Translate this page into:
Atypical Hansen’s Disease Mimicking Xanthogranuloma: Role of Cytology
Address for correspondence: Dr. Tummidi Santosh, Department of Pathology, AIIMS, Mangalagiri, Andhra Pradesh, India. E-mail: born_vss@yahoo.co.in
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Fine needle aspiration cytology is a simple, safe, and effective technique that can be used in the diagnosis of cutaneous diseases. Here, we present a case of Hansen’s disease with an erythematous dermal nodule mimicking xanthogranuloma clinically. In our scenario, since leprosy is considered eliminated in India, the presentation of patients with classical signs and symptoms is becoming rare. Atypical manifestation of leprosy is increasing day by day, so it is necessary to have a high suspicion of leprosy in every case.
Keywords
Fine needle aspiration
Fite stain
leprosy
negative image
palm and sole
xanthogranuloma
BACKGROUND
Fine needle aspiration cytology is a simple, safe, and effective technique. In the diagnosis of cutaneous diseases, cytology was first used by Arnault Tzanck in 1947.[12] Since then cytology has been used for the diagnosis of various vesiculobullous lesions, herpetic lesions, leprosy, cutaneous leishmaniasis, tumoral lesion, and granulomatous diseases.[13] Leprosy is a chronic infectious and granulomatous disease. The causative agent of leprosy is Mycobacterium leprae, an acid-alcohol–resistant bacillus, which has an affinity for skin and peripheral nerve cells.[3] Clinical manifestations of leprosy have a wide spectrum of presentation. In all of its stages, it mimics a great variety of other lesions. The differential diagnosis of leprosy is so wide that we need to exclude a wide variety of dermatological diseases before making a diagnosis of leprosy because of the social stigma.[4] Here, we present a case of Hansen’s disease with an erythematous dermal nodule mimicking xanthogranuloma clinically.
CASE PRESENTATION
A 15-year-old female presented to our Dermatology outpatient department with multiple nodules over bilateral arms, face, left thigh, and bilateral soles for 1 year [Figure 1A–F] with no family history or contact history. Her viral marker for HIV, HBsAg, and HCV was negative. On examination, the lesions were multiple, well-defined, erythematous, nontender, firm-to-hard nodules with the presence of yellowish black crust over few of the chin nodules. There were few flat-topped ill-defined grouped papules coalescing to form small plaques over bilateral soles. Her viral markers were negative. Clinical differentials were given as juvenile xanthogranuloma, rhinosporidiosis, and deep fungal infection.

- (A–F) Erythematous nodules over chin, nose, bilateral arms, and thigh along with plaque-like lesion over the sole
Since the differential of leprosy was not considered in this case, the clinician had sent the patient for FNAC of the nodules. Cytosmears showed many scattered foamy macrophages, lymphocytes, and neutrophils [Figure 2A–C]. Negative images were seen within the macrophages and in the extracellular background. ZN stain was positive for the negative images that were seen on the Giemsa stain [Figure 2D]. A diagnosis of atypical mycobacterial infection was suggested. We were able to exclude the differential diagnosis of xanthogranuloma which shows foamy macrophages, Touton giant cells but AFB stain negative. From the nodular lesions, the patient was then advised for skin punch biopsy and GeneXpert testing for tuberculosis. Histopathology revealed epidermis with orthokeratosis, hypergranulosis, flattened rete ridges, and spongiosis. The underlying dermis showed dense perivascular, perifollicular, and perineural lymphomononuclear cell infiltrate along with foamy histiocytes and necrosis [Figure 3A–C]. Fite-Faraco staining for lepra bacilli showed a bacillary index of 6+ [Figure 3D]. Histopathological features were consistent with the Histoid variant of Hansen’s disease. GeneXpert testing for Mycobacterium tuberculosis was negative.
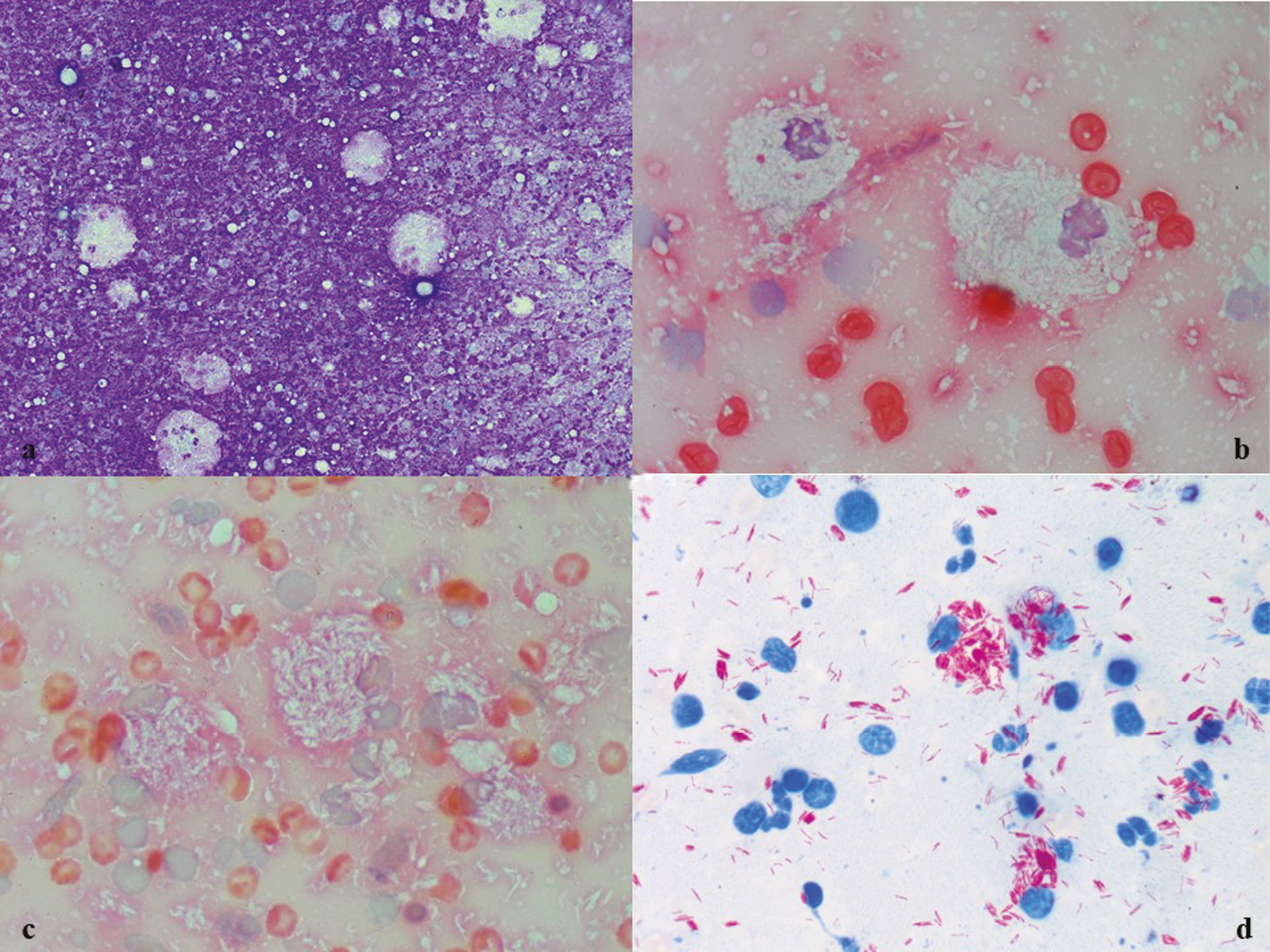
- (A–C) Scattered foamy macrophages and neutrophils with extracellular and intracellular negative images of bacilli (Giemsa and PAP ×10, ×40); (D) Bright red positive bacilli (ZN, ×100)
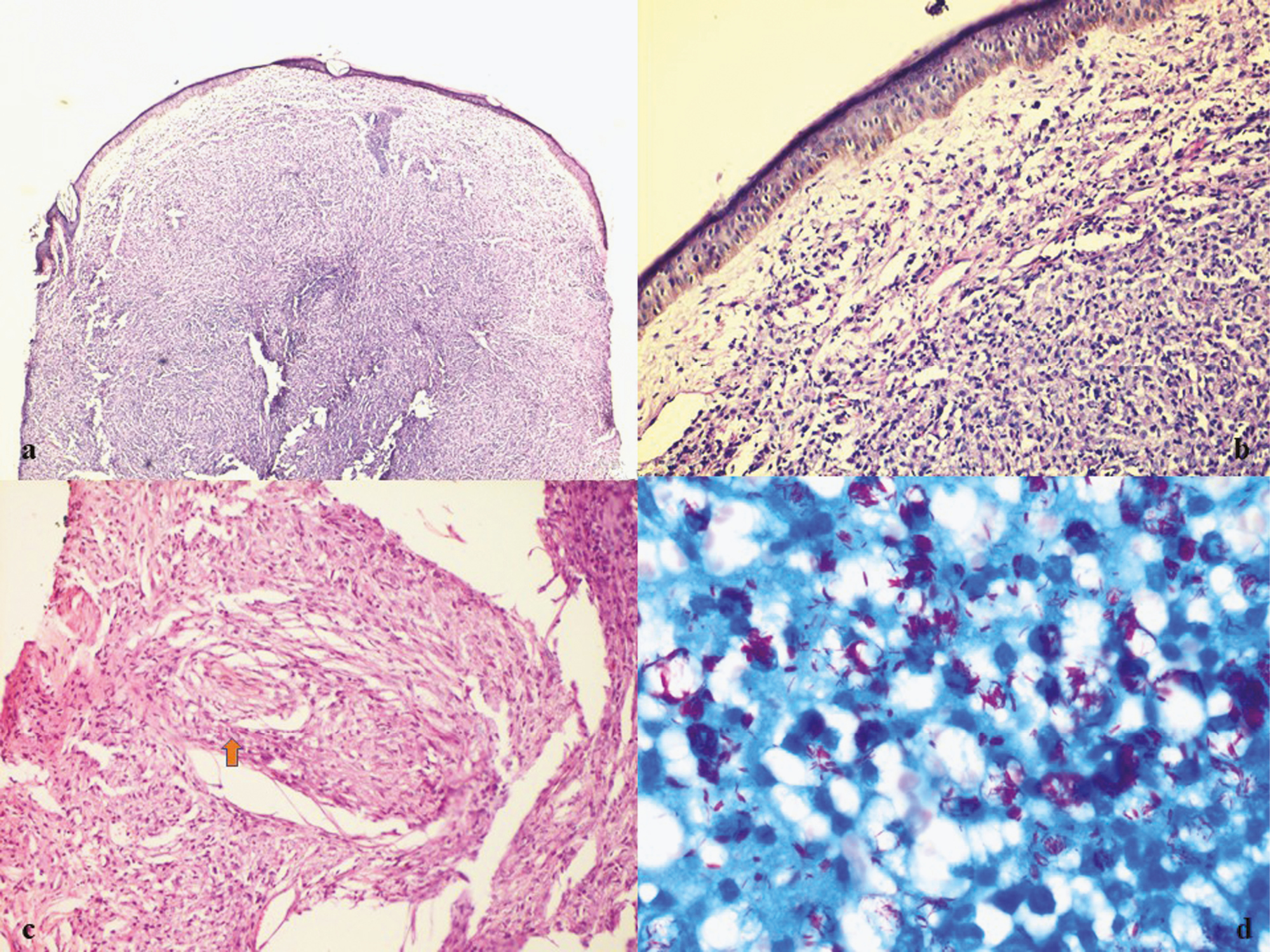
- (A–C) Nodular dome-shaped lesion on biopsy with grenz zone. Histopathology showing dense perivascular and perifollicular lymphomononuclear cells infiltrate along with foamy histiocytes (H and E ×10, ×20, ×40); (D) Positive Fite-Faraco stain for lepra bacilli (Fite, ×100)
The patient had come with her father on a second visit along with FNAC and biopsy reports. On re-evaluation, she had thick bilateral ulnar and common peroneal nerves. Positive family history in the father was noted. The patient was then started on multibacillary (MB) multidrug therapy (MDT) (rifampicin, clofazimine, and dapsone) for a duration of 12 months. She was on follow-up after 1 month with subsidence of lesions.
DISCUSSION
Globally, Hansen’s disease affects more than 180,000 people. Its prevalence has rapidly decreased because of the widespread implementation of MDT. During the 1980s and early 1990s, the global burden of Hansen’s disease was estimated to be 11–15 million people.[5] Clinical presentation of leprosy is variable. It can present as from tuberculoid to indeterminate to lepromatous disease. These clinical manifestations of leprosy depend on bacterial load and loss of M. leprae–specific cellular immunity. Because of the wide spectrum and variable clinical manifestations sometimes it is very difficult to make an accurate diagnosis clinically. Therefore, it is necessary to investigate appropriately in every suspected case.[6] Leprosy can also be presented as atypical manifestations like angioedema, lesions mimicking lupus vulgaris, mimicking cutaneous T-cell lymphoma, lepromatous leprosy with a single plaque with gynecomastia,[4] nonhealing ulcer over right finger mimicking tenia versicolor,[7] granuloma annulare, erythema multiforme,[8] and relapsing polychondritis[9] reported in the literature.
FNAC is an essential, basic diagnostic technique used to investigate superficial/deep swellings.[10] It can be used in suspected cases of Hansen’s disease as in our case the patient was presented with multiple, well-defined, erythematous, firm-to-hard nodules. Because of those erythematous nodules, differential diagnosis was given as xanthogranuloma, rhinosporidiosis, and deep fungal infections; hence, cytology was performed. Cytosmears showed the presence of foamy macrophages, extracellular and intracellular negative images. Fungal elements and Touton giant cells were not seen in Tzanck smears.[9]
Negative images (lipid in the cell wall) are well known in the cytology literature and occur not only in leprosy but also in Mycobacterium avium intracellulare (MAI) infections in immunocompromised patients and crystal-forming conditions.[10] However, the classic features of perivascular, perifollicular, and perineural foamy histiocytes and pattern of spread along with Fite stain for lepra bacilli along with the clinical signs of MAI infections were excluded.[11] Xanthogranulomatous lesions will also show foamy macrophages, but other than foamy macrophages Touton giant cells will be present and will be AFB negative.[12] Deep fungal infections will show the presence of fungal elements. Interpretation in cytology is most difficult in leprosy because M. leprae shows variable morphology like a pink rod, a fragment, or a granule.[13]
In lepromatous leprosy, the bacilli can be easily detected, while in tuberculoid leprosy the bacteria are very few and it is difficult to find. In patients with reactional leprosy, smears reveal numerous foamy macrophages along with the presence of “negative” images of M. leprae as in our case of leprosy. Raut et al.[6] also reported in their study that leprosy patients present with nodular lesions.
CONCLUSION
In our scenario, since leprosy is considered eliminated in India, the presentation of patients with classical signs and symptoms is becoming rare. Atypical manifestation of leprosy is increasing day by day, so it is necessary to have a high suspicion of leprosy in every case. FNAC/Tzanck smear/Slit skin smears and/or punch biopsy should be performed from the selective site in every suspected case of leprosy for early diagnosis and treatment.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Diagnostic reliability of the Tzanck smear in dermatologic diseases. Int J Dermatol. 2014;53:178-86.
- [Google Scholar]
- The man behind the eponym. Arnault Tzanck, his work and times. Am J Dermatopathol. 1985;7: 121-3.
- [Google Scholar]
- The value of Tzanck smear test in diagnosis of erosive, vesicular, bullous, and pustular skin lesions. J Am Acad Dermatol. 2008;59:958-64.
- [Google Scholar]
- A rare form of Hansen’s disease presenting as filiform verrucous papules on the feet. JAAD Case Rep. 2016;2:105-7.
- [Google Scholar]
- Unusual presentation of multibacillary nodular leprosy. J Lab Physicians. 2017;9:57-9.
- [Google Scholar]
- A case of Hansen disease presenting as tinea versicolor. Dermatol Online J. 2013;19:7.
- [Google Scholar]
- Atypical presentation of leprosy: A report of two cases. Indian J Dermatol. 2007;52:198.
- [Google Scholar]
- Leprosy with atypical skin lesions masquerading as relapsing polychondritis. Case Rep Infect Dis. 2016;2016:7802423.
- [Google Scholar]
- This ‘rose’ has no thorns-diagnostic utility of ‘rapid on-site evaluation’ (ROSE) in fine needle aspiration cytology. Indian J Surg Oncol. 2019;10:688-98.
- [Google Scholar]
- Lepromatous leprosy-negative images giving the diagnostic clue. Indian J Pathol Microbiol. 2017;60:616-7.
- [Google Scholar]
- More experiences with the Tzanck smear test: Cytologic findings in cutaneous granulomatous disorders. J Am Acad Dermatol. 2009;61:441-50.
- [Google Scholar]






