Translate this page into:
Platelet-rich Fibrin in Nonhealing Leg Ulcers: A Simple and Effective Therapeutic Option
Address for correspondence: Dr. Surabhi Sinha, Department of Dermatology, Dr Ram Manohar Lohia Hospital and Atal Bihari Vajpayee Institute of Medical Sciences, New Delhi 110001, India. E-mail: surabhi2310@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
Nonhealing ulcers can occur due to a variety of causes and are associated with high morbidity, expensive, and prolonged treatment. We conducted this study to determine the efficacy of autologous platelet-rich fibrin (PRF) in nonhealing ulcers in various disorders, which is a very cost-effective and safe treatment option.
Materials and Methods:
Eighteen patients with nonhealing leg ulcers were included. The ulcers were treated with PRF at weekly intervals. The response to treatment was recorded by calculating the area of ulcer at baseline and at every subsequent visit till the ulcers healed.
Results:
The study included 18 patients of nonhealing leg ulcers due to leprosy (n = 6), neuropathic ulcer (n = 4), venous ulcer (n = 3), diabetic foot ulcer (n = 2), post-traumatic ulcer (n = 2), and post-full-thickness skin graft ulcer (n = 1). The mean size of the ulcers was 8.44 cm2 and mean duration was 5.55 months. The mean age of the patients was 40.5 years. The minimum and the maximum sittings required were three and nine, respectively (mean 5). No adverse events were noted.
Conclusion:
The treatment of nonhealing ulcer with PRF is an easy, safe, simple, and cost-effective method.
Keywords
Cost-effective
nonhealing leg ulcers
platelet-rich fibrin
INTRODUCTION
Nonhealing ulcers are ulcers that fail to heal through the normal, orderly, and timely sequence of repair.[1] The causes are manifold and include diabetes, venous stasis, vasculitis, trauma, trophic changes, and infections, most notably Hansen’s disease in the Indian scenario. Their prevalence is on the rise due to higher life expectancy and sedentary lifestyle. They are a cause of significant morbidity and associated with high treatment costs. Recently, platelet concentrates, containing various growth factors secreted by platelets, have been used to promote wound healing, especially in oral and maxillofacial surgery.[23] Autologous platelet‑rich fibrin (PRF) is an easily prepared, safe platelet concentrate that has been reported to be effective in nonhealing ulcers of certain specific etiologies.[4] We report a series of 18 patients with nonhealing leg ulcers treated with PRF who achieved complete healing of ulcers.
MATERIALS AND METHODS
Patient selection
Eighteen patients with nonhealing leg ulcers of more than 8 weeks duration that had failed conventional treatments were recruited after written informed consent. Patients with bleeding diathesis and hematological disorders, platelet counts <1 lakhs/mm3, on anticoagulants (aspirin, warfarin, heparin), pregnant and lactating women, severe hypoproteinemia (<6g/dL), and deep ulcers with exposed bone, muscle, or tendon were excluded from the study.
Methodology
Detailed history was taken and examination was performed in all patients. Under aseptic precautions 10mL of venous blood was drawn in a plain vial. The vial was then immediately subjected to centrifugation at the speed of 2000rpm for 10 min. Three layers were obtained after centrifugation, comprising the upper straw colored platelet poor plasma, middle portion containing PRF, and the lower sediment of red blood cells (RBCs). The ulcer was then thoroughly cleaned with normal saline and betadine solution. The PRF was separated along with 1-mm-thick layer of RBCs by using a sterile forceps and blade, and placed over a piece of sterile gauze. The PRF was then placed over the ulcer with the help of a sterile jeweler’s forceps after which the wound was dressed with a nonadhesive dressing and sterile roller bandage. The patients were advised bed rest with avoidance of weight bearing over the treated leg for 1–2 days. The bandage was removed and changed at next sitting. Two patients with diabetes were prescribed oral antibiotics for the initial two sittings, as the ulcers were secondarily infected at baseline.
PRF was applied at weekly intervals and the ulcer area was assessed at every visit. The percentage reduction in the area was documented and weekly sittings of PRF therapy were performed till adequate response [Figures 1–3]. The size of the ulcer was measured by tracing the outline of the ulcer over a transparency sheet. The area was then calculated by superimposing a graph paper over the transparency as described by Oien et al.[5]

- (A) Post-graft ulcer on the dorsum of foot before treatment. (B) Ulcer after second sitting of PRF. (C) Ulcer after third sitting of PRF. (D) Healed ulcer after fifth sitting of PRF
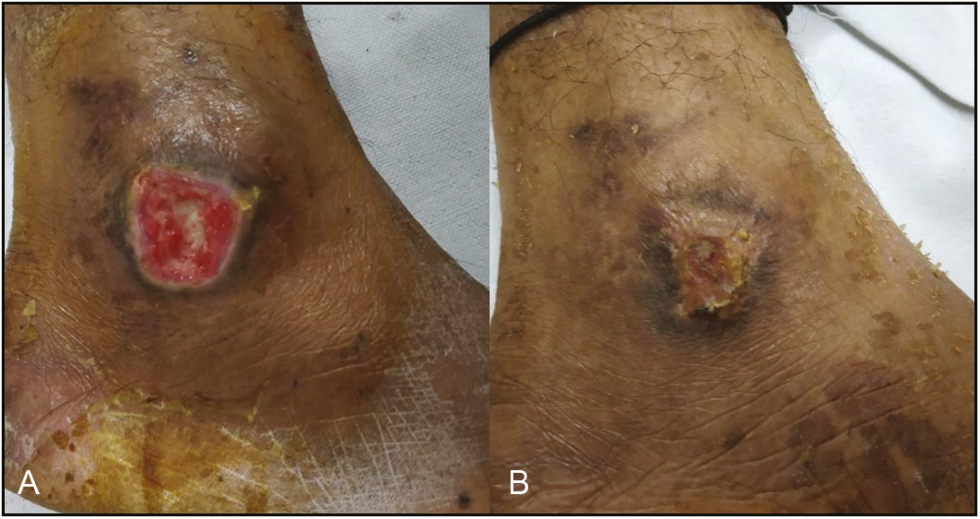
- (A) Diabetic ulcer on the lateral malleolus before treatment. (B) Ulcer after fourth sitting of PRF

- (A) Trophic ulcer on the big toe before treatment. (B) Ulcer after first sitting of PRF. (C) Ulcer after second sitting of PRF. (D) Ulcer after third sitting of PRF
RESULTS
Eighteen patients with chronic leg ulcers of various etiologies were included: leprosy (n = 6), followed by neuropathic (n = 4), venous (n = 3), diabetic foot (n = 2), post-traumatic (n = 2), and post-full-thickness skin graft (n = 1). Demographic details of the patients are listed in Table 1.
| Conditions | Age (years) | Sex | Duration (months) | Site | Area (cm2) |
|---|---|---|---|---|---|
| Trophic ulcer (Hansen’s disease) | 34 | Male | 3 | Heel of left foot | 6 |
| 29 | Female | 4 | Planter aspect of right foot | 6 | |
| 31 | Female | 5 | Big toe right foot | 2 | |
| 40 | Female | 3.5 | Lateral aspect of left foot | 4 | |
| 42 | Female | 7 | Big toe right foot | 6 | |
| 37 | Male | 5 | Planter aspect of right foot | 8 | |
| Neuropathic ulcer | 30 | Female | 6 | Heel of right foot | 16 |
| 40 | Female | 9 | Lateral malleoli left | 4 | |
| 38 | Female | 8 | Lateral aspect of left foot | 4 | |
| 41 | Female | 10 | Planter aspect of left foot | 3 | |
| Venous ulcer | 50 | Male | 4 | Medial aspect of right leg | 15 |
| 48 | Male | 3 | Medial aspect of right leg | 6 | |
| 53 | Male | 5 | Medial aspect of left leg | 9 | |
| Diabetic foot ulcer | 55 | Male | 12 | Below the lateral malleoli | 32 |
| 40 | Male | 6 | Medial malleoli of right | 6 | |
| Post-graft ulcer | 45 | Male | 4 | Dorsum of left foot | 15 |
| Post-traumatic ulcer | 40 | Male | 2.5 | Lateral malleoli right | 6 |
| 36 | Female | 3 | Lateral malleoli right | 4 |
There were nine men and nine women. One patient was lost to follow-up after the fifth sitting.
The sites involved by the ulcers are mentioned in Table 1. At initial presentation, the mean size of the ulcers was 8.44 cm2 (range, 2–32 cm2) and mean duration was 5.55 months (3–12 months). The mean age of the patients was 40.5 years (range, 29–55).
The only adjuvant treatment was a course of antibiotics given to two patients with diabetic ulcers. The ulcers of the 16 patients who were nondiabetic completely healed in 3–7 weeks and those of the two patients with diabetes healed in 7 and 9 weeks. The mean number of sittings required for complete healing of the ulcer was 5 (3–9) [Table 2].
| S. no. | Area (cm2) at first visit | Area (cm2) at second visit | Area (cm2) at third visit | Area (cm2) at fourth visit | Area (cm2) at fifth visit | Area (cm2) at sixth visit | Area (cm2) at seventh visit | Area (cm2) at eighth visit | Area (cm2) at ninth visit | Area (cm2) at tenth visit |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. | 6 | 4 | 2 | 1 | 0 | |||||
| 2. | 6 | 4 | 3 | 2.25 | 1 | 0 | ||||
| 3. | 2 | 1 | 0.5 | 0 | ||||||
| 4. | 4 | 2 | 1.5 | 0.5 | 0 | |||||
| 5. | 6 | 4 | 2 | 0.5 | 0 | |||||
| 6. | 8 | 6 | 3 | 1.5 | 0.5 | |||||
| 7. | 16 | 12 | 9 | 7.5 | 4 | 1.5 | 1 | 0 | ||
| 8. | 4 | 3 | 1.5 | 0.5 | 0 | 0 | ||||
| 9. | 4 | 3 | 2 | 1.5 | 1 | 0 | ||||
| 10. | 3 | 2 | 1 | 0.5 | 0 | |||||
| 11. | 15 | 12 | 8 | 6 | 3.75 | 2 | 1 | 0 | ||
| 12. | 6 | 3 | 1.5 | 0.5 | 0 | |||||
| 13. | 9 | 6.25 | 4 | 3 | 1 | 0 | ||||
| 14. | 32 | 26.25 | 21 | 18 | 10 | 8 | 4.5 | 2 | 1 | 0 |
| 15. | 6 | 4 | 2 | 1 | 0.5 | 0 | ||||
| 16. | 15 | 12 | 9 | 6 | 3 | 1.5 | 0.5 | 0 | ||
| 17. | 6 | 4 | 3 | 1.5 | 1 | 0 | ||||
| 18. | 4 | 2.25 | 1.5 | 1 | 0.5 | 0 |
Ulcers with size larger than 15 cm2 or require 7 or more sitting have been marked as bold
None of our patients experienced any adverse event or recurrence during the 3 months follow-up period. However, proper aseptic precautions are important during the dressing. There was partial recurrence at the same site in one patient after 6 months after a period of prolonged outstation travel. We also noticed that the number of weeks in which an ulcer healed was proportionate to the original size of the ulcer.
DISCUSSION
Wound healing occurs through three intrinsically regulated sequential phases: inflammation, proliferation, and maturation. Nonhealing ulcers are believed to get stuck in the inflammation phase leading to a delay in the healing process.[6] The premise behind using platelet concentrates is to nudge the ulcers out of the inflammation phase into the next phase of wound healing using the growth factors.
Nonhealing wounds are a frequent problem in developing countries and are a challenge both for healthcare providers and patients. The conventionally used methods such as dressings and debridement do not provide the necessary growth factors and often prove unsuccessful in such ulcers. Knighton et al.[7] had first shown that locally acting factors derived from autologous blood promote healing of chronic ulcers. Platelet-rich plasma (PRP) has been tried by a few authors but a Cochrane review concluded that PRP did not significantly hasten the healing time and larger adequately powered studies are needed before it can be recommended. Dohan Ehrenfest et al.[8] compared PRP and PRF in ulcer and significant differences were observed in the in vitro biological behavior of the two products. PRF has been shown to be superior to PRP in nonhealing ulcers. The advantages of PRF over PRP are summarized in Table 3.
| 1. | The procedure is easy and less time-consuming |
| 2. | The procedure is painless as no need to inject the sample |
| 3. | Lack of biochemical modification as no anticoagulants are needed |
| 4. | The method preparation and application is simple and is cost- effective process |
| 5. | Long‑term effect––growth factors are released slowly over a period of 7 or more days |
| 6. | Able to support cytokines enmeshment and cellular migration |
| 7. | Increased incorporation of the circulating cytokines in the fibrin meshes (intrinsic cytokines) |
| 8. | It supports and accelerates the healing process due to slow polymerization |
| 9. | Helps in hemostasis |
| 10. | Three‑dimensional structure gives elasticity and flexibility to PRF membrane |
PRF is a second-generation platelet concentrate, prepared from centrifuged blood. It was first developed in France by Choukroun et al.[9] PRF has been used by different authors for nonhealing ulcers of various etiologies: leprosy, pyoderma gangrenosum, diabetic ulcers, scleroderma ulcer, and leg ulcer.[4101112131415]
It has been shown to have a high concentration of platelets as they get trapped in the fibrin mesh. Fibrin, the activated form of fibrinogen, is abundantly present both in plasma and in the platelet α-granules, and plays a key role in platelet aggregation during hemostasis. The beneficial effect of PRF can be explained by its high concentration of platelets and leukocytes and slow progressive release of growth factors from the fibrin matrix.[8]In vitro studies have proven that PRF releases various growth factors from fibrin matrix for at least 7 days.[816] These growth factors include platelet-derived growth factor, transforming growth factor β1, vascular endothelial growth factor, and insulin-like growth factors. PRF also contains matrix glycoproteins, such as thrombospondin-1, fibronectin and vitronectin, and various cytokines.[816] PRF has also been shown to behave like living tissue and hence can be considered as tissue graft for cutaneous wounds.[15] The high concentration of leucocytes present in PRF adds to the efficacy by preventing infections.[17] An added advantage of PRF is that it can be used in patients with a wide range of comorbidities: diabetes, vascular compromise, and neuropathy.
In our study, the mean number of sittings at which complete healing of ulcer seen was 5, that is, 5 weeks. A similar finding was described by Sarvajnamurthy et al.,[18] where they found that the mean duration of the healing of the chronic ulcers using PRP or PRF was in 5.1 weeks. We also found significant reduction in size of ulcer after the third sitting, which is in consonance with previous studies.[210,19] PRF thus significantly reduce the time, cost of therapy, and associated morbidity of the disease. Notably all the 18 of our patients observed complete healing of the ulcers, which was maintained in all till the end of the follow-up period of 3 months. However, larger ulcers were seen to require larger number of sitting.
In summary, PRF can be used to treat chronic or nonhealing ulcers and a minimum of three to four sittings should be given to aid in the healing of such ulcers. But, complete healing depends on initial ulcer size. Further studies with larger sample size and a longer follow-up period would be helpful in ascertaining this cheap and effective modality in the management of nonhealing ulcers.
CONCLUSION
The use of PRF can induce and significantly hasten healing of chronic ulcers and reduce the disease burden. It is an inexpensive, easily available, and quick modality and can be incorporated in the therapeutic armamentarium for a wide range of etiologies of nonhealing ulcers.
Acknowledgement
We would like to thank all the postgraduate juniors for their valuable contribution during the study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Challenges in the treatment of chronic wounds. Adv Wound Care (New Rochelle). 2015;4:560-82.
- [Google Scholar]
- Cascade® autologous system platelet-rich fibrin matrix in the treatment of chronic leg ulcers. Adv Wound Care (New Rochelle). 2012;1:52-5.
- [Google Scholar]
- Use of autologous platelet-rich fibrin on hard-to-heal wounds. J Wound Care. 2008;17:60-3.
- [Google Scholar]
- Use of an autologous leucocyte and platelet-rich fibrin patch on hard-to-heal DFUs: A pilot study. J Wound Care. 2015;24:172-4, 176-8.
- [Google Scholar]
- Measuring the size of ulcers by planimetry: A useful method in the clinical setting. J Wound Care. 2002;11:165-8.
- [Google Scholar]
- Inflammation. 2: Its role in the healing of chronic wounds. J Wound Care. 2002;11:245-9.
- [Google Scholar]
- Classification and treatment of chronic nonhealing wounds. Successful treatment with autologous platelet-derived wound healing factors (PDWHF) Ann Surg. 1986;204:322-30.
- [Google Scholar]
- Do the fibrin architecture and leukocyte content influence the growth factor release of platelet concentrates? An evidence-based answer comparing a pure platelet-rich plasma (P-PRP) gel and a leukocyte- and platelet-rich fibrin (L-PRF) Curr Pharm Biotechnol. 2012;13:1145-52.
- [Google Scholar]
- Autologous platelet-rich fibrin matrix in non-healing trophic ulcers in patients with Hansen’s disease. J Cutan Aesthet Surg. 2017;10:3-7.
- [Google Scholar]
- Autologous platelet-rich fibrin in treatment of scleroderma ulcer. Int Wound J. 2016;13:1065-6.
- [Google Scholar]
- Leucocyte- and platelet-rich fibrin (L-PRF) as a regenerative medicine strategy for the treatment of refractory leg ulcers: A prospective cohort study. Platelets. 2018;29:468-75.
- [Google Scholar]
- Treatment of a chronic cutaneous surgical wound with platelet-rich fibrin. Dermatol Surg. 2018;44:449-52.
- [Google Scholar]
- Management of facial pyoderma gangrenosum using platelet-rich fibrin: A technical report. J Oral Maxillofac Surg. 2018;76:1460-3.
- [Google Scholar]
- L-PRP/L-PRF in esthetic plastic surgery, regenerative medicine of the skin and chronic wounds. Curr Pharm Biotechnol. 2012;13:1266-77.
- [Google Scholar]
- The role of leukocytes from L-PRP/L-PRF in wound healing and immune defense: New perspectives. Curr Pharm Biotechnol. 2012;13:1153-62.
- [Google Scholar]
- Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part III: Leucocyte activation: a new feature for platelet concentrates? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e51-5.
- [Google Scholar]
- Autologous platelet rich plasma in chronic venous ulcers: study of 17 cases. J Cutan Aesthet Surg. 2013;6:97-9.
- [Google Scholar]
- Efficacy of autologous platelet-rich fibrin in chronic cutaneous ulcer: A randomized controlled trial. Indian J Clin Exp Dermatol. 2017;3:172-81.
- [Google Scholar]






