Translate this page into:
NBUVB Phototherapy at the Donor Site Can Enhance the Graft Uptake in the Nonhealing of Ulcers of Mycosis Fungoides: A Case Report
Address for correspondence: Dr. Sushama Sushama, Department of Dermatology, Flat No. 301, Ohad Homes Welfare Society Apartment, Medical Road, Zakaria Market, Aligarh 202001, Uttar Pradesh, India. E-mail: singh.sushama@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Mycosis fungoides is a rare form of non-Hodgkin’s lymphoma, which is formed of mature, skin homing, clonal, malignant T lymphocytes. It can sometimes present with skin ulcers that are difficult to heal because of the presence of large number T lymphocytes and antigen-presenting cells. We present a case of nonhealing ulcers in a patient with mycosis fungoides, which was treated by narrow band ultraviolet B targeted phototherapy followed by split-thickness skin grafting. The graft uptake was well and the donor area also healed without any complications.
Keywords
Mycosis fungoides
phototherapy
split-thickness skin grafting
ulcers
Introduction
Mycosis fungoides is a rare form of non-Hodgkin’s lymphoma, which is formed of mature, skin homing, clonal, malignant T lymphocytes.[1] It is the most common form of cutaneous T-cell lymphoma.[2] Clinical manifestations in skin include patches, plaques, tumors, or generalized erythroderma.[3] Sometimes ulcers can be present, which can occur either due to the disease or treatment.[4] The presence of large number of atypical T lymphocytes and antigen-presenting cells has detrimental effect in healing, hence forming a chronic ulcer unable to heal. Such ulcers can be managed with autologous skin grafting; however, the donor site being affected with disease, there is often failure of graft uptake as shown by Almashagbeh et al.[5]
We present a case of management of nonhealing ulcers in a patient with mycosis fungoides.
Case Report
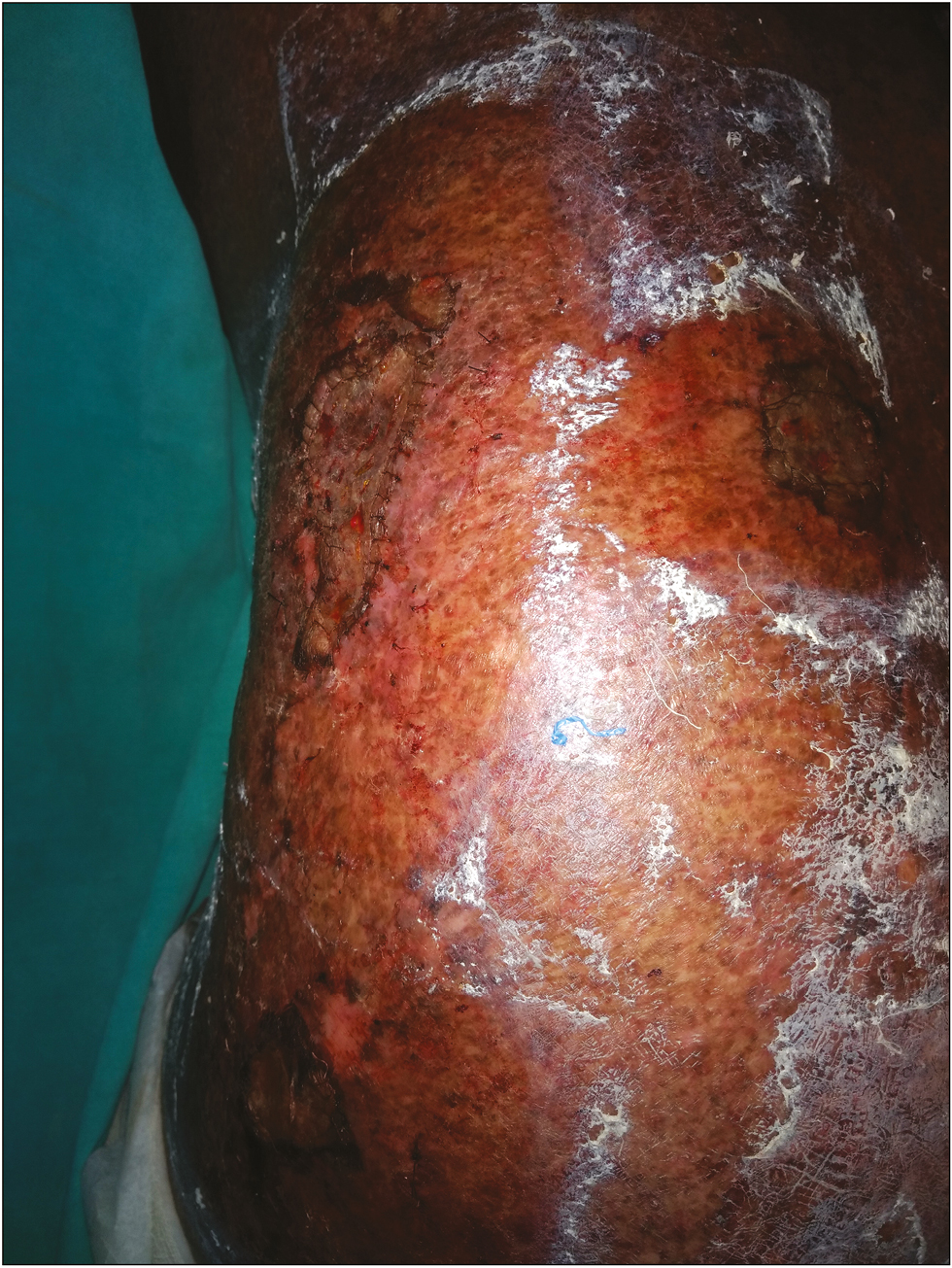
A 45-year-old male presented to the dermatologist with poikilodermatous skin over the whole body. After histopathological examination of the affected skin, a diagnosis of mycosis fungoides was made. The patient was started on topical and oral steroids. However, after a period of about 2 weeks, patient developed spontaneous ulceration of plaques at three places. Antiseptic dressing (with mupirocin) and empirical antibiotics (amoxicillin plus clavulanic acid) were recommended by the dermatologist. However, the ulcers failed to heal even after 2 weeks of treatment. Three ulcers were present, first on left lateral lumbar area of size around 4×5cm with irregular margins, and the second ulcer was smaller in size and circular in shape with diameter of 2cm present on the left buttock on lateral surface. The third ulcer was present on the trunk posteriorly in lower back area also of around 2-cm diameter and circular in shape. Second and third ulcers had regular margins. All three ulcers had sloping edges, floor was covered with granulation tissue, and base was non-indurated [Figure 1]. Though the ulcer had characteristics of healing ulcer, however, the depth and size of the ulcer were more, which rendered it difficult to heal spontaneously. Patient was then referred to plastic surgery for treatment of nonhealing of ulcers. After two more weeks of conservative management, the ulcer failed to heal, so we decided to do a split-thickness skin graft for the nonhealing of ulcers. The main concern, however, was rejection of the graft because of increased immune reaction secondary to increased number of pathologic T lymphocytes.

- Ulcers due to mycosis fungoides
Keeping in mind the aforementioned facts, targeted phototherapy of donor site (lateral surface of thigh) with narrow band ultraviolet B (NBUVB) was given. As no fixed protocol regarding dosage of NBUVB is available, a protocol was empirically framed by us. It was started with a dose of 0.3 J/cm2 and increased at a rate of 20% above the previous dose on each successful day, reaching up to 1 J/cm2 on the eighth day. The same dose was continued for another 2 days while continuing the antiseptic dressing to avoid infection of the ulcers [Table 1].
| Day | Dose of NBUVB (in J/cm2) |
|---|---|
| 1 | 0.3 |
| 2 | 0.36 |
| 3 | 0.43 |
| 4 | 0.51 |
| 5 | 0.62 |
| 6 | 0.74 |
| 7 | 0.89 |
| 8 | 1.0 |
| 9 | 1.0 |
| 10 | 1.0 |
NBUVB = narrow band ultraviolet B
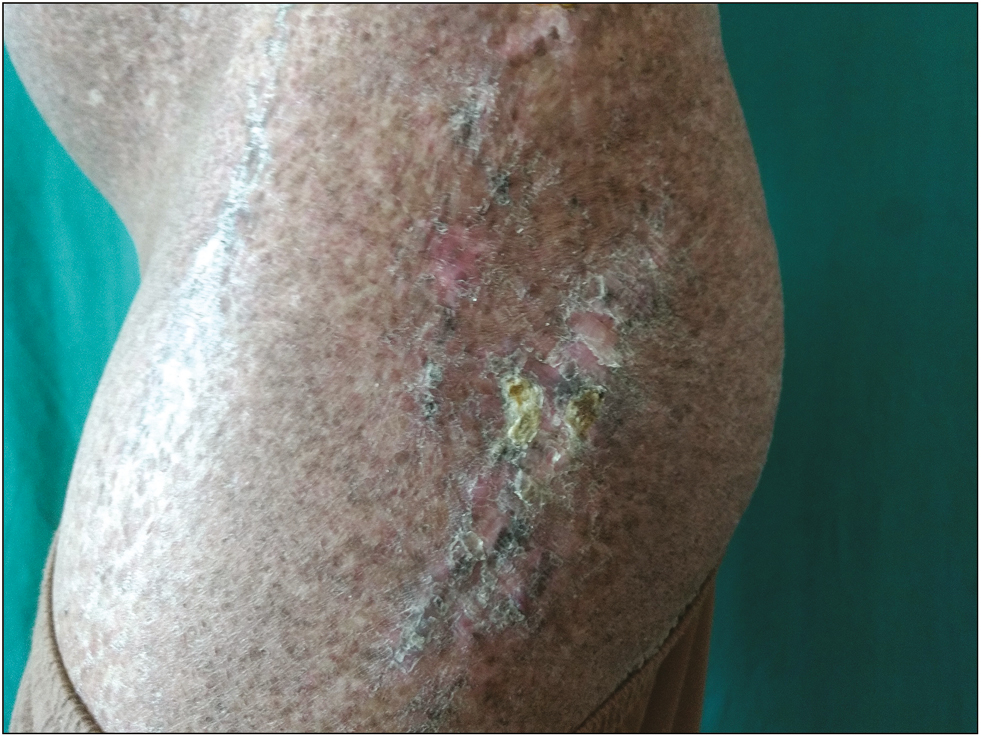
On the 11th day, split-thickness skin graft was planned. After cleaning the donor area (lateral surface of right thigh), partial thickness skin graft of size 6×12cm was taken with the help of Humby knife running it in a back and forth motion and keeping it at an angle of 45° to the taught skin surface. After harvesting the graft, cuts were made in it with knife. This prevents blood and serum from accumulating under the graft. The graft was divided into three parts according to the size of skin defects. Then it was placed on the cleaned recipient site with dermis side down and sutured at margins with absorbable sutures [Figure 2]. Paraffin gauze dressing was then applied. On the fifth day, dressing was opened and the graft was found to be healthy. Dressing was continued and after 2 weeks the graft was adherent to wound. Thereafter dressing was stopped and the patient was asked to apply bland emollients only [Figure 3].
- Postoperative (after split-thickness skin grafting)
- Recipient site after 3 weeks
After harvesting the graft, donor site was covered with paraffin and antibiotic soaked gauze. Dressing was opened after 3 weeks and the donor area had healed well [Figure 4].
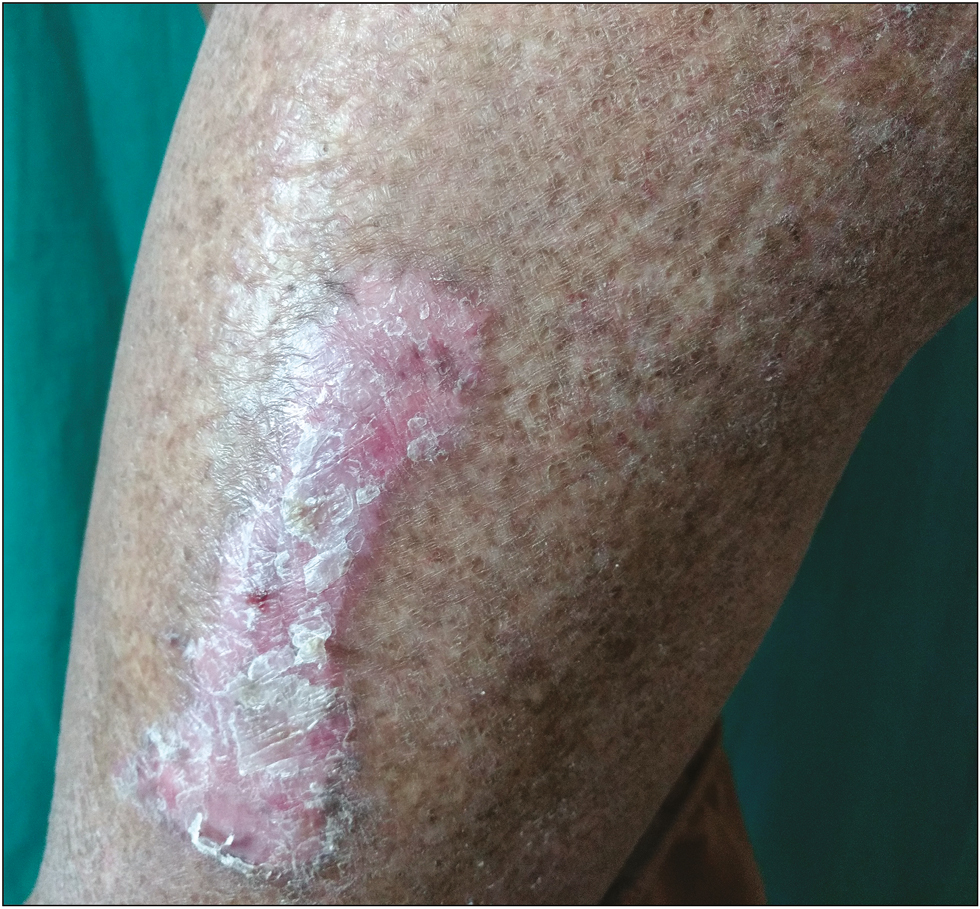
- Donor site after 3 weeks
Discussion
Mycosis fungoides corresponds to the cutaneous lymphoma that has originated from the peripheral epidermotropic T lymphocytes.[6] It commonly presents with patches, plaques, tumors, or erythroderma. A rare variant is poikilodermatous mycosis fungoides, which presents with hypopigmentation admixed with hyperpigmentation, telangiectasia, and atrophy.[7] This variant occurs in young patients as compared to the classic mycosis fungoides that occurs in the elderly. This explains the young age of our patient.
Development of ulcer can occur in a patient of mycosis fungoides either due to the disease or treatment itself. Once these ulcers develop, they are difficult to treat because of excessive number of pathological T lymphocytes that interfere with healing process.[8] Also the epidermal appendages have been destroyed by the disease process and sometimes secondary to the treatment given.[4] Split-thickness skin grafting seemed to be the only method appropriate for faster resolution of the ulcers. Both the aforementioned causes lead to rejection of graft and failure of donor site to heal if a skin graft is planned for the treatment of ulcer. Almashagbeh et al.[5] in their study found that in 10% of their patients treated with skin graft for ulcers (3 patients), the skin graft did not survive without previous therapy with ultraviolet radiation while in 90% (25 patients) of them the grafted areas survived after phototherapy of UV-A, UV-B radiation to the potential donor site.[5]
Studies have shown that suppressing the donor skin antigenicity with photodynamic therapy can prolong the allograft survival.[9] Similar immunosuppression is seen with UV-B therapy, which decreases cytotoxic T-lymphocyte activity with subsequent decrease in delayed type hypersensitivity and increased graft uptake.[10] In addition to that, NBUVB may suppress the neoplastic proliferation of clonal T cells and serve as an up-regulator of the immune system.[11] Several studies have reported that NBUVB induces an increase in expression of interleukin (IL)-2, IL-6, and tumor necrosis factor -α by human keratinocytes and a decrease in the allo-activating and antigen-presenting capacity of Langerhans cells.[1213]
We used the aforementioned property of UV-B for the donor area before the split-thickness skin graft procedure. Reduced inflammatory cells led to better healing in both donor and the recipient area.
Limitation of case report
The ulcers that the patient developed were itself not proven histopathologically to be mycosis fungoides rather was presumed to be because of mycosis fungoides.
Conclusion
NBUVB may suppress the immune response in donor area and increase the graft uptake in split-thickness skin grafting. Thus this can be used as treatment of nonhealing ulcers in mycosis fungoides.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Management of mycosis fungoides. Part 1. Diagnosis, staging, and prognosis. Oncology (Williston Park). 2003;17:1281-8.
- [Google Scholar]
- Mycosis fungoides with mucinosis follicularis in childhood. Dermatology. 1999;198:284-7.
- [Google Scholar]
- The treatment of ulcers in patients with mycosis fungoides with split-thickness skin grafts. Ann Plast Surg. 1984;13:20-3.
- [Google Scholar]
- Mycosis fungoides skin wound management with skin graft post ultraviolet radiation therapy. Int J Med Invest. 2016;5:117-20.
- [Google Scholar]
- Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, eds. WHO classification of tumors of hematopoietic and lymphoid tissues. Lyon (France): IARC; 2008.
- Mycosis fungoides and sézary syndrome: clinical, histopathological and immunohistochemical review and update. An Bras Dermatol. 2012;87:817-28. quiz 829-30
- [Google Scholar]
- The role of lymphocytes in human dermal wound healing. Br J Dermatol. 2000;143:59-65.
- [Google Scholar]
- Prolonged skin allograft survival after photodynamic therapy associated with modification of donor skin antigenicity. Transplantation. 1997;63:810-7.
- [Google Scholar]
- The effect of ultraviolet B irradiation on delayed-type hypersensitivity, cytotoxic T lymphocyte activity, and skin graft rejection. Transplantation. 1989;47:372-6.
- [Google Scholar]
- Mechanisms of ultraviolet (UV) B and UVA phototherapy. J Investig Dermatol Symp Proc. 1999;4:70-2.
- [Google Scholar]
- Biological effects of narrow-band (311nm TL01) UVB irradiation: a review. J Photochem Photobiol B. 1997;38:99-106.
- [Google Scholar]
- The effects of ultraviolet radiation on the human immune system. Br J Dermatol. 1999;140:995-1009.
- [Google Scholar]






