Translate this page into:
Effectiveness of intralesional bleomycin in the management of difficult-to-treat and resistant cutaneous warts in a tertiary care teaching hospital in Puducherry: A quasi-experimental study
*Corresponding author: Sheela Kuruvila, Department of Dermatology, Venereology and Leprosy, Aarupadai Veedu Medical College and Hospital, Puducherry, India. kuruvilasheela@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Singh Y, Rajamohanan RR, Vasudevan S, Kuruvila S. Effectiveness of intralesional bleomycin in the management of difficult-to-treat and resistant cutaneous warts in a tertiary care teaching hospital in Puducherry: A quasi-experimental study. J Cutan Aesthet Surg. 2025;18:108-13. doi: 10.25259/jcas_71_24
Abstract
Objectives:
The objective of this study was to determine the effectiveness of intralesional injection of bleomycin in the management of difficult-to-treat and resistant cutaneous warts.
Material and Methods:
A total of 54 patients were enrolled in the study, of whom 52 completed it. We administered 0.1% bleomycin over the warts and conducted follow-up at 4, 8, and 12 weeks. If the warts were not completely clear, we administered the next dose of intralesional bleomycin at each visit until the third visit. If the lesions resolved at the third visit, we conducted a telephonic interview for the next follow-up at the end of 12 weeks to record any recurrence of warts and residual side effects.
Results:
Out of 54 patients enrolled in the study, two were lost to follow-up. About 49 (94.2%) patients had clearance of warts at the end of the study period. About 45 (86.5%) patients had complete resolution of lesions after the first session. Three patients achieved complete clearance after the second treatment session. One patient achieved complete clearance at the end of the 12th week. One patient showed a partial response at the end of the 12-week treatment. There was no response for two patients at the end of 12 weeks. Two patients were lost to follow-up.
Conclusion:
The present study demonstrates that intralesional bleomycin is an efficient and safe treatment option in the management of resistant and difficult-to-treat warts.
Keywords
Effective
Intralesional bleomycin
Resistant warts
Safe
INTRODUCTION
Cutaneous warts are one of the most common viral infections affecting the skin.1 They are caused by multiple strains of the human papillomavirus (HPV) and occur frequently on both skin and mucosal surfaces.2 While spontaneous recovery is possible, it often takes years and remains unpredictable.3 Many individuals opt for treatment due to cosmetic concerns, pain, social stigma, and the risk of malignancy.4 Difficult-to-treat and resistant warts constitute a substantial proportion of cases presenting to dermatologists for treatment. However, despite trying various treatment modalities with varying results, dermatologists still lack a universally accepted treatment choice for these groups of warts.5 Since the 1970s, intralesional bleomycin has been used to treat warts, although it is not a common procedure.6 In 1962, Umezawa et al. isolated bleomycin from the actinomycotic soil fungus Streptomyces verticillus.7 Bleomycin sulfate is a polypeptide mixture of glycoproteins that contains cytotoxic sulfur. It can be separated into two main fractions, bleomycin A and B, through chromatography. These fractions can, further, be divided into subfractions, with the main components available commercially being A2 and B2.8 Intralesional bleomycin is a relatively new treatment modality being explored for the management of resistant warts.9 However, cure rates and reported adverse effects vary widely among the different studies available in the literature. In this study, we aim to determine the effectiveness of intralesional bleomycin in the treatment of difficult-to-treat and resistant warts.
MATERIAL AND METHODS
The quasi-experimental study was carried out between August 2022 and August 2023 at the Department of Dermatology, Venereology, and Leprosy in Pondicherry Institute of Medical Sciences, Kalapet, Puducherry, India. We enrolled a total of 54 patients in our current study. Of these, 52 patients completed the study and were available for analysis.
Study design
After obtaining Institutional Ethical Clearance, all patients above 12 years of age, clinically diagnosed to have resistant or difficult-to-treat warts, were included in this study. Pregnant and lactating women, patients with a history of Raynaud’s phenomenon, and patients who have taken any other immunotherapy for the treatment of warts in the past month were excluded from the study. We conducted a detailed history and examination, obtained written consent, and took pictures of the warts at each visit. We informed the study participants to refrain from using any other treatment modalities during the study period.
Data management
Data were entered and compiled using Microsoft Excel 2010 (Office 360, Microsoft Ltd., USA), and data were analyzed using the Statistical Package for the Social Sciences 23.0 version (IBM Ltd., USA).
Statistical analysis
We expressed categorical variables as frequencies and proportions. Continuous variables were expressed as mean and standard deviation.
Case definitions
Resistant warts are defined as warts that have failed to respond to treatment twice in the past.
Difficult site warts were classified as periungual, palmar, and plantar warts.
Procedure
A single vial of bleomycin containing 15 mg of powdered bleomycin was dissolved in 5 mL of distilled water to give a final solution of bleomycin. We filled an insulin syringe with two parts of 2% lignocaine and one part of bleomycin solution, achieving a final concentration of 1 mg/mL. We cleaned each wart and the surrounding skin with isopropyl alcohol. A superficial paring of the wart was done to remove the surrounding callus without reaching the bleeding points. We injected 0.1% bleomycin intralesionally until the wart blanched. We administered a maximum of 2 mL of bleomycin in a single visit to prevent any systemic effects. We gave the patient oral analgesics for 3 days after the procedure.
We conducted follow-ups at 4, 8, and 12 weeks. At each visit, the number of lesions remaining, and the local and systemic side effects were recorded. If the warts were not completely clear, we administered the next dose of intralesional bleomycin at each visit until the third visit. At the third visit, if all lesions had resolved, we conducted a telephonic interview for the next follow-up at the end of 12 weeks to record any recurrence of warts and residual side effects. During each visit, all patients were screened for the following adverse effects: pain, erythema, edema, pigment changes, Raynaud phenomenon, scarring, and nail damage.
RESULTS
In this present study, we recruited and totally incorporated 54 patients.
The baseline characteristics of study patients were 38 (70.4%) males and 16 (29.6%) females. The ratio of male and female was M: F = 2.3:1, the average age of the patients was found to be 28.11 ± 9.32 (range: 12–61) years, and the warts were localized over palms and soles (in 40 patients) and periungual skin (in 14 patients), as shown in Table 1.
| Baseline characteristics | Classifications | Number of patients (%) |
|---|---|---|
| Gender | Male | 38 (70.4) |
| Female | 16 (29.6) | |
| Age in years | 11–20 | 14.8 |
| 21–40 | 75.9 | |
| 41–60 | 3.7 | |
| >60 | 1.8 | |
| Location of warts | Palms and soles | 74.1 |
| Periungual | 25.9 |
Prior treatment modalities included electrocautery in 41 patients, cryotherapy in 10 patients, chemical cautery in two patients, and fractional carbon dioxide in one patient. About 85.2% of patients had 2–3 treatment modalities prior, and 14 patients had 3–4 treatment modalities prior, as shown in Table 2.
| Variables | Classifications | Number of patients (%) |
|---|---|---|
| Number of past procedures | 2–3 | 85.2 |
| 3–4 | 14.8 | |
| Past procedure | Electrocautery | 75.9 |
| Cryotherapy | 18.5 | |
| Chemical cautery | 3.7 | |
| CO2laser | 1.9 |
CO2: Carbon dioxide
Out of 54 patients enrolled in the study, two lost follow-ups. About 49 (94.2%) patients had clearance of warts at the end of the study period. About 45 (86.5%) patients had complete resolution of lesions after the first session [Figure 1], and no further treatment was given to them. Among the remaining nine patients, 3 (92.3%) achieved complete clearance following the second treatment session [Figure 2], and they received no further treatment. One patient (94.2%) had complete clearance at the end of the 12th week [Figure 3]. One patient had a partial response at the end of a 12-week treatment. There was no response for 2 patients at the end of 12 weeks (which may be due to the larger size of the warts). Two patients lost follow-up. Table 3 displays the responses to treatment at various visits.
| Follow-up | Response to treatment | Number of patients (%) |
|---|---|---|
| First follow-up | Complete clearance | 86.5 |
| Partial clearance | 13.5 | |
| Second follow-up | Complete clearance | 92.3 |
| Partial clearance | 7.7 | |
| The third follow-up | Complete clearance | 94.5 |
| Partial clearance | 5.5 | |
| At the end of treatment | Complete clearance | 94.2 |
| Partial clearance | 5.5 |
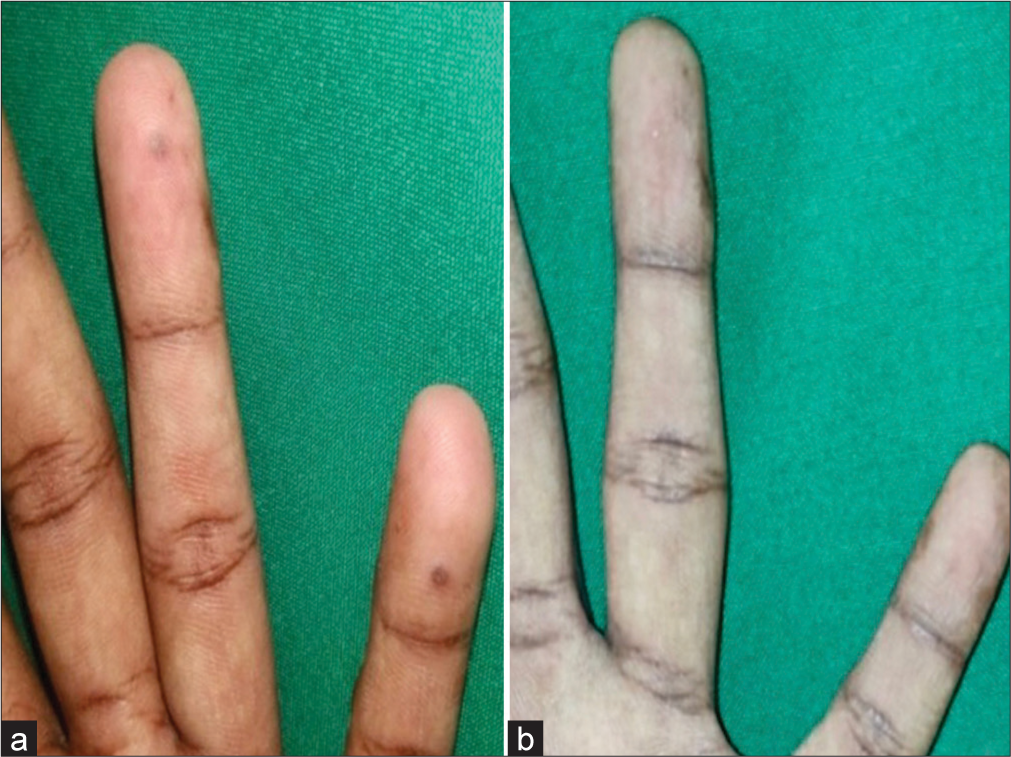
- (a) A single hyperpigmented papule is seen over the distal end of the left little finger. (b) Lesions resolved after 4 weeks of treatment with bleomycin.

- (a) Single-skin-colored plaque with a verrucous surface present on the sole of the right foot. (b) Complete clearance after 8 weeks of bleomycin treatment.

- (a) Single plaque with a verrucous surface present over the middle finger of the right hand. (b) Complete clearance after 12 weeks of bleomycin treatment.
DISCUSSION
Warts are benign infectious lesions of the skin and mucosa caused by HPV.10 They are common among school-going children and young adults. A major proportion of the warts are responsive to conventional therapeutic measures. However, they can sometimes be tough to treat as they may become chronic, resistant, and relapsing, posing a problem in the dermatology outpatient department.
Resistant warts are defined as warts that have failed treatment twice in the past. Difficult-to-treat warts refer to warts occurring on sites such as periungual, palmar, and plantar warts.4
A variety of therapeutic modalities have been used for these, with varying degrees of success. Since the 1970s, people have used intralesional bleomycin for the treatment of warts, although not regularly.6 Intralesional bleomycin has gained commendation recently for the management of warts, especially in the palmar and plantar regions, as other treatment modalities have been unsuccessful.11 It has been used in various studies to treat resistant warts, with differing degrees of success.11
A study by Amer et al. looked at how well intralesional bleomycin worked on resistant plantar warts and found that it worked 47.6% of the time for resistant plantar warts and 77% of the time for warts on the extremities.12 Agius et al. conducted a study where they injected bleomycin (1 U/mL) intralesionally using a dermojet at 5-week intervals for 25 weeks, resulting in complete or partial clearance in 89.9% of recalcitrant plantar warts.13 Overall, a complete cure rate of 86.5% (after the first follow-up) and 92.3% (after the second follow-up) without any recurrences were noted in our study. Only 7.7% of patients had a partial cure at the end of the 12-week study period, demonstrating the substantial effectiveness of this treatment modality. Similarly, Soni et al. successfully treated 85 palmoplantar and periungual warts with intralesional bleomycin (1 mg/mL). After receiving one or two intralesional injections of bleomycin during 12 weeks, they observed a total resolution of 82 (96.5%) warts.11 Unni and Tapare conducted an evaluator-blinded and placebo-controlled study on intralesional bleomycin in the treatment of common warts, in which 93.10% of patients showed complete resolution.1
Barkat et al., in their study on the evaluation of 1 mg/mL intralesional bleomycin every 2 weeks for four sessions in the treatment of plantar warts, found a cure rate of 69.3% with minimal and tolerable side effects.14 In a study conducted by Alghamdi and Khurram, 74% of patients with plantar warts showed complete clearance with very diluted bleomycin delivered through the intralesional mini-puncture technique.15 Bremner, in 1976, managed 24 patients with 142 warts with intralesional injections of bleomycin and achieved a cure rate of 63%, which is substantially less than our study.16 Aziz-Jalali et al. achieved complete resolution of warts in 95 (73%) and partial resolution in 31 (24%) warts after intralesional injection of bleomycin.17
In a study by Soni et al., the cure rate for periungual warts was 94%, which is almost like our study.11 In a study by Alghamdi and Khurram, with only one injection, 86.6% of patients showed total clearance of the treated periungual wart on a 6-month follow-up, which is less than our study.15 Golchai and Vaghe Karegar treated resistant palmoplantar and periungual warts with a bleomycin injection and reported a cure rate of 88.4%.18 Sollitto et al. observed a cure rate of 65.4%, which is significantly lower than our study.19 Al-Naggar et al. did a study on topical bleomycin spraying for plantar warts and reported a cure rate of 70%.20 Kruter et al. treated warts over the hands and feet, including plantar warts, and reported a 74% cure rate.21 Table 4 shows the cure rate of various previous studies for the treatment of warts with intralesional bleomycin.
| Other studies | Dosage and schedule for intralesional bleomycin | Cure rates (%) | Remarks |
|---|---|---|---|
| Salk and Douglas8 | 1.5 mg/mL 2 weeks apart and followed up to 6 months | 87 | Plantar warts |
| Soni et al.11 | Two injections 2 weeks apart in 1 mg/mL strength and followed up for 1 year | 96.5 | Included are palmoplantar and periungual warts |
| Barkat et al.14 | 1 mg/mL 2 weeks apart for a maximum of four injections | 69.3 | Plantar warts |
| Unni and Tapare1 | 1 mg/mL 2 injections, 2 weeks apart, and followed up to 6 months | 93.1 | Common warts |
| Mehta et al.3 | 1 mg/mL 2 injections, 2 weeks apart, and followed up for 6 months | 84 | Common warts, including periungual warts |
| Golchai and Vaghe Karegar18 | 1 mg/mL injections 2 weeks apart for up to three injections | 88.4 | Resistant periungual and palmoplantar warts |
| Aziz-Jalali et al.17 | 1 mg/mL 4 weeks apart for 3 doses, and were followed up for 6 months | 73 | Periungual warts |
| Sollitto et al.19 | 1 mg/mL at 0, 1 week, 1 month, and followed up to 6 months | 65.4 | Mosaic plantar warts |
| Al-Naggar et al.20 | 1 mg/mL 2 weeks apart for a maximum of 4 injections | 70 | Topical bleomycin spraying for plantar warts |
| Marahatta et al.4 | IL bleomycin only (retrospective case series) | 88 | Resistant palmoplantar and periungual warts |
| Kruter et al.21 | 3 mg/mL bleomycin 3 weeks apart and followed up for 6 months | 74 | Warts on hands and feet, including plantar warts |
| Our study | 1 mg/mL every 4 weeks for a maximum of two sessions | 94 | Included are resistant palmoplantar and periungual warts |
IL: Intralesional
We included patients with resistant warts (warts that have failed treatment twice in the past) with different treatment modalities. Hayes and O’Keefe did a similar retrospective study on resistant warts. Hayes and O’Keefe reported a cure rate of 73.3% with 0.25 mg/mL of bleomycin, 87.5% with 0.5 mg/mL, and a 90% cure rate with 1 mg/mL of bleomycin.22 The dose at which bleomycin is given could act as a supplementary factor that can impact the therapeutic outcome.
The size of the wart, rather than its location, duration, number, dose, or method of bleomycin infiltration, is an important factor in predicting response. As seen in our study, warts with a larger size showed a minimal response, this might be because huge warts are harder to infiltrate with bleomycin adequately, necessitating repeated treatment sessions.
In all individuals, common side effects included erythema at the injection site, induration, and pain that did not need treatment cessation.23 The combination of intralesional bleomycin with 2% lignocaine reduced injection site pain immediately. Consumption of oral co-amoxiclav and diclofenac over the post-injection period at the appropriate doses was adequate to provide relief from the symptoms.24 None of our patients displayed any side effects following the injection of bleomycin in the periungual region. Baseline hematological and biochemical parameters were normal. Intralesional injection of bleomycin appears to be an effective and safer modality of treatment for cutaneous warts without producing any adverse systemic side effects.
Limitations
The limitations of our study are acknowledged. The sample size of our study could have been larger. There was no comparison between intralesional bleomycin and other treatment modalities in our study.
CONCLUSION
From this study, we have concluded that difficult-to-treat and resistant warts constitute a substantial proportion of all warts presenting to dermatologists for treatment. However, this group of warts still does not have an accepted treatment of choice, and different treatment modalities are being tried with varying results. Given the proven effectiveness of intralesional bleomycin, its use in routine practice may aid in formulating treatment protocols.
Authors’ Contributions
All the authors contributed to the research study. Yogindher Singh: Concepts, design, definition of intellectual content, literature search, manuscript preparation, manuscript editing, and manuscript review. Remya Raj Rajamohanan: Definition of intellectual content, literature search and manuscript review. Senthilvel Vasudevan: Statistical analysis. Sheela Kuruvila: Definition of intellectual content, literature search, manuscript preparation, manuscript editing and manuscript review.
Ethical approval
The research/study approved by the Institutional Review Board at Pondicherry Institute of Medical Sciences, IEC: RC/2022/42, and dated 26th July 2022.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Intralesional bleomycin in the treatment of common warts. Indian J Drugs Dermatol. 2017;3:73.
- [CrossRef] [Google Scholar]
- Comparison of effectiveness and safety of immunotherapy of warts with intralesional versus subcutaneous MMR vaccine: An open label randomized, parallel group, clinical trial. Indian J Dermatol. 2022;67:99-108.
- [CrossRef] [Google Scholar]
- Evaluation of efficacy and safety of intralesional bleomycin in the treatment of common warts: Results of a pilot study. Indian J Dermatol Venereol Leprol. 2019;85:397-404.
- [CrossRef] [Google Scholar]
- Intralesional bleomycin for the treatment of resistant palmoplantar and periungual warts. Dermatol Res Pract. 2021;2021:8655004.
- [CrossRef] [Google Scholar]
- Dermatography with bleomycin as a new treatment for verrucae vulgaris. Int J Dermatol. 1997;36:145-50.
- [CrossRef] [Google Scholar]
- Intralesional bleomycin in the treatment of cutaneous warts: A randomized clinical trial comparing it with cryotherapy. Indian J Dermatol Venereol Leprol. 2009;75:262-7.
- [CrossRef] [Google Scholar]
- Intralesional bleomycin sulfate injection for the treatment of verruca plantaris. J Am Podiatr Med Assoc. 2006;96:220-5.
- [CrossRef] [Google Scholar]
- Pulsed dye laser and intralesional bleomycin for treatment of resistant viol hand warts. Lasers Surg Med. 2002;30:135-40.
- [CrossRef] [Google Scholar]
- Efficacy of a bleomycin microneedle patch for the treatment of warts. Drug Deliv Transl Res. 2018;8:273-80.
- [CrossRef] [Google Scholar]
- Efficacy of intralesional bleomycin in palmo-plantar and periungual warts. J Cutan Aesthet Surg. 2011;4:188-91.
- [CrossRef] [Google Scholar]
- Therapeutic evaluation for intralesional injection of bleomycin sulfate in 143 resistant warts. J Am Acad Dermatol. 1988;18:1313-6.
- [CrossRef] [Google Scholar]
- Dermojet delivery of bleomycin for the treatment of recalcitrant plantar warts. J Dermatol Treat. 2006;17:112-6.
- [CrossRef] [Google Scholar]
- Evaluation of intralesional injection of bleomycin in the treatment of plantar warts: clinical and dermoscopic evaluation. Int J Dermatol. 2018;57:1533-7.
- [CrossRef] [Google Scholar]
- Successful treatment of plantar warts with very diluted bleomycin using a translesional multipuncture technique: Pilot prospective study. J Cutan Med Surg. 2012;16:250-6.
- [CrossRef] [Google Scholar]
- Efficacy of intralesional bleomycin in the treatment of resistant warts. J Skin Stem Cell. 2014;1:e18875.
- [CrossRef] [Google Scholar]
- Therapeutic evaluation of intralesional injection of bleomycin sulfate in the treatment of resistant warts. Med J Islamic Republic Iran. 1995;8:233-6.
- [Google Scholar]
- A perspective study using bleomycin sulfate in the treatment of plantar verrucae. J Foot Surg. 1989;28:141-4.
- [Google Scholar]
- Intralesional bleomycin injection vs microneedling-assisted topical bleomycin spraying in treatment of plantar warts. J Cosmetic Dermatol. 2019;18:124-8.
- [CrossRef] [Google Scholar]
- Intralesional bleomycin for warts: Patient satisfaction and treatment outcomes. J Cutan Med Surg. 2015;19:470-6.
- [CrossRef] [Google Scholar]
- Reduced dose of bleomycin in the treatment of recalcitrant warts. J Am Acad Dermatol. 1986;15(5 Pt 1):1002-6.
- [CrossRef] [Google Scholar]
- Guidelines for the management of cutaneous warts. Br J Dermatol. 2001;144:4-11.
- [CrossRef] [Google Scholar]
- Therapeutic evaluation of efficacy of intralesional bleomycin in common warts including palmo-plantar and periungual warts: A prospective study. Int J Res Dermatol. 2019;5:329-37.
- [CrossRef] [Google Scholar]







