Translate this page into:
Use of Cultivated Epidermal Allograft in Chronic Wounds: A Novel Therapeutic Alternative
Address for correspondence: Dr. Daniel De-Luna-Gallardo, Hospital Central Sur de Alta Especialidad de Petroleos Mexicanos, Plastic and Reconstructive Surgery, Anillo Perif. 4091, Fuentes del Pedregal, Tlalpan, PC 14140, Mexico City, Mexico. E-mail: Daniel.delunag@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Introduction:
Chronic wounds represent a frequent cause of consultation for plastic and reconstructive surgeons. The use of epidermal culture stands out because they provide complete epithelialization, adequate aesthetic-functional results, and no morbidity for the patient. Epifast® is a pre-manufactured cultured epidermal allograft derived from the amplification in vitro of human keratinocytes.
Materials and Methods:
A prospective longitudinal multicenter study was carried out in four chronic wound reference centers, which were in charge of plastic and reconstructive surgery services. For a standardized wound bed preparation, the protocol synthesized by the acronym “TIME” was used. At the end of the “TIME” protocol, the pre-fabricated allograft was applied and removed 7 days after its application.
Results:
A total of 133 patients with diagnosis of chronic wound were included in the study. The median age was 69.3 ± 13.6 years. The most common comorbidity found was diabetes mellitus type 2 in 71.4% of the patients (n = 95) and systemic arterial hypertension in 60.2% of the patients (n = 80). The most frequent location of chronic wounds was seen in the lower extremity with 45.1% (n = 60). The mean duration for it to close was 46 ± 14 days, in which they closed within the first 3 months in 93% (n = 125) of the cases. About 91.7% (n = 122) of the wounds achieved total closure.
Conclusion:
Cultured epidermal allograft, combined with a meticulous technique and an adequate selection of patients, represents a safe and effective tool for chronic wounds.
Keywords
Allografts
chronic wound
cultured epidermal grafts
epidermal substitutes
Epifast
Mexico
plastic surgery
reconstructive surgery
INTRODUCTION
Chronic wounds represent a frequent cause of consultation for plastic and reconstructive surgeons, with a prevalence of approximately 1–2.4% worldwide.[123] It is estimated that in the USA, there are about 4.5 billion people with chronic wounds, generating an annual expense that ranges from $28.1 to $96.8 billion dollars, which corresponds 4% of the national health budget, generating a significant economic and psychosocial impact.[456]
In response to the increasing prevalence of chronic wounds, the development of new research has clarified the cellular, humoral, and molecular processes involved in the physiological healing of wounds.[7891011] A better understanding of this process, described as an “Orchestral” phenomenon, has allowed the development of new technologies for the treatment of chronic wounds. These include negative pressure wound therapy,[1213] hyperbaric oxygen therapy,[1415] advanced dressings,[16] and dermal and epidermal substitutes.
Recently, several biological and synthetic dermal and epidermal substitutes (temporary and permanent modalities) have been released. Each of them has different manufacture, processing, mechanism of action, and most importantly, different indications [Table 1]. All of them stand out in the time they aid to complete epithelialization, lower morbidity, and improve medical follow-ups. Within these substitutes, we can find cultured-epidermal grafts (CEGs), which are manufactured from in-vitro cell cultures, which can be amplified from the same patient (autograft) or pre-manufactured from other humans (allograft) or animals (xenografts).[17]
| Substitute | Description | Type | Composition | Duration | Indication |
|---|---|---|---|---|---|
| Oasis (Smith&Nephew, Inc. Smith&Nephew Wound Management, UK) | Porcine extracellular matrix | Biological— xenograft | Porcine small intestinal submucosa | Temporal | Burns, traumatic wounds, chronic wounds |
| Amniotic membrane | Human amniotic membrane | Biological—allograft | Sterilized amniotic membrane | Temporal | Chronic wounds, burns |
| Apligraf (Organogenesis Inc. Living Technology, New Jersey, USA) | Bilayer human in a porcine collagen matrix | Biological— xenograft | Differentiated keratinocytes and fibroblasts in a porcine collagen matrix type I | Permanent | VLU, DFU |
| Epifast (Bioskinco S.A. de C.V. Estado de México, México) | Culture of human epidermal cells | Biological—allograft | Cryopreserve human keratinocytes cultured in vitro on a vaseline gas layer | Permanent | Burns, chronic wounds, VLU, DFU |
| Biobrane (Smith & Nephew, Inc., Smith & Nephew Wound Management, UK) | Advance wound dressing with collagen porcine peptides | Biosynthetic—xenograft | Nylon and silicone with porcine collagen peptides | Temporal | Excised burn wound with or without meshed autografts |
| Integra (Integra LifeSciences Holdings Co., Plainsboro, NJ, USA) | Dermal regenerate template | Biosynthetic—xenograft | Bovine collagen, chondroitin-6-phosphate and a silicone membrane | Permanent | Burns, VLU, DFU, traumatic wounds, general reconstruction |
| Alloderm Select Regenerative Tissue Matrix (Allergan Aesthetic, USA) | Acellular human dermis | Biosynthetic—allograft | Cryopreserved bilayer membrane (basement membrane and dermal surface) | Permanent | Breast reconstruction |
| Alloskin AC (AlloSource, Centennial, CO, USA) | Acellular human dermis | Biological— allograft | Sterilized and washed mesh (1:1) skin graft | Permanent | Burns, traumatic, chronic wounds, VLU, DFU |
| Dermacell AWM (LifeNet Health, Virginia Beach, VA, USA) | Acellular human dermis | Biological— allograft | Terminally sterilized acellular dermis | Permanent | VLU, DFU, PU, AU |
| Endoform (Aroa Biosurgery, Auckland, Nueva Zelanda) | Ovine extracellular matrix | Biological— xenograft | Ovine forestomach bioscaffold | Permanent | Chronic wounds, VLU, DFU, PU, AU |
| PriMatrix (TEI Biosciences, MA, USA) | Bovine dermal matrix | Biological— xenograft | Fetal bovine scaffold, rich in type III collagen | Permanent | Burns, traumatic wounds, chronic wounds |
VLU = venous leg ulcers, DFU = diabetic foot ulcers, PU = pressure ulcers, AU = arterial ulcers
In Mexico, and with great honor for those inventors on whose shoulders we stand, Epifast® (Bioskinco S.A. de C.V., Estado de México, México) was developed. A pre-fabricated cryopreserved biological allograft derived from the culture of in-vitro human keratinocytes (newborn foreskin) was placed on a sterilized and vaselined cloth. Due to its great morphogenic capacity through the production of growth factors such as fibroblast growth factor, epidermal growth factor, platelet-derived growth factor, vascular endothelial growth factor, and transforming growth factor-β and α, it represents an alternative in the treatment of chronic wounds.[181920]
MATERIALS AND METHODS
A prospective longitudinal multicenter study was carried out in four chronic wound referral centers with plastic and reconstructive surgery services. Chronic wound was defined as any wound whose evolution does not progress through a physiological healing process in >30 days or whose definitive closure has not been achieved in 3 months. The research group designed and supervised the trial analysis in collaboration with the sponsor (Bioskinco). Patients gave their consent to participate in the study, and it was approved by the Ethics Committee of the participating centers.
The sponsor, Bioskinco, provided the pre-fabricated biological allograft (Epifast®) 56 cm2 (7.0 cm × 8.0 cm), supervised the trial, and analyzed the data with the supervision of the investigating committee, and established confidentiality agreements between the authors and the sponsor.
A total of 158 patients were referred with diagnosis of chronic wound, from which only 133 patients fully met the inclusion criteria.
Statistical analysis
A descriptive statistical analysis was performed with measures of central tendency and dispersion observed in the studied population.
Wound bed preparation
In all patients, the first consultation in the Wound Clinic service in charge of plastic and reconstructive surgery was taken as day 0. On day 0, the wound was evaluated by a wound specialist nurse and the plastic surgeon in charge. A complete medical history record was taken, emphasizing comorbidities (chronic diseases) and their management. Those patients with uncontrolled chronic diseases were excluded from the study.
Chronic wounds were classified according to the Infectious Diseases Society of America (IDSA) guidelines.[21] Similarly, its etiology, duration, and microbiological culture were assessed by tissue biopsy. The chronic wound area was determined using a digital planimetric program (cm2) according to the recommendations of Jørgensen et al.[22]
For a standardized wound bed preparation, the protocol synthesized by the acronym “TIME” (Tissue management, Inflammation/Infection control, Moisture balance, and Edge of wound), proposed by Leaper et al.[23] and modified by Schultz et al.,[24] was used. Debridement was done according to Smith et al.[25] [Figure 1]. Empirical and targeted drug therapies were based on WSES/SIS-E consensus.[26] The use of negative pressure wound therapy was reserved for chronic wounds with exposed tissue (bone and ligaments). The use of hyperbaric oxygen therapy was reserved for wounds with a history of radiotherapy and peripheral arterial insufficiency.

- Diabetic ulcer in left plantar area with 4 months of evolution. (A) Chronic wound in the first clinical assessment. (B) At the end of the “TIME” protocol. (C) Pre-fabricated biological allograft applied. (D) Chronic wound at the end of the first application. (E) Chronic wound at the end of the second application
The pre-fabricated biological allograft was applied [Figure 1(B) and (C)], at the end of the “TIME” protocol. The product was managed in accordance with the recommendations by the sponsor:
Storage temperature of −20 ± 5°C and up to −60°C for a period not exceeding 12 months;
Slow thawing 10 min before its use;
Application must be aseptically in a controlled environment;
The entire allograft plate must be applied;
The plate removal must be 7–10 days after its application;
Once the plate is removed, it must be discarded.
In all cases, the allograft was removed 7 days after its application, aseptically and in a controlled environment. The size of the wound was reassessed using the digital planimetric program. Individually, a second and third application of a new allograft sheet was evaluated with the same recommendations and methodology mentioned earlier, serially reassessing every 7–10 days after its application [Figure 1(D)].
The total closure was defined as any chronic wound that completed ≥90% epithelialization of the initial total wound area [Figure 1(E)]. In case of an epithelialization between ≥50% and <90%, it would be considered a partial closure; if it is <50%, a non-healing chronic wound would be classified. The etiology, total area (cm2), and total number of allograft plates used until wound closure were collected for all the studied chronic wounds.
Finally, all those wounds that completed total closure were assessed for recurrence rate in long-term follow-up (≥18 months).
RESULTS
A total of 133 patients with a diagnosis of chronic wound who met the inclusion criteria were included in the study. The mean age was 69.3 ± 13.6 years, being the female sex the most affected gender in 77 patients (57.8%) vs. 56 male patients (42%) [Table 2].
| n = 133 | |
|---|---|
| Age (years, SD) | 69.3 (13.8) |
| Gender | |
| Female (%) | 77 (58%) |
| Male (%) | 56 (42%) |
| BMI (kg/m2) (SD) | 30.89 (4.12) |
| Comorbidities | |
| SAH | 80 (60.20%) |
| DM | 95 (71.4%) |
| COPD | 6 (4.5%) |
| AMI | 6 (4.5%) |
| Stroke | 5 (3.7%) |
| Obesity (BMI >30 kg/m2) | 94 (70.6%) |
| CHD | 7 (5.2%) |
SD= standard deviation, BMI = body mass index, COPD = chronic obstructive pulmonary disease, SAH = systemic arterial hypertension, DM = diabetes mellitus, AMI = acute myocardial infraction, CHD = congestive heart disease
The most frequent comorbidity found was diabetes mellitus type 2 (DM2) in 71.4% (n = 95), followed by systemic arterial hypertension (SAH) in 60.2% (n = 80) and chronic obstructive pulmonary disease (COPD) in 4.5% (n = 6). Obesity (BMI > 30 kg/m2) was present in 70.6% (n = 94 patients) [Table 2].
The most frequent etiology related to chronic wounds found in our population was diabetic ulcers (DU) in 26% (n = 34), followed by venous ulcers, dehiscent wounds and pressure ulcers in 17% (n = 175), 16% (n = 21%) and 14% (n = 19), respectively. The mean area was 21.2 ± 8.1 cm2, with a mean duration from its origin of 6 ± 3 months [Table 3].
| n = 133 | |
|---|---|
| Duration (months/sd) | 6.02 (3.1) |
| Area in cm2 (DE) | 21.2 (8.12) |
| Etiology | |
| Dehiscence | 21 (16%) |
| Diabetic ulcer | 34 (26%) |
| Venose ulcer | 22 (17%) |
| Arterial ulcer | 8 (6%) |
| PU | 19 (14%) |
| Radiation ulcer | 16 (12%) |
| Trauma | 12 (9%) |
| Compromised flap | 1 (1%) |
SD = standard deviation, PU = pressure ulcer
The most frequent location of chronic wounds was the lower extremity in 58.6% (n = 78). Other anatomical areas affected were the sacrum and upper extremity in 15.7% (n = 21) and 9.7% (n = 13), respectively. The least affected anatomical regions were the head, thorax, breast, and abdomen [Figure 2]. The 72.9% (n = 97) of all the chronic wounds, had undergone previous treatment for closure (primary closure, topical treatments and dressings).
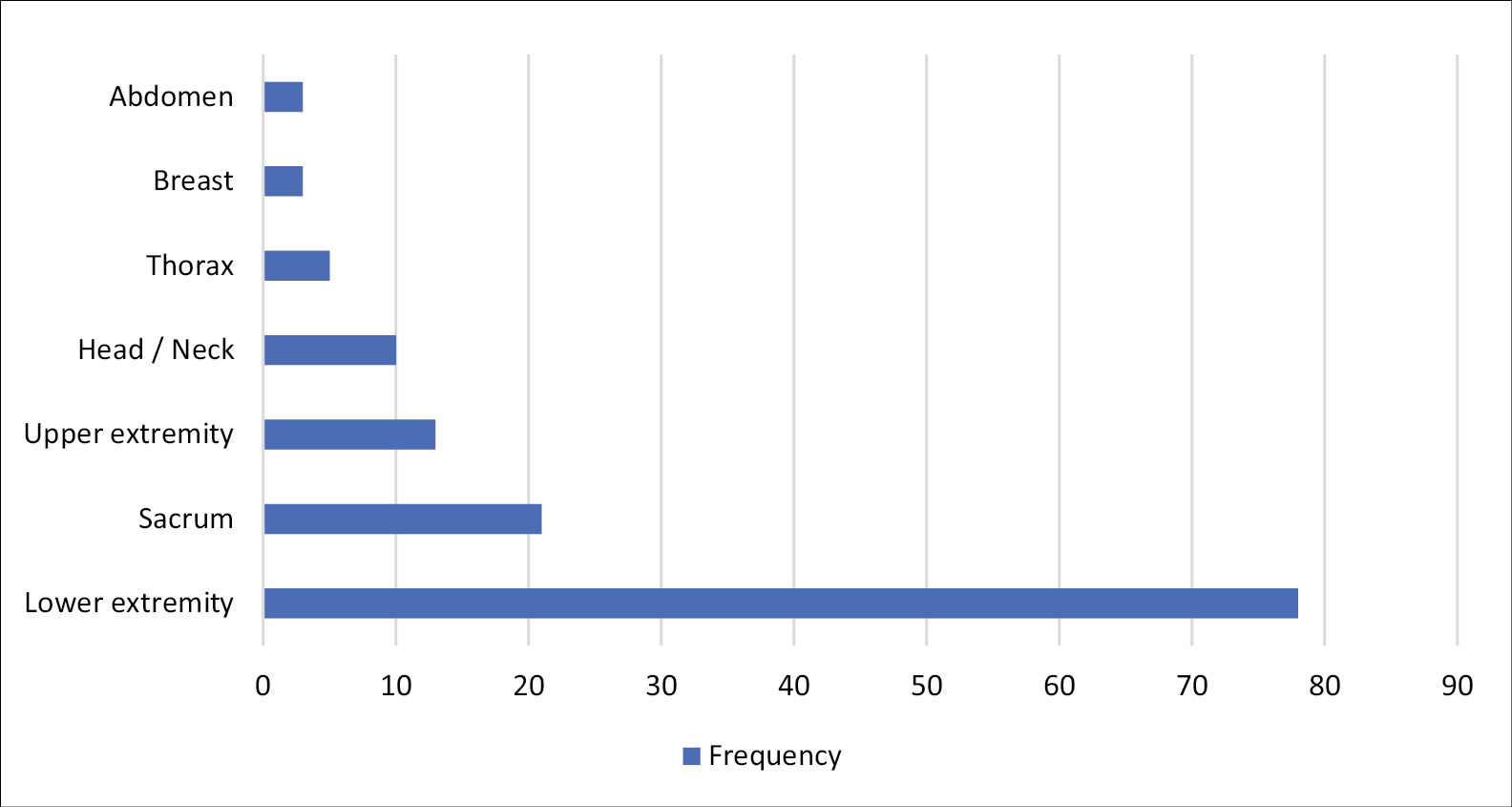
- Wound locations
For wound bed preparation, all patients (n = 133) started the “TIME” protocol, requiring an initial surgical debridement (T). 20.3% (n = 27) of the wounds required two or more serial surgical debridement depending on contamination, depth and non-viable tissue present in the wound. In wounds related with radiotherapy or arterial insufficiency, treatment was supplemented by the use of negative pressure wound therapy in 17.2% (n = 23), hyperbaric oxygen therapy in 18% (n = 24), and compression therapy in 17% (n = 22) of the cases.
The mean duration for closure was 46 ± 14 days, in which 93% (n = 125) of the cases closed within the first three months of starting the treatment. 63% (n = 82) required two replacements of the prefabricated allograft seven days after each one was applied. In total, 91.7% (n = 122) of the wounds achieved total closure, while 7.5% (n = 10) achieved partial closure and 0.75% (n = 1) non-healing [Table 4].
| Number of Epifast replacement | |
|---|---|
| 1 dressing (%) | 29 (22%) |
| 2 dressings (%) | 82 (63%) |
| 3 dressings (%) | 20 (15%) |
| Days for closure (SD) | 46 (± 14) |
| Closure within 3 months | 125 (93%) |
| Closure after 3 months | 6 (4.5%) |
| Wound healed | |
| Partial closure | 10 (7.5%) |
| Total closure | 122 (91.7%) |
| Non-healing | 1 (0.7%) |
In two patients (1.5%) minor adverse reaction occurred at the application site (contact urticaria and itching), that improved with the administration of oral antihistamine. None of them had to discontinue the study or presented a major adverse reaction.
In the long-term follow-up (18 months), of the wounds that achieved total closure (n = 122), 96.7% (n = 118) presented an adequate stability and long-lasting skin cover, without presenting ulceration, infection or recurrence of the chronic wound.
DISCUSSION
Epithelialization is one of the last steps for a successful healing. Within the pathophysiology of chronic wounds, this process is presented as one of the most important challenges to deal with. Therefore, the latest research is aimed at developing products that help promote and accelerate this crucial step in the shortest possible time, in order to avoid potential complications and improve the patient’s quality of life.
One of the greatest advances in recent decades has been the use of temporary and permanent substitutes for the human-dermis, such as human CEG. Its first description dates from 1981.[27] Since its introduction and constant improvement with advanced technology, the use of CEGs has been gaining ground in multiple specialties.[28]
The vast majority of studies based on the use of CEG focussed on the treatment of severely burned patients, as an alternative for dermal substitutes, given the small amount of donor dermal tissues. It was not until 2014, when Gabriel et al.[29] innovated the use of CEG in chronic wounds. The authors described its use in several types of wounds in patients with multiple comorbidities such as DM, SAH, venous and arterial insufficiency, cancer, among others, reporting a complete epithelialization in 75% of the cases. In our study, it is important to emphasize that 100% of the chronic wounds were presented in patients with some comorbidity, where the most frequently found was DM2, closely followed by SAH. It is important to highlight the prevalence of patients with chronic wounds and obesity, which plays an important role in the dysregulation of the immune system and cellular and humoral signaling.
In more recent studies, Fearmonti[30] and Bhatia[31] used CEG in chronic wounds with different etiologies. As in our study, among the most frequent etiologies were: DUs, pressure ulcers, venous ulcers, and surgical dehiscence. The mean percentage of epithelialization was 88% and 82%, respectively (taking 50–99% of the total wound area as partial closure), which corresponds to encouraging results such as those observed in our study.
As reported in the literature, we observed that the most frequently involved anatomical site is the lower extremity, followed by the sacral region with a very important difference. Everts et al.[32] reported, as in most case series, that the anatomical site mostly affected by chronic wounds is the lower extremity. However, this may vary in specialized centers, in which there may be a greater number of chronic wounds in breast, abdomen, or even thorax.
Regardless of the susceptibility of the anatomical site involved, the control of pre-existing comorbidities and the wound bed preparation constitute a crucial step in the success of wound closure prior to the placement of a CEG. Leaper et al.[23] showed that the “TIME” sequence is still relevant 10 years after its publication for wound preparation, helping us to standardize our approaches and therapeutic protocols and significantly improving our success rates, in which negative pressure wound therapy, hyperbaric oxygen therapy, compression therapy, and platelet-rich plasma (PRP) therapy are new complementary options that we must take into account. In our experience, the use of hyperbaric oxygen therapy and negative pressure wound therapy prior to the application of prefabricated allograft in wounds with a history of radiotherapy or arterial insufficiency increased the rate of successful closure by up to 35–65%.
Currently, in-vitro amplification of CEG can be obtained from healthy skin of the same patient (autograft), being able to cultivate enough epithelium to cover 150% of the body surface from a minimal biopsy (<1 cm2). Although the majority of recent studies have decided the cultivation of autologous grafts, these can also be pre-manufactured from other humans (allografts) or animals (xenografts), hence the innovation of our study.[3334]
As shown in our methodology, the main advantage of using a pre-fabricated allograft is availability and accessibility at all times, compared with the time required for a clonal expansion in autologous grafts, which is usually between 2 and 5 weeks depending on the wound size, reflected in prolonged therapeutic periods.[33] Therefore, the use of prefabricated allografts, allowing to shorten waiting times, and being a product available at any time and place are according to the individual requirements.
Another important limitation in the use of autologous grafts is the lack of reproducibility, efficiency in harvesting, and culture techniques, which limits their potential for use in wound clinic services. This study shows that pre-fabricated allografts eliminate the harvesting-culture-amplification processes, standardizing our therapeutic protocols and allowing treatment as an outpatient. Another great advantage of in-vitro cultured allografts is the loss of Langerhans cells during cultivation and cooling, which significantly reduces host rejection by major allogeneic class II histocompatibility antigens, as well as pain decreases in the receiving area. These explains the low rate (1.5%) of adverse reactions in our study, being classified as minor reactions.[343536]
In our study, the mean rate of complete epithelialization was 6.5 weeks, reducing the time average expected for total closure by up to 45–61%, which may have a direct impact on the total cost of medical care for chronic wounds. Bhatia[31] and Everts et al.[32] report a mean rate of complete epithelialization within 7–10 weeks, respectively. Serena et al.[37] reported total closures in 85.7% of the patients within the first 4 weeks after applying the graft in a developing country. These findings support its high efficacy and an alternative with a good cost–benefit ratio.
The rate of partial wound closure in our study was observed in 7.5% (n = 10), where the etiology can play a fundamental role, especially in wounds with history of radiation (moderate-to-severe radiodermatitis), where 81.8% of the therapeutic failures were found. This is different from what was reported by Bhatia,[31] Everts et al.,[32] and Prakash et al.,[38] in which partial closure rates were 11.1%, 11.8%, and 12.8%, respectively.
Finally, one of the great mysteries of CEG was clarified by Gallico et al.[39] and Green,[40] showing that durability as skin covering and its high capacity adapting to mechanical stress developed by the epidermal skin grafts were similar to the autologous partial thickness grafts. This was evidenced in grafts used in children with varying degrees of burn for at least 20 years after grafting. In our study, in long-term follow-up (18 months), 96.7% (n = 118) presented an adequate stability and long-lasting skin cover without recurrence.
Although the results are very encouraging, as it is a non-randomized study, our conclusions will require future studies to demonstrate and support our findings.
CONCLUSION
Chronic wounds continue to be a great challenge for plastic and reconstructive surgeons, as well as for health personnel specialized in this area, such as multidisciplinary groups in wound clinics.
The complete and appropriate closure of chronic wounds is the main objective of wound care, trying to avoid increased morbidity during its treatment. Pre-fabricated allografts, combined with a meticulous technique and an adequate selection of patients, represent a safe and effective alternative in the treatment of chronic wounds.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledge
Subsequent studies to this publication will have the objective to measure the cost–benefit analysis of its use, as well as the reduction in the number of days of hospital stay and the number of surgical interventions.
REFERENCES
- An economic evaluation of the impact, cost, and Medicare policy implications of chronic nonhealing wounds. Value Health. 2018;21:27-32.
- [Google Scholar]
- The resource impact of wounds on health-care providers in Europe. J Wound Care. 2009;18:154-61.
- [Google Scholar]
- Cost-of-illness studies in chronic ulcers: A systematic review. J Wound Care. 2017;26:S4-14.
- [Google Scholar]
- Epidemiology of chronic wounds in Germany: Analysis of statutory health insurance data. Wound Repair Regen. 2016;24:434-42.
- [Google Scholar]
- Health economic burden that wounds impose on the National Health Service in the UK. BMJ Open. 2015;5:e009283.
- [Google Scholar]
- Management of negative pressure wound therapy in the treatment of diabetic foot ulcers. World J Orthop. 2015;6:387-93.
- [Google Scholar]
- Hyperbaric oxygen therapy: Exploring the clinical evidence. Adv Skin Wound Care. 2017;30:181-90.
- [Google Scholar]
- The use of hyperbaric oxygen therapy to treat chronic wounds: A review. Wound Repair Regen. 2008;16:321-30.
- [Google Scholar]
- A decade of conflict: Flap coverage options and outcomes in traumatic war-related extremity reconstruction. Plast Reconstr Surg. 2015;135:895-902.
- [Google Scholar]
- Advances in addressing full-thickness skin defects: A review of dermal and epidermal substitutes. Regen Med. 2018;13:443-56.
- [Google Scholar]
- Advances in keratinocyte delivery in burn wound care. Adv Drug Deliv Rev. 2018;123:18-32.
- [Google Scholar]
- Producción de equivalentes dermo-epidérmicos autólogos para el tratamiento de grandes quemados y cicatrices queloideas. Cuad Cir. 2002;16:41-7.
- [Google Scholar]
- Controlled clinical study of deep partial-thickness burns treated with frozen cultured human allogeneic epidermal sheets. J Burn Care Rehabil. 2000;21:291-9.
- [Google Scholar]
- Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2014;59:e10-52.
- [Google Scholar]
- Methods to assess area and volume of wounds—A systematic review. Int Wound J. 2016;13:540-53.
- [Google Scholar]
- Extending the TIME concept: What have we learned in the past 10 years?(*) Int Wound J. 2012;9(Suppl. 2):1-9.
- [Google Scholar]
- Wound bed preparation: A systematic approach to wound management. Wound Repair Regen. 2003;11(Suppl. 1):S1-28.
- [Google Scholar]
- 2018 WSES/SIS-E consensus conference: Recommendations for the management of skin and soft-tissue infections. World J Emerg Surg. 2018;13:58.
- [Google Scholar]
- Grafting of burns with cultured epithelium prepared from autologous epidermal cells. Lancet. 1981;1:75-8.
- [Google Scholar]
- Porcine xenograft and epidermal fully synthetic skin substitutes in the treatment of partial-thickness burns: A literature review. Medicina (Kaunas). 2021;57:432.
- [Google Scholar]
- Initial experience with a new epidermal harvesting system: Overview of epidermal grafting and case series. Surg Technol Int. 2014;25:55-61.
- [Google Scholar]
- Efficacy of epidermal skin grafts over complex, chronic wounds in patients with multiple comorbidities. Wounds. 2016;28:226-32.
- [Google Scholar]
- Epidermal skin grafting in patients with complex wounds: A case series. J Wound Care. 2016;25:148, 150-3.
- [Google Scholar]
- Use of epidermal skin grafts in chronic wounds: A case series. Int Wound J. 2017;14:1213-8.
- [Google Scholar]
- A prospective, multicentre study on the use of epidermal grafts to optimise outpatient wound management. Int Wound J. 2017;14:241-9.
- [Google Scholar]
- Composite autologous-allogeneic skin replacement: Development and clinical application. Plast Reconstr Surg. 1987;80:626-37.
- [Google Scholar]
- Regenerative medicine of epithelia: Lessons from the past and future goals. Front Bioeng Biotechnol. 2021;9: 652214.
- [Google Scholar]
- Progressive replacement of human cultured epithelial allografts by recipient cells as evidenced by HLA class I antigens expression. Dermatologica. 1987;175: 166-70.
- [Google Scholar]
- Use of a novel epidermal harvesting system in resource-poor countries. Adv Skin Wound Care. 2015;28:107-12.
- [Google Scholar]
- Epidermal grafting for chronic complex wounds in India: A case series. Cureus. 2016;8:e516.
- [Google Scholar]
- Permanent coverage of large burn wounds with autologous cultured human epithelium. N Engl J Med. 1984;311:448-51.
- [Google Scholar]






