Translate this page into:
Far From Luck’s Way: A Concurrence of Kaposi Sarcoma and Cutaneous Angiosarcoma in the Setting of Chronic Lymphocytic Leukemia
Address for correspondence: Dr. Billur Sezgin, Department of Plastic Reconstructive and Aesthetic Surgery, Koc University School of Medicine, Topkapi, 342000 Istanbul, Turkey. E-mail: bsezgin@ku.edu.tr
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Kaposi sarcoma and cutaneous angiosarcoma are rare forms of skin malignancies that are vascular in nature and are frequently encountered in the immunosuppressed population. Although synchronous angiosarcoma and Kaposi sarcoma have been documented, to our knowledge, the coexistence of these vascular malignancies with underlying chronic lymphocytic leukemia has not been previously reported. A 51-year-old male patient with chronic lymphocytic leukemia presented with Kaposi sarcoma located on his left ankle. Shortly after, the patient presented with de novo lesions located on the plantar region of the right foot, reported as angiosarcoma. Following a multidisciplinary decision, treatment with adjuvant chemotherapy consisting of paclitaxel and carboplatin with consolidation radiotherapy was planned. The patient’s Kaposi sarcoma has remained unchanged throughout this period.
In such cases, the treatment is advised to be planned around the more aggressive malignancy. These patients should also be followed-up by dermatology due to the higher risk of secondary cutaneous malignancies.
Keywords
Angiosarcoma
chronic lymphocytic leukemia
cutaneous angiosarcoma
immunosuppression
Kaposi sarcoma
INTRODUCTION
Chronic lymphocytic leukemia (CLL) is a proliferative monoclonal B-cell disorder that constitutes the most common form of leukemia in adults. It accounts for 0.8% of all cancers and almost 30% of leukemic cancers.[1] The immunosuppressive molecules that are elaborated from B cells in patients with CLL, the downregulation of CD40 ligand expression on activated T cells, and altered granulocyte and T-cell function all contribute to the impaired immune system.[1] The impaired immune system lead to a high incidence of secondary malignancies. Acute leukemia, lung cancer, and skin cancer are among the reported secondary malignancies in CLL patients with increased risk in comparison to the normal population.[2] Cutaneous lesions other than skin cancers may also develop due to underlying CLL including varicella zoster, leukemia cutis, acute graft-versus-host disease, multiple warts, cutaneous drug eruptions, eosinophilic folliculitis, cutaneous T-cell lymphoma, and Merkel cell tumor.[3]
Cutaneous angiosarcoma is a vascular tumor with a very poor prognosis and high local relapse rates. Survival rate has been reported as 10%–15% in 5 years.[4] Types of cutaneous angiosarcoma include idiopathic angiosarcoma of the face and scalp; Stewart–Treves syndrome; and postradiation angiosarcoma. Angiosarcoma cases have been encountered in immunosuppressed patients.[5] The only potentially curative treatment is surgery with or without radiotherapy.
Kaposi sarcoma is an angioproliferative tumor, associated with human herpesvirus-8 (HHV-8). It has several types including immunosuppression-associated Kaposi sarcoma, which is seen in patients receiving immunosuppressive treatment and transplant patients.[6] Kaposi sarcoma treatment includes combination of surgical excision, local radiotherapy, and chemotherapeutics such as vinblastine, paclitaxel, and doxorubicin.
Both cutaneous angiosarcoma and Kaposi sarcoma have been reported individually as secondary tumors in patients with CLL.[78] Although synchronous angiosarcoma and Kaposi sarcoma have been documented, to our knowledge, the coexistence of these vascular tumors with underlying CLL has not been previously reported.[9] We hypothesized that the two different vascular tumors could be coincidentally present in the setting CLL. Here, we present a case of CLL, with consecutive diagnoses of Kaposi sarcoma and angiosarcoma 2 months apart.
CASE HISTORY
A 51-year-old male patient with a 2-year history of CLL was previously examined for a purple plaque located in the medial part of his left ankle [Figure 1] for which an incisional biopsy had revealed Kaposi sarcoma. The patient had been followed up without intervention and the lesion had remained stable for 3 years. In May 2018, a Positron Emission Tomography/Computed Tomography (PET-CT) reported new lesions in the plantar part of the opposite foot. The patient presented to our department 2 months later for these plantar lesions that showed fast growth over 3 weeks. Physical examination showed an exophytic vascular lesion with a diameter of 1.5 cm and two other millimetric dark purple lesions in the mid-plantar region of the right foot overlying a generalized ecchymotic area [Figure 2]. Lesions were excised with negative margins and the histopathological diagnosis was reported as spindle cell angiosarcoma [Figure 3]. Yet, in a duration of 1 month, new lesions started to form in the same location [Figure 4]. Generalized edemas of the right foot along with a reluctancy of healing in the incisional wounds were also noted. Following a multidisciplinary decision, further treatment with adjuvant chemotherapy consisting of monthly paclitaxel with a dose of 175 mg/m2 and carboplatin (AUC 5) with consolidation radiotherapy was planned. A total of six doses of chemotherapy were given where the patient received chemotherapy every 3 weeks for 3 months. Minimal side effects were noted (grade I). Since the patient had a partial response with a resolution of edema, healing of the incisional wounds, and no further lesions after the administration of chemotherapy, consolidation radiotherapy treatment at a total dose of 25 Gy was administered. The patient received five fractions twice a week along with a 5 Gy boost fraction at the location of the primary lesion. The patient has been followed up uneventfully for the past 6 months in regards to the angiosarcoma [Figure 5].

- Presentation of Kaposi sarcoma as a purple plaque located in the medial part of the patient’s left ankle

- Presentation of cutaneous angiosarcoma as an exophytic vascular lesion with a diameter of 1.5 cm and two other millimetric dark purple lesions on the right plantar region overlying a generalized ecchymotic area
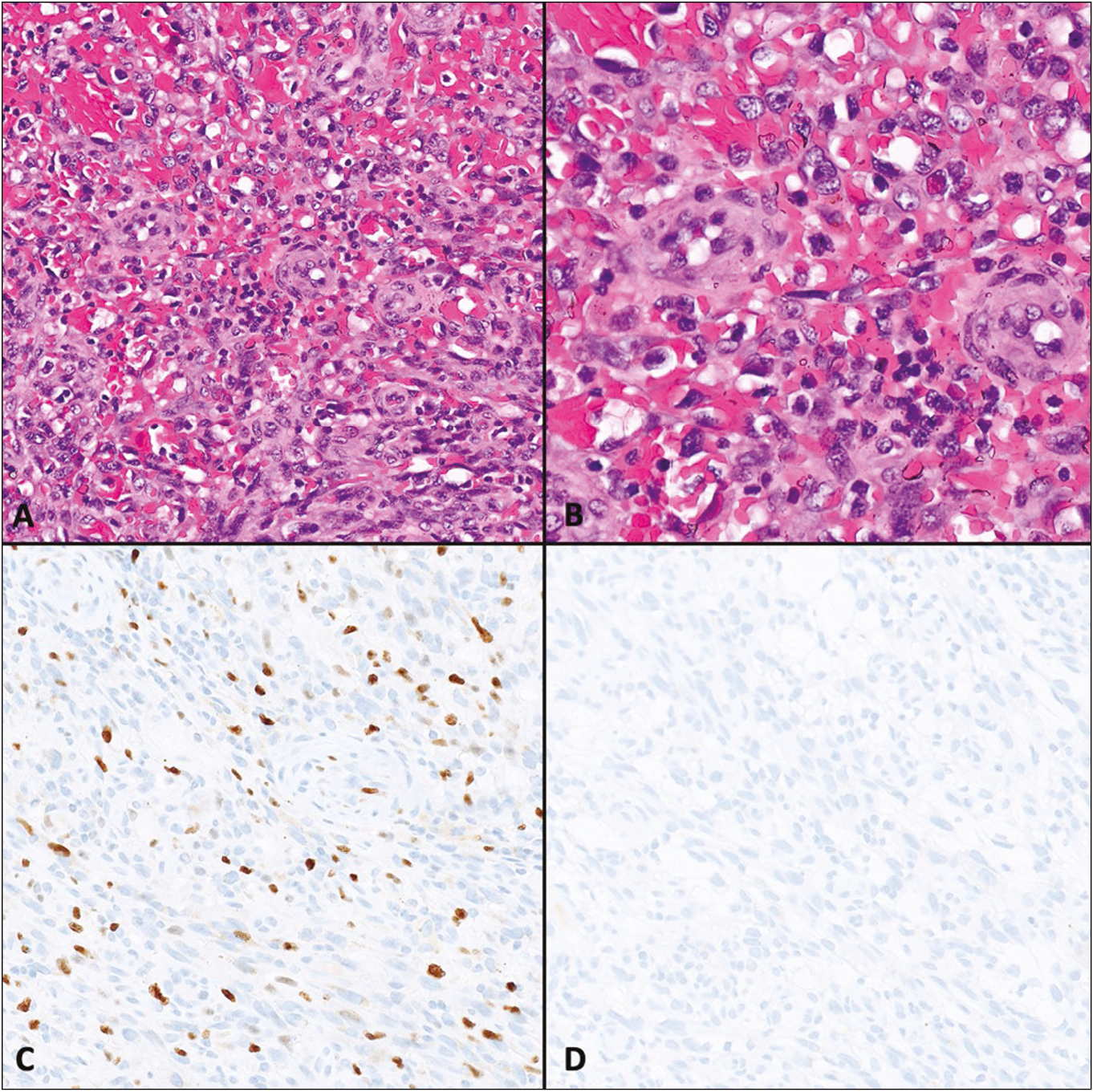
- Histomorphological features of the angiosarcoma on the right foot. Tumor is composed of spindle cell-forming slit-like spaces filled with erythrocytes. Note the prominent atypia and pleomorphism (A and B). Ki-67 proliferation index was high—20% (C). No immunoreactivity was observed with antibody against HHV-8 (D)

- Appearance of new dark purple lesions on the right foot a month after the excision of the primary lesions

- Posttreatment 6-month follow-up of the patient’s right plantar region
The patient’s Kaposi sarcoma has also been treated with radiotherapy with a total dose of 32 Gy. The treatment was administered at four fractions, with a weekly fraction of 8 Gy per week. The formation of a very small millimetric vascular nodule on the patient’s right thumb was also biopsied with excision and was diagnosed as Kaposi sarcoma [Figure 6]. This area was also treated under the same radiotherapy protocol. The lesions have been followed up and have remained the same throughout this period.
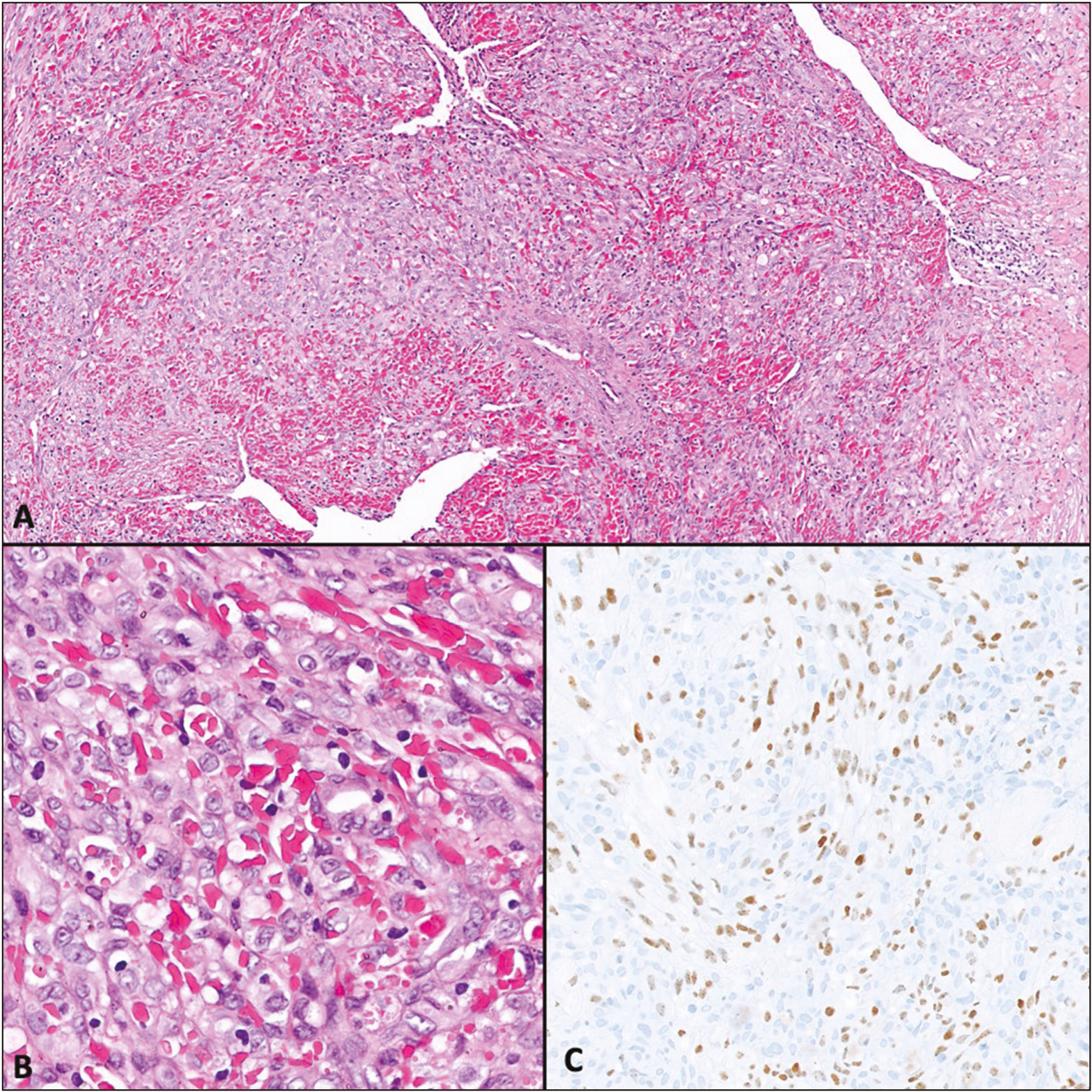
- Histomorphological features of the Kaposi sarcoma. This tumor is also composed of spindle cell-forming slit-like spaces filled with erythrocytes. Tumor cells have slight atypia and no pleomorphism (A and B). Note the diffuse positivity with the antibody against HHV-8 (C)
DISCUSSION
The accumulation of functionally incompetent lymphocytes along with immunosuppressive agents for the treatment of CLL disrupts the immune system and leads to high incidences of secondary malignancies, including skin cancers, such as melanoma and squamous cell carcinoma (SCC).[2] According to Mehrany et al.,[10] SCC has an increased metastasis and mortality rate in patients with CLL; therefore, it behaves more aggressively. Therefore, routine follow-up by dermatology is strongly recommended for these patients.
Although both Kaposi sarcoma and angiosarcoma are rare vascular tumors, they have been reported individually in patients with CLL. Angiosarcoma is a malignant tumor that is composed of spindle cells that show prominent atypia, brisk mitotic activity, and high Ki-67 proliferation index. Angiosarcomas are not associated with HHV-8. On the contrary, neoplastic cells of Kaposi sarcoma are relatively monomorphic with no prominent pleomorphism and atypia. Moreover, Kaposi sarcoma is almost always associated with HHV-8.
The coexistence of these two vascular tumors with underlying CLL is a unique situation that requires a different treatment strategy. Kaposi sarcoma is a rare borderline angioproliferative tumor that is mostly seen in immunocompromised patients, especially patients with HIV. In Kaposi sarcoma, surgery is usually performed for palliative purposes. Local cryotherapy, radiation therapy, and intralesional chemotherapeutics are other treatment options.[11]
On the contrary, angiosarcoma affects many tissues and organs but the most commonly affected organ is the skin. Cutaneous angiosarcoma is a rare aggressive vascular tumor and its widely accepted treatment is wide excisional surgery with clear margins and postoperative radiotherapy. Radical surgery and postoperative chemoradiotherapy is another option and literature studies have reported a decrease in mortality with adjuvant chemotherapy.[12] As for chemotherapy, taxanes have shown to be effective.
Compared to Kaposi sarcoma, the coexistence of angiosarcoma and CLL is a rarer manifestation. Angiosarcoma has a higher mortality rate and is more aggressive; therefore, the treatment should be focused on cutaneous angiosarcoma.
CONCLUSION
Kaposi sarcoma and cutaneous angiosarcoma are rare forms of skin malignancies that are vascular in nature and are frequently encountered in the immunosuppressed population. To the best of our knowledge, this is the first report of the coexistence of these vascular malignancies with underlying CLL. In such cases of concurrent malignancies, treatment should be planned and staged according to the potential of aggressivity. The multidisciplinary follow-up of CLL patients must include routine dermatological examinations in order to facilitate early recognition and treatment of malignant skin lesions.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Risk of second cancer after chronic lymphocytic leukemia. Int J Cancer. 2007;121:151-6.
- [Google Scholar]
- Cutaneous findings in chronic lymphocytic leukaemia. Br J Dermatol. 2004;150:1129-35.
- [Google Scholar]
- Kaposi sarcoma and cutaneous angiosarcoma: guidelines for diagnosis and treatment. Actas Dermosifiliogr. 2018;109:878-87.
- [Google Scholar]
- Angiosarcoma in a chronically immunosuppressed renal transplant recipient: report of a case and review of the literature. Am J Dermatopathol. 2002;24:330-5.
- [Google Scholar]
- Immunosuppressive therapy and Kaposi’s sarcoma after kidney transplantation. Transplant Proc. 2004;36:168-70.
- [Google Scholar]
- A rare coexistence––chronic lymphocytic leukemia and Kaposi sarcoma: case report and review of the literature. J Cancer Res Ther. 2015;11:954-6.
- [Google Scholar]
- Angiosarcoma treated successfully with anti-PD-1 therapy: a case report. J Immunother Cancer. 2017;5:58.
- [Google Scholar]
- A patient with classical Kaposi’s sarcoma and angiosarcoma: bad luck or a common aetiology? Clin Oncol (R Coll Radiol). 1997;9:186-8.
- [Google Scholar]
- Increased metastasis and mortality from cutaneous squamous cell carcinoma in patients with chronic lymphocytic leukemia. J Am Acad Dermatol. 2005;53:1067-71.
- [Google Scholar]
- An update on Kaposi’s sarcoma: epidemiology, pathogenesis and treatment. Dermatol Ther (Heidelb). 2016;6:465-70.
- [Google Scholar]
- Metastatic angiosarcomas: doxorubicin-based regimens, weekly paclitaxel and metastasectomy significantly improve the outcome. Ann Oncol. 2012;23:517-23.
- [Google Scholar]






