Translate this page into:
When Expanding a Margin of Skin Cancers After Reconstruction with Local Flap: Where to Do It?
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Dear Editor,
The basic principle of facial plastic and reconstructive surgery is the removal of the tumour with optimal aggressiveness, and the operational defects must be closed with the simplest method.
The involvement of deep margins correlates with a higher incidence of relapse, and so there is a further indication for re-excision. We can use three techniques to evaluate the margins: Mohs micrographic surgery, extemporaneous histological examination, and in cases where it is not possible to use the previous methods, a defect can be left open for a few days (without a considerable disadvantage) until the definitive histological examination.
Often, when re-excision is required in an area previously reconstructed by locoregional flaps, there may be difficulties in finding the points where the enlargement needs to be made.
In order to make this decision, three key points need to be clarified:
-
Which margin is positive?
-
Which type of local flap we used to repair the defect?
-
What kind of movement the flap undergoes? [Figure 1].
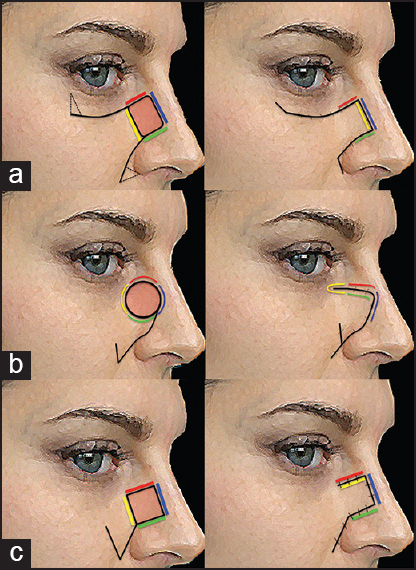
- (a) With an advancement flap, if we were to make an enlargement of a margin (in red), this would not change its position after the advancement, but it would be necessary to lift the coverage flap in order to make said enlargement (b) A rotation flap: We usually divide the removed piece into four parts: So, if the need to make an enlargement should arise, it would be easier to do (c) The more complex transposition flap involves rotating an adjacent piece of tissue, resulting in the creation of a new defect which must then be closed
For example, we report a case of a female, S.Q., 62-years old, who underwent excision of BCC in the caruncle and internal canthus of the left eye and immediate reconstruction with frontal flap [Figure 2a]. The excision was incomplete according to the pathological report (histological findings showed involvement of the medial margin of the skin). Therefore, she underwent elective re-excision of cutaneous medial margin, but it was not easy and intuitive to understand where expanding after reconstruction with frontal transposition flap [Figure 2b]. For this reason it was necessary to re-evaluate the pre- and intra-operative photos and, together with the description of the pathologist (assisted by the use of landmarks on the piece removed), we decided to enlarge the skin adjacent to the bridge of the nose and above the frontal flap.
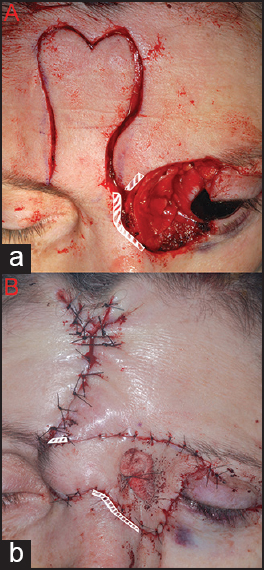
- (a) Preoperative view of a 62-year-old woman with basal cell carcinomas in the caruncle and internal canthus of the left eye. She underwent excision and immediate reconstruction with a frontal flap (b) Postoperative views after 1 month from the first operation and before the re-excision (re-enlargement on cutaneous medial margin). The white dotted line shows that, after this complex reconstruction, it is not intuitive where the re-enlargement should be made
In order to better understand where an enlargement needs to be made it is important to consider not only the geometric shape in which the lesion is included, but also the type of movement that the flap undergoes. Performing an enlargement after reconstruction with a transposition or rotation flap is more difficult than performing an enlargement following an advancement flap [Figure 1].[12]
From our clinical experience we have observed the importance of the following points:
-
The use of landmarks in the piece that we removed.
-
The evaluation and comparison of preoperative and intraoperative photos.
-
The close cooperation with the pathologist.
-
The enlargement, made during flap in setting and shaping, should always be sent to the pathologist for histological analysis.
Margins should always be assessed in the following way:
-
Orient and ink the specimen.
-
Use different ink for different sides of the specimen.
-
Re-excision specimens should be oriented, inked and sent to the pathologist along with a pre-operative photo of the patient where enlargements and their landmarks are shown.
Although this field is undeniably in a state of flux, rudimentary guidelines can be established:
-
The surgeon must apply oncologic principles during a skin cancer resection to increase the right orientation of the tumor;
-
The pathologist must consider techniques that increase the accuracy of margin analysis;
-
The surgeon and the pathologist must collaborate closely to assess the actual needs of enlargement.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Local flap reconstruction of defects after excision of nonmelanoma skin cancer. Clin Plast Surg. 1997;24:747-67.
- [Google Scholar]





