Translate this page into:
Outcome of Recurrent Auricular Keloid Treatment with a Combination of Surgical Excision and Perioperative Corticosteroid Injection
Address for correspondence: Dr Mohammed Abd-Alhussein Aljodah, Department of Surgery, Al-Kindy College of Medicine, University of Baghdad, Medical Post Office Box 61314, Medical City, Baghdad, Iraq. E-mail: mohammedaljodah@kmc.uobaghdad.edu.iq
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
Auricular keloids that occur after ear piercing or other traumas can challenge surgeons as recurrence is frequent; there has been no consensus about the best management protocol. Surgical excision combined with perioperative corticosteroid injections is frequently used as first-line therapy, but recurrent auricular keloids are usually shifted to a combination of radiotherapy and surgical excision.
Objectives:
The objective is to evaluate the rate of recurrence when recurrent auricular keloids are treated with surgical excision with perioperative corticosteroid injections.
Materials and Methods:
Between February 2017 and January 2020, 41 patients (52 auricles) with recurrent auricular keloids were treated by extralesional keloid excision combined with five corticosteroid steroid injections (two preoperative, one intraoperative, and two postoperative doses). Recurrence was recorded if the surgical scar showed hypertrophy or started to rise above the level of the margins.
Results:
The mean postoperative follow-up was 13.04 months (ranging from 6 to 24 months). Recurrence was recorded in five auricles (9.6%) during the follow-up period.
Conclusion:
Perioperative corticosteroid injections combined with surgical excision of auricular keloids are still a valid option in recurrent cases, and it is a useful choice when radiotherapy facilities are limited.
Keywords
Auricle
excision
intralesional injection
keloid
triamcinolone acetonide
INTRODUCTION
Keloid development following ear piercing or surgical trauma is both an aesthetic and psychological concern for patients. Management is challenging because of possible recurrence and exacerbation by surgical manipulation. There is no consensus about the best management modality. Keloid incidence is about 2.5% following ear piercing.[1] Surgical excision of keloid can be disappointing, as the recurrence rate may reach 100% in some cases.[2] Many adjuvant treatment modalities have been promoted to improve the outcome when combined with surgical excision, but the results have been variable. Perioperative corticosteroid injection, postoperative compression therapy, and radiotherapy are common methods. Each modality has pros and cons, but some studies have reported zero recurrences of keloid scarring following the use of perioperative corticosteroid injection.[34]
Radiotherapy is usually preferred for recurrent keloids after the failure of other treatment modalities.[5] Minimal information has been reported in the literature about the outcome of treating recurrent auricular keloids. Most of the studies involve either primary keloids or a mixture of primary and recurrent keloids. In this study, we use the term “primary keloid” to indicate keloids that develop following primary insult and “secondary keloid” for those that arise after surgical resection of a primary keloid. The aim of this study is to prospectively evaluate the outcome of treating secondary keloids by a combination of surgical excision and perioperative corticosteroid injections.
MATERIALS AND METHODS
Study sample
This prospective study was conducted in the surgical unit of Al-Kindy Hospital, a teaching hospital, from February 2017 to January 2020. During this time, 41 participants (52 auricles) presented with recurrent auricular keloid scars following previous surgical excision performed outside our facility by surgeons not associated with our surgical unit. Each participant underwent the protocol of surgical excision combined with preoperative, intraoperative, and postoperative corticosteroid injections after a full clinical assessment and necessary laboratory tests. A checklist was used to determine anatomical location, keloid duration, keloid dimensions, and previous surgical intervention date. Inclusion criteria were patients with recurrence of auricular keloid after previous surgery for excision of a primary keloid. Exclusion criteria were patients who received keloidal corticosteroid injections within the previous 6 months or had a history of radiotherapy for treatment of keloids.
The protocol involved five steroid injections (two preoperative, one intraoperative, and two postoperative). The interval between injections was 1 month, making the total duration of the intervention 4 months. After the operation, all patients were seen after 7 days, and sutures were removed according to signs of healing. All patients were followed up post-operatively for at least 6 months, and recurrence was recorded if the surgical scar showed hypertrophy or started to rise above the level of the margins and if the operative area became thicker than adjacent tissue at any time during the follow-up period.
Injections and operative techniques
Extralesional keloid excision was marked along the keloid border in the adjacent normal-looking skin [Figure 1]. All operations were done under local anesthesia infiltration. The intraoperative infiltration solution was prepared by mixing 1 cc of a 40 mg/cc triamcinolone acetonide suspension with 1 cc of xylocaine 1% with adrenaline (epinephrine) at a rate of 1:200,000. The same solution preparation method was used for preoperative and postoperative injections. The entire lesion was excised meticulously to remove all scarring and to avoid perforation of anterior skin. Primary wound closure was achieved with 6-0 polypropylene suture. The wound was covered with Fucidin ointment (LEO Laboratories Ltd, Berkshire, UK) and a lightly compressive sterile gauze dressing that was removed after 48 h. A 27 G × ½″ hypodermic needle with a 1 cc Luer-Lock syringe was used for the intraoperative and postoperative injections, whereas a 23 G × 1″ needle with a 1 cc Luer-Lock syringe was used for the two preoperative injections to facilitate infiltration of tough keloid tissue.

- Patient with recurrent earlobe keloid. A and B. Preoperative picture. C. Excision of the keloid. D and E. After 6 months with no signs of recurrence
Data collection and analysis
Collected data were loaded into the IBM SPSS Statistics for Windows, Version 24.0 program (IBM Corp., Armonk, NY, USA). Data were presented using tables. Numerical data were presented using mean ± SD or medians and ranges if not normally distributed, whereas percentages were used for categorical data.
RESULTS
Forty-one female participants (52 auricular keloids) were included in this study with an age range of 15–37 years, all of whom were experiencing recurrent auricular keloids after a previous excision. The keloids were located in the earlobe in 42 participants (80.8%) in the study sample, and 10 keloids (19.2%) were in the auricular helices. There were 21 right-sided keloids and 31 left-sided keloids. The keloids were measured, and the longest diameters of each ranged from 0.8 to 4 cm.
The median duration of keloids before surgery was 24 months (ranging from 9 to 36 months). The previous treatment modalities provided elsewhere to the participants before being included in this study were: excision alone in 35 participants (67.3%), excision followed by any technique of compression therapy in nine participants (17.3%), and excision combined with corticosteroid injection in eight participants (15.4%). The majority of patients, 44 (84.6%), had a single previous excision, whereas the remaining eight (15.4%) reported more than one attempt at excision. The mean length of all cases was 13.04 months (ranging from 6 to 24 months). Healing was uneventful for all participants after surgery, but two auricles (3.8%) showed partial dehiscence after removal of stitches, and complete healing was achieved by local wound care within an additional 5 days. Recurrence was recorded in five (9.6%) auricles during the follow-up period that started 4 months postoperatively. A summary of the above is presented in Table 1.
| Number of auricles | n = 52 |
|---|---|
| Number of patients | 41 (29 unilateral + 12 bilateral) |
| Age (years) | Median (range) |
| 29 (15–37) | |
| Location | |
| Helix | 10 (19.2%) |
| Earlobe | 42 (80.8%) |
| Duration before presentation (months) | 24 (9–36) |
| Previous treatment | |
| Excision | 35 (67.3 %) |
| Excision + compression | 9 (17.3%) |
| Excision + corticosteroid | 8 (15.4 %) |
| Frequency of previous excisions | |
| One time | 44 (84.6%) |
| More than one time | 8 (15.4%) |
| Follow-up (months) | Mean ± SD |
| 13.04 ± 6.50 | |
| Recurrence | N = 5 (9.6%) |
DISCUSSION
Keloids following ear piercing or other ear traumas represent fertile soil for research. The literature is rich with articles about treatment modalities, although variable results after using the same technique have led to elusive conclusions, and no consensus exists about the best treatment protocol.[6] Corticosteroid injection is a well-known keloid treatment modality, and the mechanism of action may be inhibition of fibroblast proliferation, collagen synthesis, and suppression of inflammation.[78] It is simple, cost-effective, and has low morbidity.
Radiotherapy is another adjuvant therapy for keloid management, which has a possible mechanism of destroying fibroblasts, connective tissue stem cells, and acute inflammatory cells.[9] Cost and possible side effects are the reasons that it is used mainly in recurrent keloids.[5]
Compression therapy is another modality that achieves good results with minimal side effects when combined with surgical resection. The mechanism of action is unknown, but it is hypothesized that altered wound tension and pressure-induced localized hypoxia play a role in the prevention of keloid recurrence. Poor patient compliance and early recurrence after withdrawal are considered its main limitations.[10] Multimodality therapeutic protocols provide better results in keloid management.[6] Although auricular keloids are extensively described in the literature, only a few studies are specific about studying secondary keloids. Secondary keloids have a high risk of recurrence.[11] However, treatment of primary keloids is more promising; some studies reported zero recurrences after surgical resection of primary earlobe keloids when it was combined with perioperative and intraoperative corticosteroid injections.[4]
A study by Aluko-Olokun et al.[3] found that preoperative corticosteroid injections were not necessary and did not improve results when intraoperative and postoperative corticosteroid injections were used as adjuvant therapy with surgical resection in primary earlobe keloids. A study by Rosen et al.[5] proposed that intraoperative corticosteroid injection was the most important dose for preventing keloid development. Variable results were reported about secondary keloid management when using a combination of surgical excision and corticosteroid injections; higher recurrences were reported in studies that omitted preoperative corticosteroid injections. Rosen et al.[5] reported six recurrences of 15 secondary keloids (40%) when only intraoperative and postoperative corticosteroid injections were combined with surgical resection; however, the data did not reach statistical significance when compared with the recurrence of primary keloids treated with the same protocol in that study. Sclafani et al.[12] also reported earlobe keloid recurrence of approximately 33% in a mixed primary and secondary keloid sample after a combination of surgery and postoperative corticosteroid injections. Some studies reported fewer recurrences when preoperative corticosteroid injections were given in addition to intraoperative and postoperative doses. A study by Carvalhaes et al.[13] reported less than 6% recurrence after using preoperative steroids on a mixed sample of primary and secondary keloids. Jung et al.[14] reported no recurrences in four secondary keloid patients after application of preoperative and postoperative corticosteroid injections. However, 16.6% recurrence rate was reported in the mixed sample, but only in primary keloid cases.
The variable results reported in the literature about secondary auricular keloid management and the number of patients with secondary auricular keloids in the researcher’s country revealed an opportunity to prospectively evaluate the outcome of combined surgery and perioperative corticosteroid injections on secondary keloid cases.
All participants included in this study received two preoperative corticosteroid injections 1 month apart. A triamcinolone acetonide suspension concentration of 20 mg/mL has been reported to be effective for keloid treatment.[13] In this study, only five patients (9.6%) exhibited recurrence during the follow-up period. This recurrence happened after the fourth month of postoperative follow-up in one participant, and the remaining four cases recurred after one year. All five participants responded well to additional steroid injections. This low recurrence could be related to preoperative corticosteroid injections or due to the limited follow-up period (6–24 months). However, the recurrence rate did not exceed the reported rates in studies that used adjuvant radiotherapy to treat secondary keloids. The use of perioperative radiotherapy in secondary keloids does not make them immune to recurrence; a study by Stahl et al.[11] reported a 27% recurrence rate after application of preoperative and postoperative radiotherapy in secondary keloid cases. Sclafani et al.[12] also reported a recurrence of approximately 12.5% in their comparative study, which included a mixed sample of primary and secondary keloids. In another study, Ollstein et al.[15] reported a 21% recurrence after intralesional excision and postoperative radiotherapy.
A meta-analysis by Shin et al.[16] found that there were no significant differences in recurrence rates when comparing radiotherapy and corticosteroid injections as adjuvant keloid treatment combined with surgical excision. The lower cost and minimal risk of corticosteroid injections compared with radiotherapy gives the surgeon a simple tool to treat secondary keloid cases and is a useful option when there are limited radiotherapy facilities or if patients decline radiotherapy [Figure 2]. Longer follow-up is necessary for further assessment of the recurrence rate, and the role of preoperative corticosteroid injections in secondary keloids warrants further evaluation.
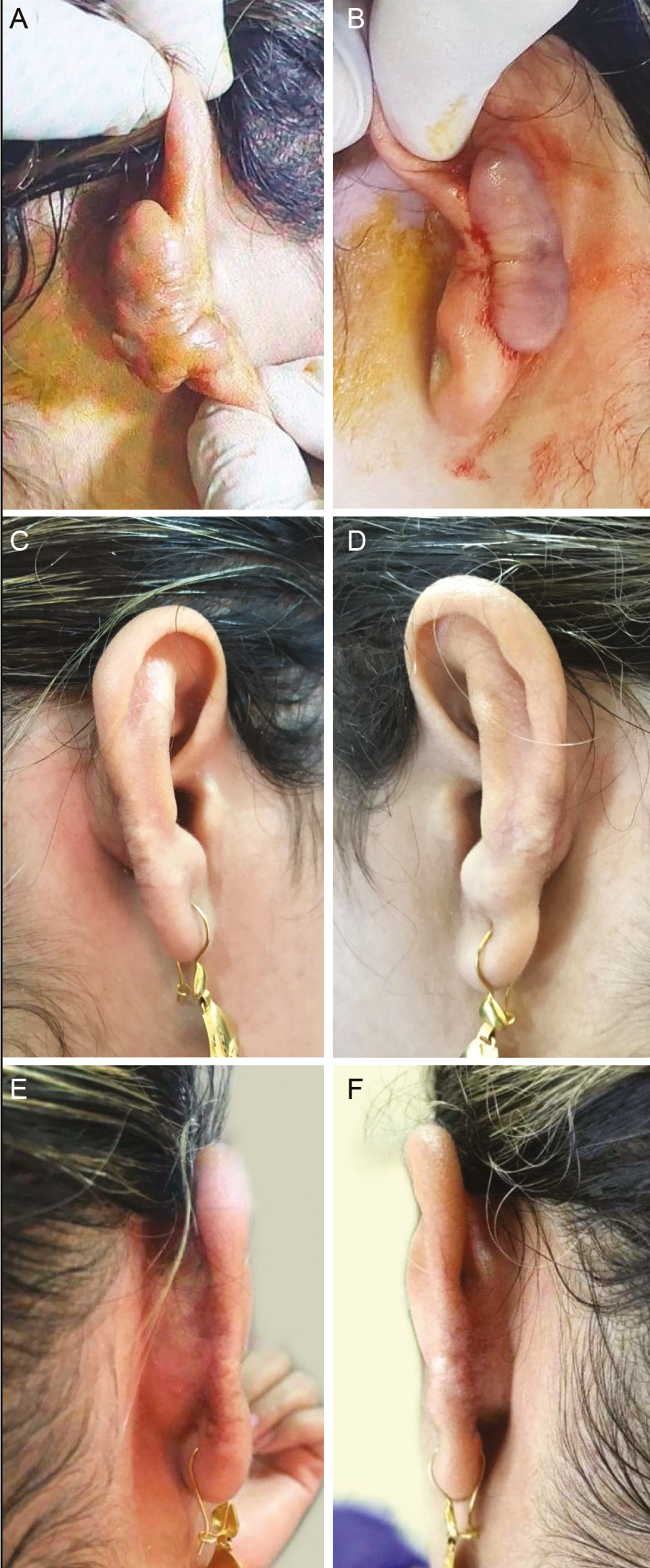
- Patient with recurrent bilateral auricular helix keloids. A and B. Preoperative picture. C–F. Postoperative pictures after 18 months with no evidence of recurrence
CONCLUSION
Perioperative corticosteroid injection is a useful option when treating secondary keloid cases. The recurrence rate is comparable to that of radiotherapy, and the role of preoperative corticosteroid injection in secondary keloids warrants further evaluation.
Recommendation
Researchers recommend a study with a larger sample size, longer follow-up period, and controlled evaluation.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
All authors affirm that there is no actual or potential conflict of interest, including any financial, personal, or other relationships with other people or organizations within three years of beginning the submitted work that could inappropriately influence or be perceived to influence their work.
REFERENCES
- Comparison between cartilage and soft tissue ear piercing complications. Am J Otolaryngol. 1998;19:305-10.
- [Google Scholar]
- Treatment of the keloid: What is new? Otolaryngol Clin North Am. 2002;35:207-20, viii.
- [Google Scholar]
- Unilateral cleft lip repair: Assessment of outcome of Olokun-Olaitan vermillion flap approach. J Craniofac Surg. 2018;29:e804-7.
- [Google Scholar]
- On the nature of hypertrophic scars and keloids: A review. Plast Reconstr Surg. 1999;104:1435-58.
- [Google Scholar]
- A primary protocol for the management of ear keloids: Results of excision combined with intraoperative and postoperative steroid injections. Plast Reconstr Surg. 2007;120:1395-400.
- [Google Scholar]
- Ear keloids: A review and update of treatment options. Clujul Med. 2013;86:313-7. Epub November 6, 2013. PMID: 26527968; PMCID: PMC4462461
- [Google Scholar]
- Scar treatments: Preclinical and clinical studies. J Am Coll Surg. 2008;206:719-30.
- [Google Scholar]
- Inhibition of human keloid fibroblast growth by isotretinoin and triamcinolone acetonide in vitro. Ann Plast Surg. 1994;33:401-5.
- [Google Scholar]
- Therapy of auricular keloids: Review of different treatment modalities and proposal for a therapeutic algorithm. Eur Arch Otorhinolaryngol. 2007;264:1497-508.
- [Google Scholar]
- Combination of different techniques for the treatment of earlobe keloids. Aesthetic Plast Surg. 2002;26:184-8. https://doi.org/10.1007/s00266-002-1490-3
- [Google Scholar]
- Treatment of earlobe keloids by extralesional excision combined with preoperative and postoperative “sandwich” radiotherapy. Plast Reconstr Surg. 2010;125:135-41.
- [Google Scholar]
- Prevention of earlobe keloid recurrence with postoperative corticosteroid injections versus radiation therapy: A randomized, prospective study and review of the literature. Dermatol Surg. 1996;22:569-74.
- [Google Scholar]
- Assessment of the treatment of earlobe keloids with triamcinolone injections, surgical resection, and local pressure. Rev Col Bras Cir. 2015;42:9-13.
- [Google Scholar]
- Surgery and perioperative intralesional corticosteroid injection for treating earlobe keloids: A Korean experience. Ann Dermatol. 2009;21:221-5.
- [Google Scholar]
- Treatment of keloids by combined surgical excision and immediate postoperative X-ray therapy. Ann Plast Surg. 1981;7:281-5.
- [Google Scholar]
- A comparison of the effectiveness of triamcinolone and radiation therapy for ear keloids after surgical excision: A systematic review and meta-analysis. Plast Reconstr Surg. 2016;137:1718-25.
- [Google Scholar]






