Translate this page into:
Facial Reconstruction According to Aesthetic Units
Address for correspondence: Dr. Silvana L. Chang Grozo, Head, Neck and Maxillofacial Surgery Service, Hospital Nacional Dos de Mayo, Jirón Barlovento 453, Santiago de Surco 15038, Lima, Perú. E-mail: silvanachang5@hotmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Context:
The facial subunit principle organizes the facial skin into subunits. Facial reconstruction for skin cancer based on aesthetic units consists of replacing the entire subunit when a large part of a subunit has been removed.
Aims:
To determine the prevalence of facial skin cancer, their location by facial aesthetic units, and the type of facial reconstruction used in each of them.
Settings and Design:
An observational cross-sectional study was conducted at the Head and Neck Surgery Service of a general hospital between 2017 and 2018.
Materials and Methods:
A population census was conducted during this period.
Statistical Analysis Used:
The categorical variables were expressed as frequencies (percentages). Continuous variables were described as the means and standard deviations or medians and interquartile ranges.
Results:
The most common skin cancer was basal cell skin cancer, followed by epithelial skin cancer and, at last, melanoma. In general, the most frequent localization of these cancers was the nose.
Conclusions:
In spite of primary closure being the most common form of reconstruction, a considerable number of patients required facial reconstruction based on aesthetic facial units, with satisfying results.
Keywords
Facial aesthetic units
reconstruction
skin cancer
Reconstruction based on aesthetic units has the advantage of providing a natural, harmonic, and beautiful result after the excision of the skin cancer, giving the patient the possibility of reincorporating his/her daily activities in the quickest and most natural way possible, with the restoration of form and preservation of function without disfiguring scars in comparison with other types of reconstruction.

INTRODUCTION
Skin cancer has gradually increased its incidence due to changes in the social and medical environment.[1] The main types of skin cancer include basal cell carcinoma, squamous cell carcinoma, and malignant melanoma. The causes attributed to them are multifactorial such as environmental and host factors, especially ultraviolet radiation.[1] The predilected site of skin cancer is the head and neck region because these zones are more exposed to ultraviolet radiation. However, the specific preference of each type of skin cancer has been ambiguous due to the different descriptions of the occurrence sites in various studies.[1]
Facial reconstruction is delicate as the face is the most visible part of the body and has a complex three-dimensional topography.[2] For the reconstruction of facial defects after the excision of cutaneous malignant lesions, it is important to have adequate knowledge of the facial anatomy, the expected surgical defect, and the available reconstructive options.[3] Thus, the goals of facial reconstruction are basically the restoration of form and the preservation of function.[3]
The initial concepts of facial reconstruction were proposed by Gonzales-Ulloa[4] in 1956, who emphasized the need to put an end to the “age of skin-patch surgery” and proposed a method of selective regional restoration by means of “aesthetic units.” This method consists of making cutaneous grafts of the same size, shape, and thickness as the whole region on which the repair is done.[4] Later, in 1981, Millard proposed concepts of facial reconstruction based on facial features, including the three basic layers: cover, frame, and lining.[5] In 1985, Burget and Menick[5] established the initial concepts of aesthetic subunits in nasal reconstruction. Since then, these concepts have been considered as an important step in preoperative planning.[6]
The facial subunit principle organizes the facial skin into subunits that are grouped by skin color, texture, thickness, quantity of subcutaneous fat, mobility, and hair distribution.[7] Each subunit affects the aesthetic of surrounding units.[3] The face is typically divided into six units: forehead, eye and eyebrow, nose, lips, cheek, and chin. Some of them, such as the nose and the auricles of the ear, are subdivided further based on their anatomic complexity.[7] For example, the nose is composed of the back, tip, columella, paired wings, lateral walls, and soft triangles.[8]
The facial reconstruction based on aesthetic subunits consists of replacing the whole subunit, instead of simply patching the defect, when a large part of a subunit has been removed.[8] It also allows the placement of incisions along the edges of the aesthetic subunits, minimizing scars.[6] For better results, a flap should be designed within the limits of the cosmetic facial unit in which the primary defect is located, and the incisions need to be arranged along the borders of the units, without crossing them.[7] It should also be noted that the best results are obtained with the reconstruction of complete cosmetic units, even though the defective area is smaller than the whole unit.[7] For example, if the defect involves greater than 50% of the subunit, it is better to perform the resection of the whole subunit, in order to achieve better aesthetic outcomes by camouflaging the incisions at the border of the aesthetic subunits.[2]
The aim of this study was to determine the prevalence of facial skin cancer (basal cell carcinoma, squamous cell carcinoma, and malignant melanoma), their location by facial aesthetic units, and the type of facial reconstruction used in each of them, as well as presenting cases where reconstruction based on aesthetic units was used.
MATERIALS AND METHODS
An observational cross-sectional study was conducted at the Head and Neck Surgery Service of a general hospital between 2017 and 2018, which attends patients who need specialized care as cancer management.
The study population consists of patients attended during the period of study with the diagnosis of skin cancer by the previous biopsy, who underwent surgery in the minor surgery room of the Head and Neck Surgery Service, and who attended their postoperative control. The patients included should have had their diagnosis confirmed by postoperative pathology. Patients with compromised edges in the pathological site of the skin and who did not attend their postoperative control where excluded from the study.
During the surgical procedure, once the lesion has been resected and the defect defined, two types of closure can be chosen. The first is the primary closure. The second is the closure based on aesthetic units, which consists of designing facial flaps that, according to the need, can rotate, advance, or interpolate, following the edges of the units or facial aesthetic units and subunits.
Informed consent was obtained in all cases before performing surgery. Medical records and pre- and postoperative photographs were used as a source of information. Data were collected by health workers of the Head and Neck Surgery Service of Hospital Nacional Dos de Mayo. The data were entered into a database in Microsoft Excel 2010, and quality control was performed by double digitization of data.
Data analysis was performed using the statistical package Stata version 13.0 (StataCorp LP., College Station, TX). For univariate analyses, the categorical variables were expressed as frequencies (percentages). Continuous variables were described as the means and standard deviations or medians and interquartile ranges (IQRs).
RESULTS
A population census was conducted in 71 patients. Overall, 75 patients underwent surgical management during the study period; 4 patients were excluded, including those whose margins were compromised by neoplasia (n = 2) and who did not attend their postoperative control (n = 2), as a result only 71 patients were included in the analysis. Among the 71 patients, 60 patients (84.5%) had a diagnosis of basal cell skin cancer, 10 patients (14%) of squamous cell skin cancer, and 1 patient (1.4%) of melanoma. The median age was 76 years (IQR: 20.5), and 42 patients (59.1%) were female [Figure 1].
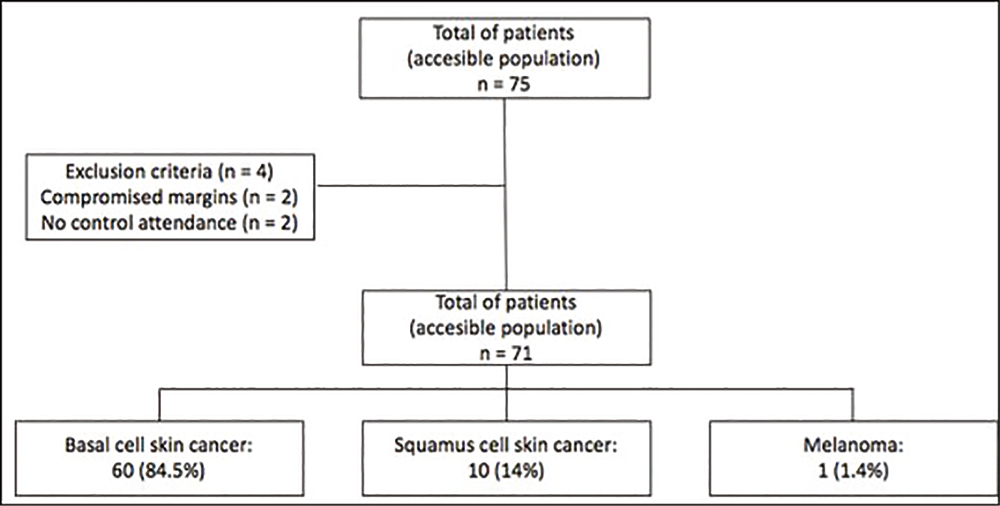
- Flow chart of patients included in the analysis
Regarding patients with basal cell cancer, the most frequent localization was the nose with 29 cases (48.3%) followed by the eyelid and the nasogenian region with 7 cases (11.6%) each. Furthermore, six cases (10%) were located on the cheek, three cases (5%) on the lips, ear and eyebrow each, and finally, two cases (3.3%) in the forehead [Table 1; Figure 2].
| Patient characteristics | Total |
|---|---|
| Age, years | 76 ( 20.5) |
| Sex | |
| Female | 42 (59) |
| Diagnosis | |
| Basal cell skin cancer | 60 (84.) |
| Squamous cell skin cancer | 10 (14) |
| Malignant melanoma | 1 (1.4) |
| Localization of basal cell cancer | |
| Nose | 29 (48.3) |
| Eyelid | 7 (11.6) |
| Nasogenian | 7 (11.6) |
| Cheek | 6 (10) |
| Lips | 3 (5) |
| Ear | 3 (5) |
| Eyebrow | 3 (5) |
| Forehead | 2 (3.3) |
| Localization of squamous cell cancer | |
| Nose | 3 (30) |
| Lips | 2 (20) |
| Cheek | 2 (20) |
| Chin | 1 (10) |
| Nasofrontal orbital | 1 (10) |
| Nasogenian | 1 (10) |
| Localization of melanoma | |
| Nose | 1 (100) |
| Reconstruction in basal cell cancer | |
| Primary closure | 51 (85) |
| Facial aesthetic units | 9 (15) |
| Reconstruction in squamous cell cancer | |
| Primary closure | 6 (60) |
| Facial aesthetic units | 4 (40) |
| Reconstruction in melanoma | |
| Facial aesthetic units | (100) |
The results are expressed as the median (IQR) or n (%).
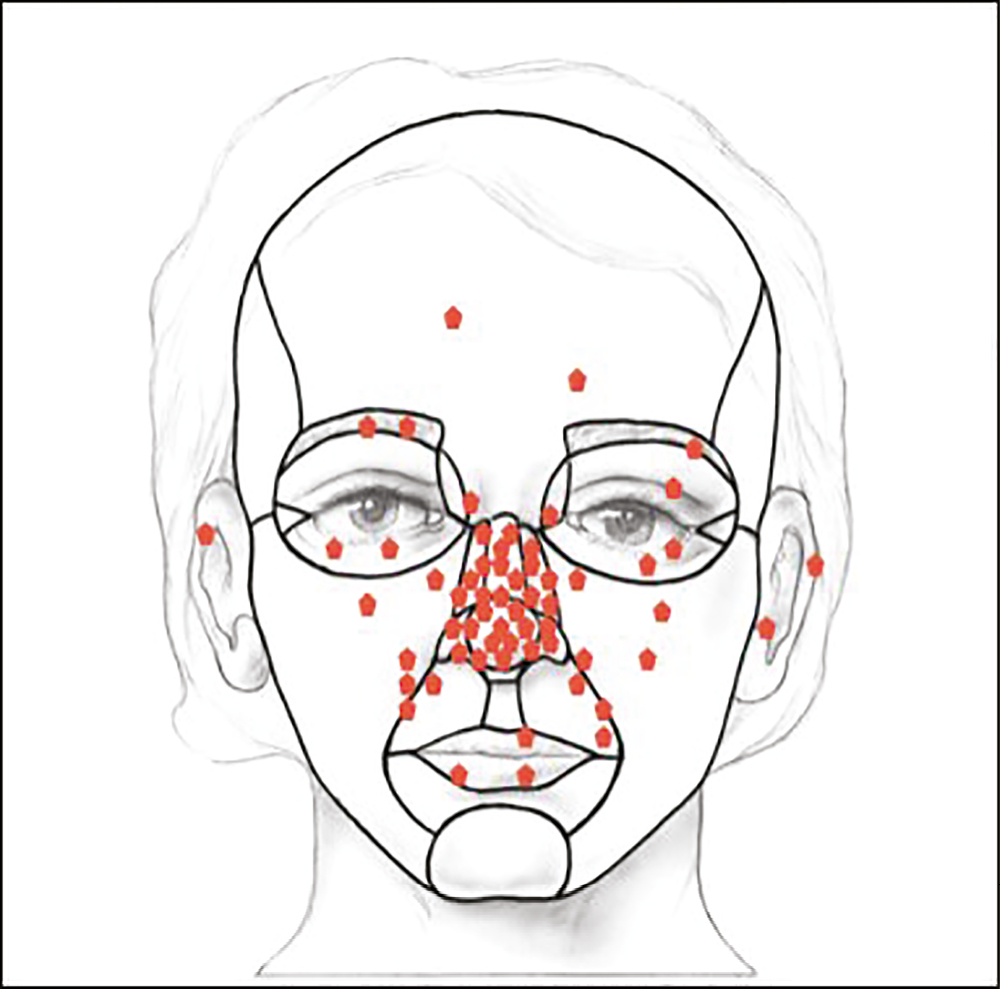
- Localization of basal cell skin cancer based on facial aesthetic units
In all locations of basal cell cancer, the most frequent type of reconstruction was the primary closure, which was used in 51 cases (85%), followed by reconstruction based on facial aesthetic units in 9 cases (15%) [Figures 3 and 4].
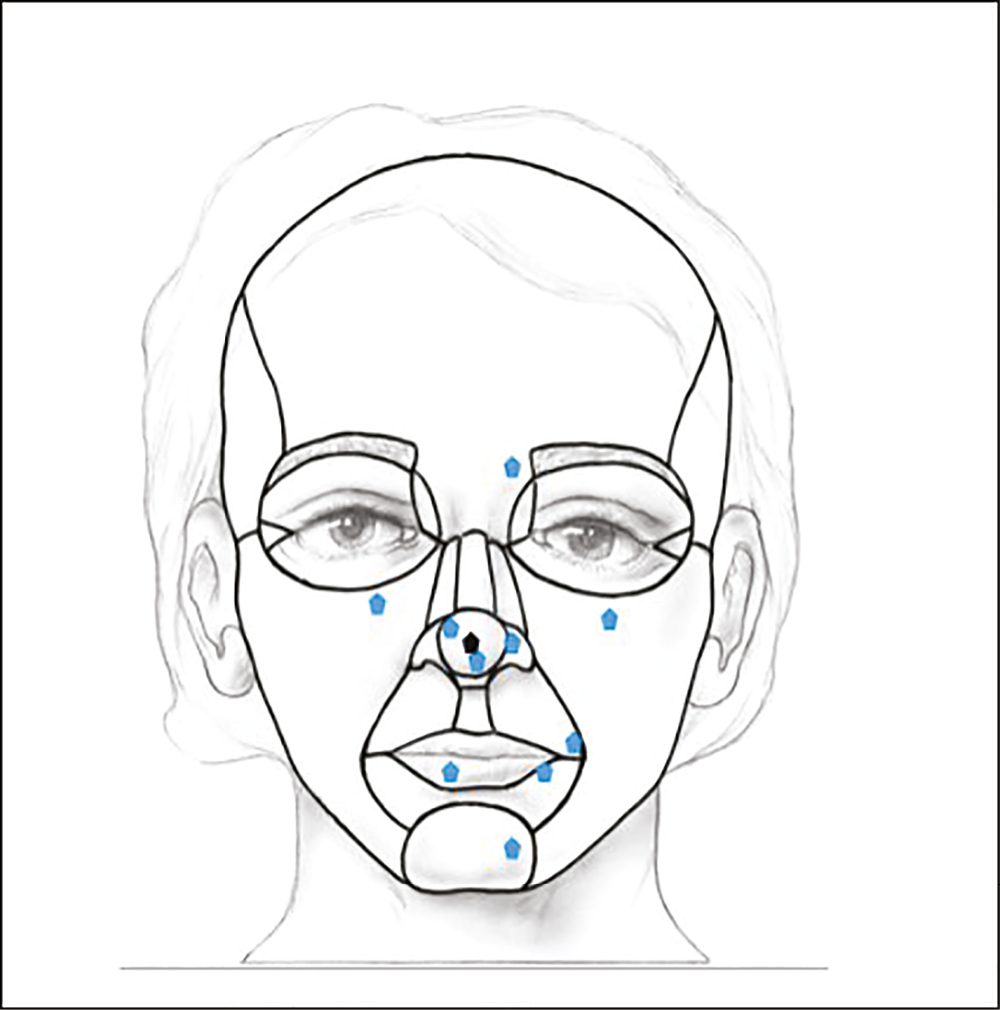
- Localization of squamous cell skin cancer based on facial aesthetic units
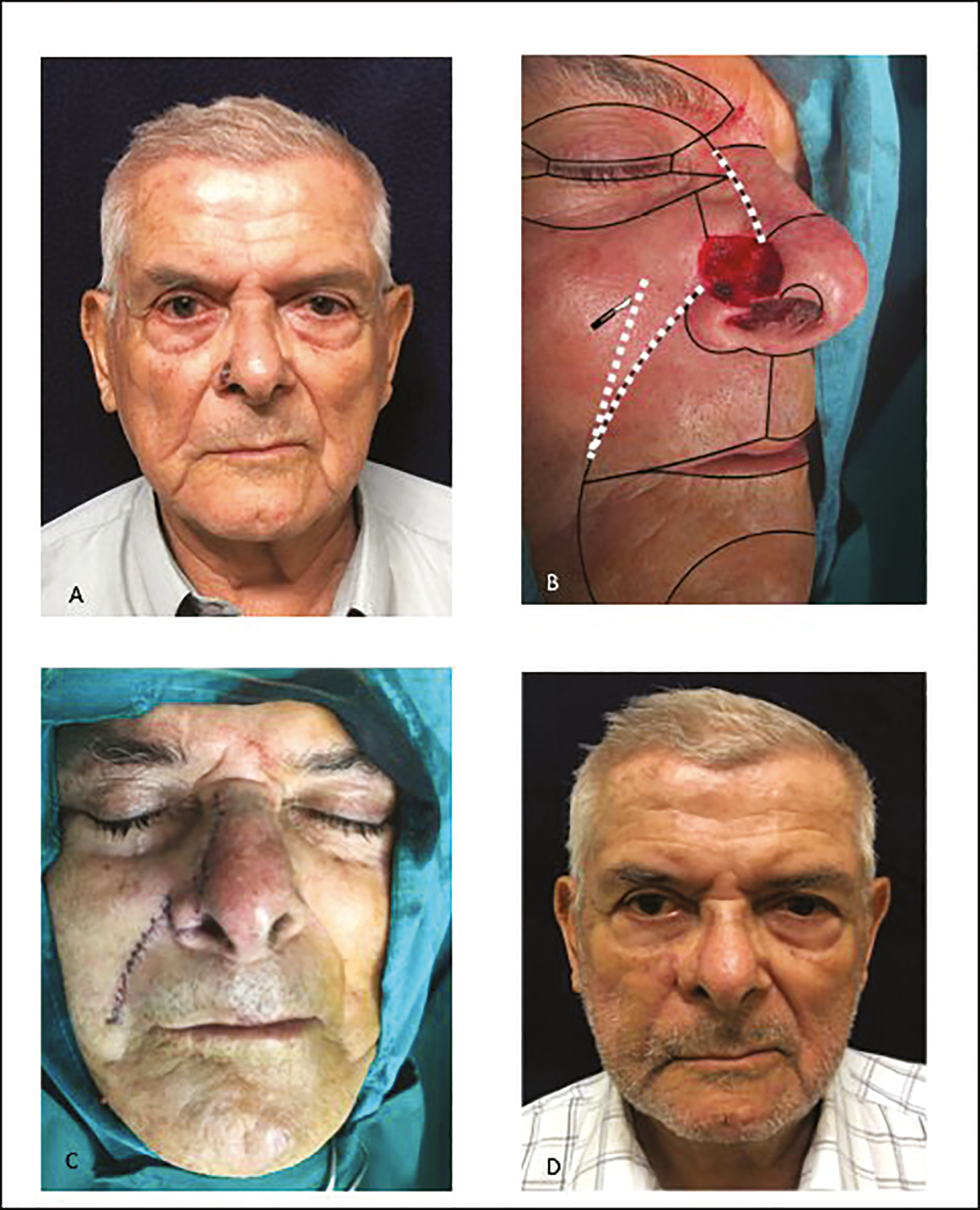
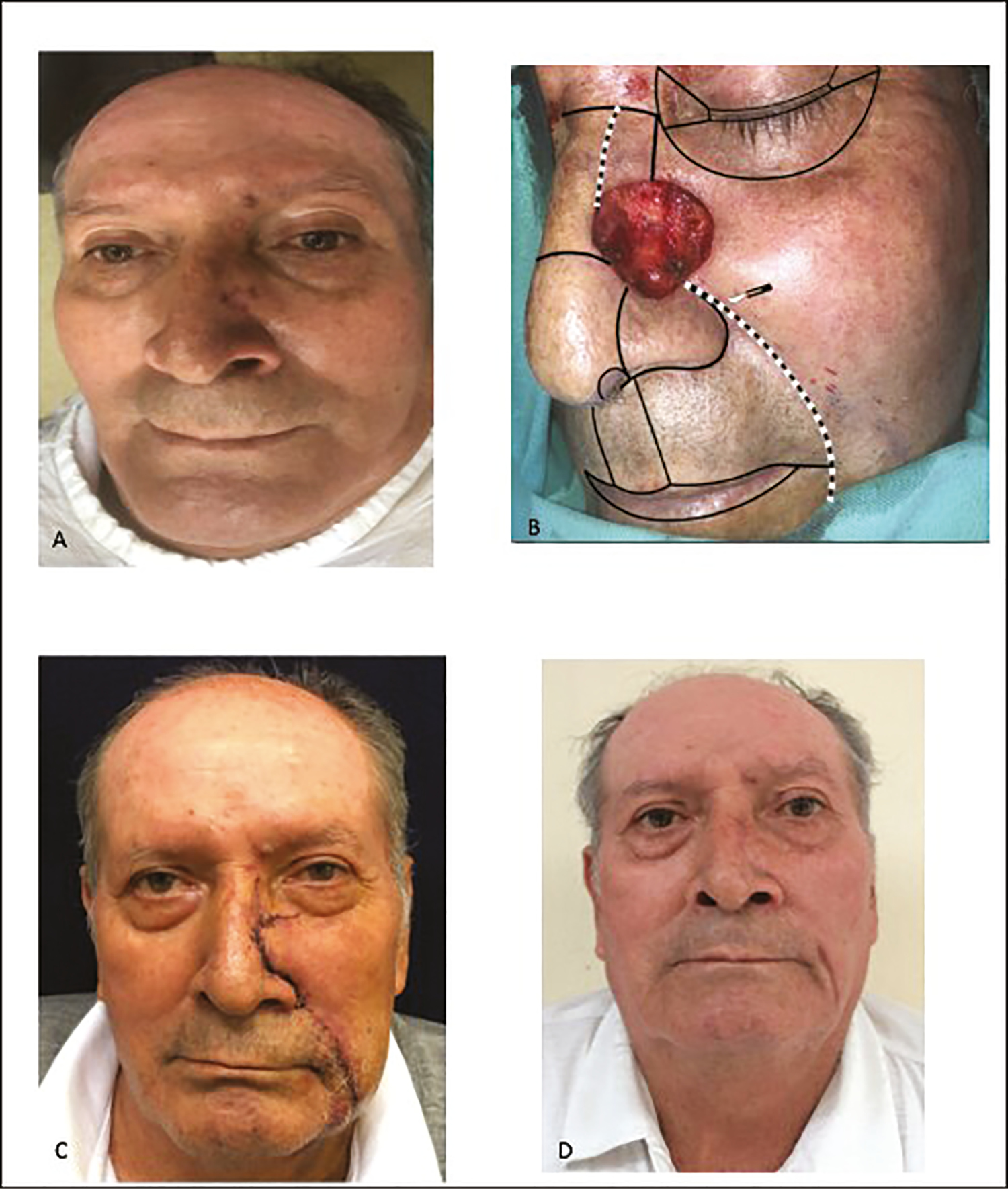
- Reconstruction of basal cell skin cancer based on aesthetic units. (A) Preoperative photograph, (B) reconstruction based on aesthetic units, (C) immediate postoperative result, and (D) control
On the other hand, the most frequent location of squamous cell cancer was the nose, which was evident in three patients (30%), followed by lips and cheek in two patients (20%) each. The least frequent locations were chin, nasofrontal orbital region, and nasogenian region, with one case (10%) each [Table 1; Figure 5].
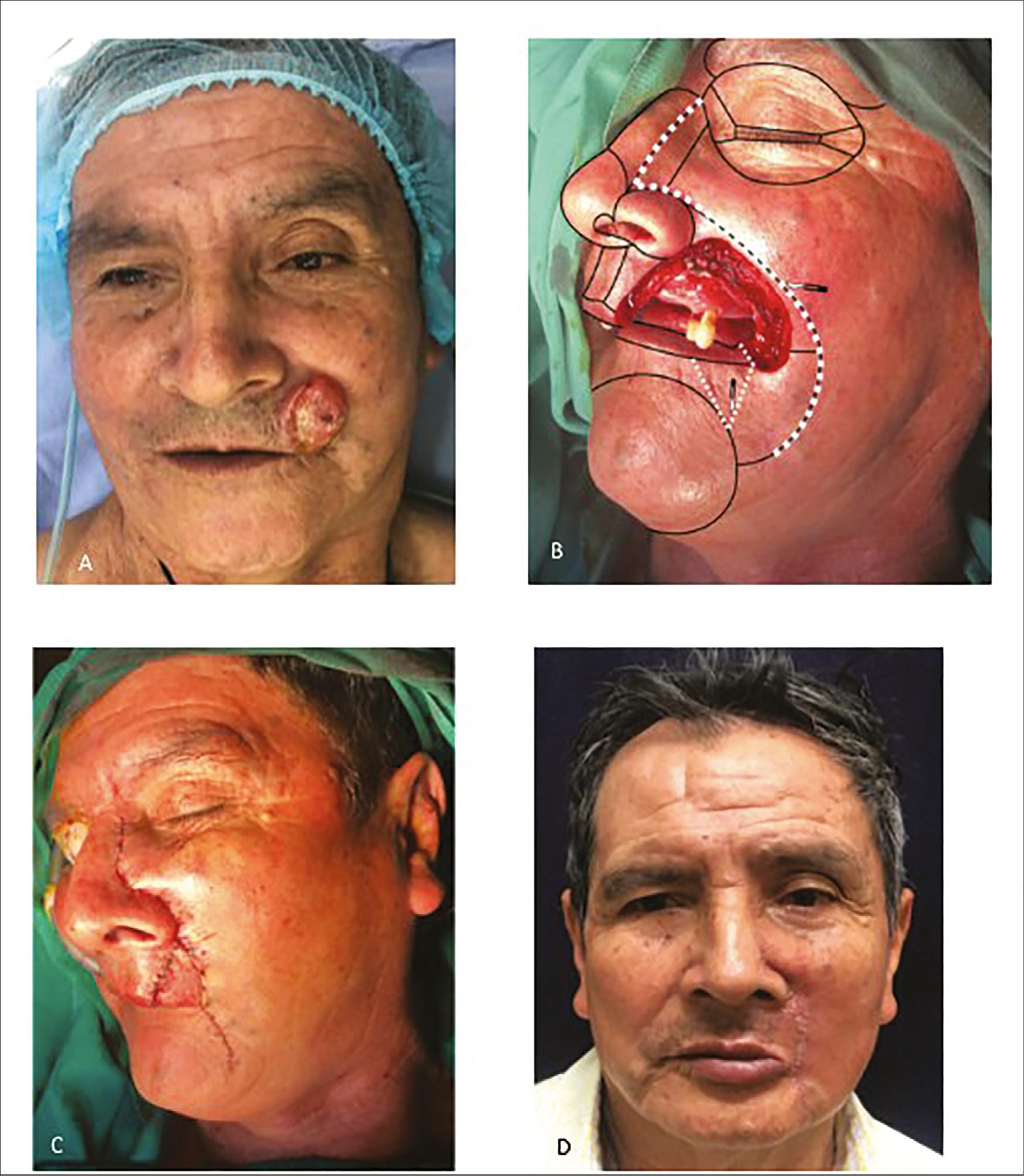
- Reconstruction of basocelular skin cancer based on aesthetic units. (A) Preoperative photograph, (B) reconstruction based on aesthetic units, (C) immediate postoperative result, and (D) control
With respect to the type of reconstruction used in this type of cancer, it was found that the primary closure was performed in six patients (60%) and reconstruction based on the facial aesthetic units was performed in four patients (40%) [Table 1; Figure 6].
- Reconstruction of squamous cell skin cancer based on aesthetic units. (A) Preoperative photograph, (B) reconstruction based on aesthetic units, (C) immediate postoperative result, and (D) control
Finally, the location of the only case of melanoma was the nasal tip. In this patient, a type of frontal flap closure based on the facial aesthetic units was performed [Table 1].
DISCUSSION
Skin cancer was the most commonly diagnosed cancer in the United States, with more than 1 million Americans diagnosed with skin cancer each year.[9] They are usually found in sun-exposed areas, especially the head and neck regions.[10] Our study found a high prevalence of basal cell skin cancer, followed by squamous cell skin cancer and malignant melanoma. These results agree with the findings of Choi et al.,[1] who found in their study that the most common cutaneous malignant mass was basal cell skin cancer (64.4%), followed by squamous cell skin cancer (32.2%).
In our study, we found that the most common location of basal cell skin cancer was the nasal unit, followed by the eyelid. These results agree with the findings of Choi et al.,[1] who also found that the most common location was the nasal unit (48.7%), and Jung and Kim[11] who reported that the most frequent location of this type of cancer was the nose (38.4%). In addition, Kim et al.[12] also reported the nose as being the most common region for basal cell skin cancer (47.3%). On the other hand, Kim et al.[12] reported that basal cell skin cancer had occurred on the cheek, followed by the periorbital area and the nose.
Regarding the most common location of squamous cell skin cancer, we found that the nasal unit was the most affected, followed by lips and cheek; contrary to the findings of Choi et al.,[1] who found that the most common location for this type of skin cancer was the buccal unit (21.1%), followed by the parotid-masseteric unit (18.4%). Jung and Kim[11] reported that it occurred most commonly on the lower lip (41%), followed by the cheek (23.2%), whereas Kim et al.[12] reported that it occurred on the lower lip (26.2%) and cheek (21.4%).
With respect to the surgical treatment, our study found that primary closure was the most common method for repairing defects in basal cell skin cancer and squamous cell skin cancer (85% and 60%, respectively). These results agree with the findings of Choi et al.,[1] who also found that primary closure was the most common method for repairing any surgical defect (38.9%), followed by a local flap (35.5%). The exception in our study was the case of melanoma, where the patient required a local flap based on facial aesthetic units.
The facial reconstruction of surgical defects after surgical excision of skin tumors based on facial aesthetic units is well described in the literature and recommended by various authors.[7] Russo et al.[7] published a guideline specifying which flap should be used in each cosmetic unit. They found that the flap with the highest score was the glabellar flap for defects of the medial canthus of the eye.[7] The flaps with the highest scores were the bilateral advancement flag flap or H flap for the forehead, the revolving-door flap for the auricle of the ear, the Mustardé flap for the infraorbital cheek, the O-Z rotation flap for the scalp, the Tenzel flap for the lower eyelid, and the island flap for the upper lip.[7] Although the classification of flaps provides clear knowledge of the flap properties, the existence of varied reconstructive options makes it necessary to have a systematic approach to analyze the patient and facial defect. The key points for facial reconstruction, according to Patel and Sykes,[2] are (1) analyze the facial defect and characterize the defect based on skin color, skin thickness, tissue composition, location, and subunits involved. If the defect involves more than 50% of the subunit, it is recommended the resection of the whole subunit as it may improve the aesthetic outcomes by camouflaging the incisions at the borders of the aesthetic subunits. (2) Once the defect is established, options for reconstruction should consider a graduated approach using the reconstructive ladder. The ladder from simplest to most complex approach is healing by secondary intention, primary closure, skin grafting, tissue expansion, local tissue transfer, distant tissue transfer, and free flap. (3) It is crucial to consider the surrounding anatomy and take into account the acceptable areas of tissue recruitment and consider facial landmarks that do not tolerate distortion. (4) Once the ideal areas for tissue recruitment have been chosen, flaps should be designed such that the scars rest within the relaxed skin tension lines and close parallel to the lines of maximal extensibility. Lastly, incisions designed along subunit borders should fall within the relaxed skin tension lines.[2]
Figure 3 shows a defect in the nasal region, which can traditionally be reconstructed with a bilobular flap[13]; however, lateral defects are not suitable, as flaps constructed in this way tend to lie across the cheek-to-nose concavity and obliterate this normal anatomic contour, thus creating a deformity that would defy satisfactory correction later.[13] Additionally, a poor flap design can cause tenting across the nasal cheek lines sometimes with pincushioning of the flap, a situation that cannot be corrected.[13] Therefore, it is more advantageous to make the reconstruction based on facial aesthetic units, with the advantage of obtaining better-camouflaged scars.
On the other hand, the defect shown in Figure 4 could have been traditionally reconstructed with an inferior rotation flap,[13] in which the flap is planned so that it rotates upward along the nasolabial fold. The disadvantage of this flap is a slight distortion of the palpebral opening and facial asymmetry. Even if the flap is well planned, the scar parallel to the lid margin may cause lid edema and ectropion, especially in younger patients. These limitations are reduced with the use of facial reconstruction based on aesthetic units.
Finally, Figure 6 shows a defect that could traditionally be reconstructed with a bilateral perialar crescentic advancement flap or with an Abbe flap,[13] with the disadvantage of obtaining a thick flap, a problem that is minimized when performing a reconstruction based on aesthetic units.
The advantage conferred by facial reconstruction based on aesthetic units is the incisions that perfectly camouflaged within the limits of the facial aesthetic units, as the flaps converge toward medial, either by advance, rotation, or interpolation. Another advantage is that, once designed, the incisions can be enlarged according to the need following the limits of the facial aesthetic units. Finally, the aesthetic results can be perceived from the beginning, even with the stitches placed.
CONCLUSIONS
In this study, we state that the most common skin cancer found in our population was basal cell skin cancer, followed by epithelial skin cancer and malignant melanoma. In general, the most frequent localization of these cancers was the nose. Moreover, in spite of primary closure being the most common method of reconstruction, a considerable number of patients required a facial reconstruction based on aesthetic facial units, whereby it is important to have clear concepts about this type of reconstruction, with satisfying results.
It is important to emphasize that we present the concept of facial reconstruction based on aesthetic units, with the idea that the patient’s concern is not the number of incisions or stitches made, but the naturalness of the aesthetic result. In a globalized world, demanding the aesthetic aspect, it is very important to offer the patient the possibility of reincorporating his/her daily activities in the quickest and most natural way possible.
Nevertheless, the results of this study do not represent the prevalence and we cannot extrapolate the results, as this study is a single-center analysis with a small number of patients. Therefore, it would be important that, in the future, results from other health centers should be studied together to get a general consensus.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
This study was self-funded.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Distribution of basal cell carcinoma and squamous cell carcinoma by facial esthetic unit. Arch Plast Surg. 2013;40:387-91.
- [Google Scholar]
- Concepts in local flap design and classification. Oper Tech Otolaryngol. 2011;22:13-23.
- [Google Scholar]
- Facial reconstruction after resection for cutaneous malignancies. Oper Tech Otolaryngol. 2013;24:36-44.
- [Google Scholar]
- Restoration of the face covering by means of selected skin in regional aesthetic units. Br J Plast Surg. 1956;9:212-21.
- [Google Scholar]
- Nasal reconstruction: Seeking a fourth dimension. Plast Reconstr Surg. 1986;78:145-57.
- [Google Scholar]
- The subunit principle in nasal reconstruction. Plast Reconstr Surg. 1985;76:239-47.
- [Google Scholar]
- Reconstruction techniques of choice for the facial cosmetic units. Actas Dermosifiliogr. 2017;108:729-37.
- [Google Scholar]
- Usefulness of the subunit principle in nasal reconstruction. An Bras Dermatol. 2017;92:159-62.
- [Google Scholar]
- A randomized trial of tailored skin cancer prevention messages for adults: Project SCAPE. Am J Public Health. 2010;100:735-41.
- [Google Scholar]
- A clinical study in malignant skin tumors. J Korean Soc Plast Reconstr Surg. 1982;9:377-88.
- [Google Scholar]
- A 10 year period (1968–1977) of clinical observation of cutaneous malignant tumors. Korean J Dermatol. 1978;16:19-29.
- [Google Scholar]
- Local flaps in head and neck reconstruction (1st ed.). St Louis, MO: Thieme Medical Publishers Inc; 2007.





