Translate this page into:
Double Hatchet Flap for Scalp Defect Reconstruction
Address for correspondence: Dr. Roberto Cecchi, UO Dermatologia, San Jacopo Hospital, Pistoia - 51100, Italy. E-mail: r.cecchi@usl3.toscana.it
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Dear Editor,
The repair of scalp defects, not suitable for primary closures, can be problematic due to the limited mobility of the scalp tissue. Traditional local flaps have a limited role at this level to restore moderate size defects. Second intention healing or skin grafting are reasonable options, especially in older patients. However, both methods inevitably result in suboptimal cosmetic outcomes with depressed, dyschromic, and hairless scars. Therefore, new reconstruction approaches are always welcome.
The “hatchet” flap is a procedure first described by Emmett in 1977, that has been successfully used in recent years to repair wounds in different body areas, including the craniofacial region, trunk, and limbs.[12] In particular, the modified double hatchet flap (DHF) technique has shown excellent results in the reconstruction of moderate to large scalp defects.[34]
We report our favorable experience with the use of DHF in 22 patients (nine females, 13 men) with skin defects in different scalp sites, following tumor excisions. The patient ages were 64-88 years (mean age 71 years). Defect sizes ranged from 2.5-4.7 cm (mean 3.3 cm). Further data are indicated in Table 1. In all cases, two hatchet flaps were incised on either side of the defect to the defect. The length of each flap was approximately 1.5 times the wound diameter, while the width of the pedicle equaled the defect radius. Dissection was usually performed at a subgaleal level. The flaps were advanced and rotated to cover the primary defect, while the opposite poles were closed in a V-Y fashion. Flap edges were sutured with simple, interrupted, nonabsorbable sutures, or metallic stitches. Buried sutures were added, if necessary. The mean follow-up was 5.2 months (range 1-10 months).

All surgical procedures were performed under local anesthesia. No relevant complications, such as extensive flap necrosis, wound dehiscence, or scar retraction were observed during follow-up. Minimal flap necrosis occurred on the mid-scalp of three patients with prominent actinic damage. Satisfactory cosmetic outcomes were apparent in all cases. Some patients are illustrated in Figures 1 and 2.
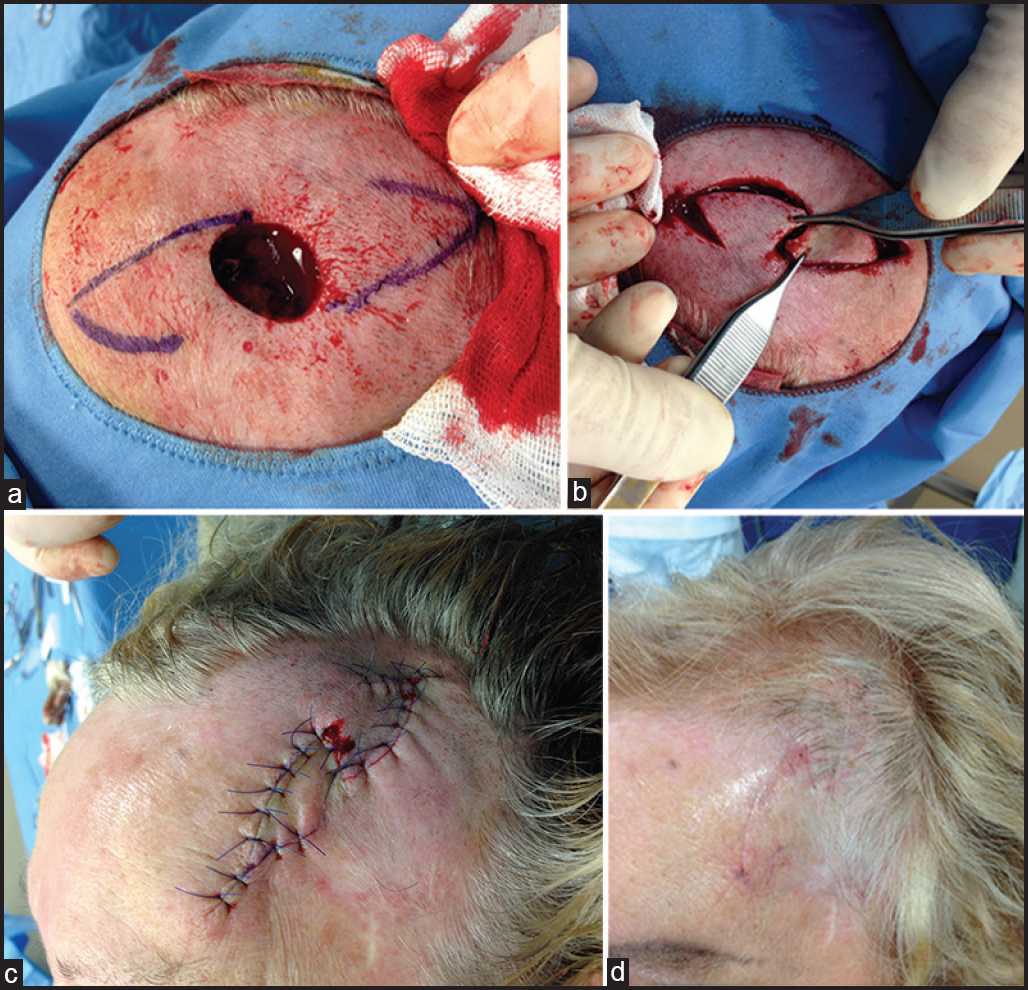
- (a) Frontal/temporal scalp defect after excision of basal cell carcinoma and design of double hatchet flap, (b) double hatchet flap incision and mobilization, (c) view of suture, (d) result after a month
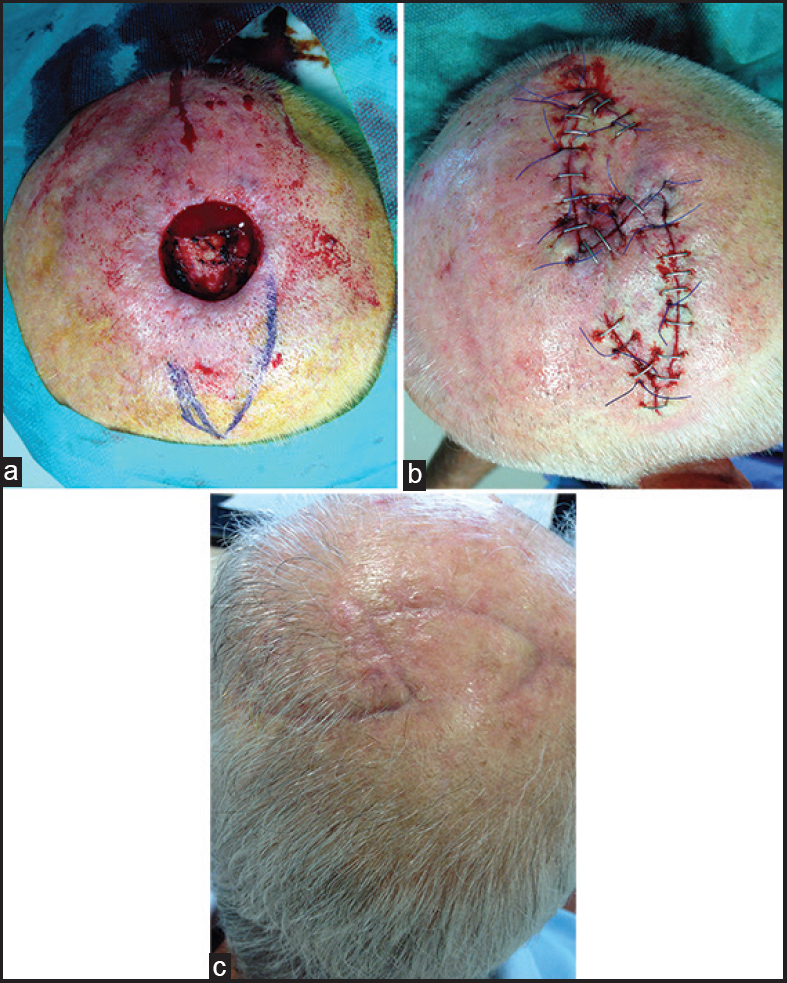
- (a) Defect of the vertex after excision of keratoacanthoma and double hatchet flap marking, (b) flap suture, (c) result after a month
A variety of flap procedures can be achieved to restore scalp wounds. Unilateral or bilateral rotational and transposition flaps are more often used, particularly for losses of the hair-bearing scalp. However, they require extensive incisions and mobilization of skin areas, which are 4-5 times the diameter of defects, in order to allow tension-free closures.[4] Advancement flaps are of little benefit on the scalp, with the exclusion of the central forehead.
DHF is a reliable, versatile, and effective procedure to reconstruct skin defects of moderate to larger size in different scalp regions.[34] The combined effect of rotation and advancing of these flaps allows coverage with a distribution of the traction forces in two opposite directions from the defect. Although, the flap's rotation is made on a relatively narrow pedicle, ischemic failures usually do not occur in areas with a rich vascular network, such as the head. To overcome this risk, the flap base should not be smaller than half the defect to be restored. Finally, DHF should be planned allowing the preservation of the hairline, to warrant a better cosmetic result.
In conclusion, DHF is an easy, time-sparing, but effective solution for single-stage defect reconstruction in a problematic body site such as the scalp.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- The closure of defects by using adjacent triangular flaps with subcutaneous pedicles. Plast Reconstr Surg. 1977;59:45-52.
- [Google Scholar]
- The double hatchet flap: A workhorse in head and neck local flap reconstruction. Arch Facial Plast Surg. 2010;12:198-201.
- [Google Scholar]
- Versatility of hatchet flaps for the repair of scalp defects. Actas Dermosifiliogr. 2012;103:629-31.
- [Google Scholar]
- The double hatchet flap as a potential alternative closure technique for scalp defects. J Dtsch Dermatol Ges. 2015;13:73-5.
- [Google Scholar]





