3].

- PRP injected to the ulcer

- (a) The diabetic left foot ulcer before PRP. (b) After 1 sitting of PRP. (c) Ulcer after four sittings of PRP. (d) Ulcer healed completely at the end of 6 sittings
The patient was advised for bed rest for 2 weeks. He was referred to artificial limb centre for proper foot wear (forefoot support with microcellular rubber) to prevent further complications [Figure 4].

- (a and b) The left foot (anterior and lateral view) after 8 weeks. (c) The MCR foot wear
DISCUSSION
Leg ulcers are classified as acute or chronic according to their duration; however, there is no consensus as to a specific length of time to define chronicity. An acute ulcer usually should heal in less than a month. Among chronic ulcers, duration of 6 months or more seems to define the most recalcitrant ulcers.[5] Among diabetic patients, 2-3% will develop a foot ulcer each year, 15% will develop a foot ulcer during their lifetime.[7] Although the pathogenesis of peripheral sensory neuropathy is still poorly understood, there seem to be multiple mechanisms involved, including the formation of advanced glycosylated end products and diacylglycerol, oxidative stress and activation of protein kinase Cβ.[8] The frequency and severity of wound infection is increased in diabetes, which may be related to high glucose levels or impairment of granulocytic function and chemotaxis.[9] In addition, there seems to be a prolonged inflammation, impaired neovascularisation, decreased synthesis of collagen, an abnormal pattern of synthesis of extracellular matrix proteins and decreased fibroblast proliferation.[10] The main principles of treatment are relief of any pressure from the wound by total contact casting, adequate control of infection, debridement of devitalised tissue and control of blood sugar levels. If the standard measures fail, new therapeutic options such as recombinant human growth factors and bioengineerd skin substitutes may be benefited but cost is the limiting factor. Autologous PRP is a cost-effective method. PRP enhances wound healing by promoting the healing process by seven growth factors present in it. They are platelet-derived growth factor (PDGF-αα, αβ, αβ), fibroblast growth factor, vascular endothelial growth factor, epidermal growth factor and transforming growth factor. These growth factors are important in modulating mesenchymal cell recruitment, proliferation and extra-cellular matrix synthesis during the healing process.[11] PDGF stimulates chemotaxis, proliferation and new gene expression in monocytes, macrophages and fibroblasts in vitro, cell types considered essential for tissue repair. Transforming growth factor-β stimulates cell proliferation, protein synthesis and collagen synthesis. It also inhibits growth of many epithelial tumour cells and fibroblastic cell lines. Platelet-derived angiogenesis factor is a polypeptide capable of stimulating new capillary growth by inducing migration of endothelial cells. Platelet-derived epithelial cell growth factor is partially responsible for the initial influx of neutrophils into the wound space; it is also a mitogen for many cells, including epithelial cells and fibroblasts. More recently, it was suggested that this was the mechanism by which platelet factors influence the process of angiogenesis and revascularisation, thus promoting granulation tissue formation.[12] In addition to growth factors, leucocytes also help in wound healing as the have and also help in preventing infections. In our case, the patient was suffering from non-healing diabetic foot ulcer for more than two and half years. The patient had under gone skin grafting which was not useful. The patient was treated with all standard care like off loading of foot from pressure, systemic antibiotics and his diabetes was under control. In spite of these measures, his foot ulcer did not heal and the patient was physically and mentally traumatised. We treated his non-healing foot ulcer with PRP and ulcer healed completely in 6 weeks.
CONCLUSION
Diabetic foot ulcer is a major health problem and in 15% it leads to amputation. There is prolonged inflammatory phase which results in delay in granulation tissue formation and decrease in tensile strength of the wound. PRP enhances wound healing by providing necessary growth factors and reducing the inflammation. We treated a long-standing recalcitrant graft failure diabetic foot ulcer successfully with PRP. Autologous PRP is a safe, inexpensive method in treating diabetic foot ulcer.
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- Cellular and molecular basis of wound healing in diabetes. J Clin Invest. 2007;117:1219-22.
- [Google Scholar]
- Autologous platelet rich plasma in chronic venous ulcers: Study of 17 cases. J Cutan Aesthet Surg. 2013;6:97-9.
- [Google Scholar]
- Comparison of negative pressure wound therapy using vacuum-assisted closure with advanced moist wound therapy in the treatment of diabetic foot ulcers: A multicenter randomized controlled trial. Diabetes Care. 2008;31:631-6.
- [Google Scholar]
- Efficacy of autologous platelet rich plasma in the treatment of chronic non healing leg ulcers. Plast Aesthet Res. 2014;1:65-9.
- [Google Scholar]
- Causes, investigation and treatment of leg ulceration. Br J Dermatol. 2003;148:388-401.
- [Google Scholar]
- Differences in cellular infiltrate and extracellular matrix of chronic diabetic and venous ulcers versus acute wounds. J Invest Dermatol. 1998;111:850-7.
- [Google Scholar]
- Quality assessment of platelet concentrates prepared by platelet rich plasma-platelet concentrate, buffy coat poor-platelet concentrate (BC-PC) and apheresis-PC methods. Asian J Transfus Sci. 2009;3:86-94.
- [Google Scholar]
- Current applications of platelet gels in facial plastic surgery. Facial Plast Surg. 2002;18:27-33.
- [Google Scholar]






