Translate this page into:
The deception of acantholysis: The painful and overlooked story of ocular surface squamous neoplasia in a red eye
*Corresponding author: Shibhani Sudheer Hegde, Department of Dermatology, Venereology and Leprosy, Bharati Vidyapeeth Medical College and Hospital, Pune, Maharashtra, India. shibhani.s.hegde@gmail.comm
-
Received: ,
Accepted: ,
How to cite this article: Shah S, De D, Hegde SS, Maknikar V, Chatterjee D, Goliwale F. The deception of acantholysis: The painful and overlooked story of ocular surface squamous neoplasia in a red eye. J Cutan Aesthet Surg. doi: 10.25259/JCAS_5_2024
Abstract
A painful red eye can be extremely distressing and can be caused by various ophthalmological or dermatological disorders. We hereby report a case of a red, painful eye in a 55-year-old woman suspected to have pemphigus or ocular cicatricial pemphigoid. Acantholytic cells were seen on conjunctival biopsy, and treatment with prednisolone 60 mg/day with the preliminary diagnosis of ocular pemphigus showed no improvement. Reevaluation of the tissue block showed full-thickness dysplasia within the conjunctival epithelium and acantholytic cells. A diffuse subtype of ocular surface squamous neoplasia, formerly called Bowen’s disease of the eye, is an extremely rare condition and is often misdiagnosed as conjunctivitis, leading to delayed diagnosis. Our case posed an additional diagnostic dilemma due to the uncertainty caused by acantholysis in histology. She was finally treated with external beam radiotherapy, showing resolution of redness and pain. There was no recurrence over the next 1 year.
Keywords
Acantholysis
Ocular surface squamous neoplasia
Bowen’s disease
Carcinoma in situ
Radiotherapy
INTRODUCTION
Ocular surface squamous neoplasia (OSSN) is an uncommon entity encompassing a broad spectrum of corneal and conjunctival malignancies ranging from mild epithelial dysplasia carcinoma in situ to invasive squamous cell carcinoma.1 Vascularized limbal mass in the inter-palpebral part of one eye is the classical presenting feature.2 Diffuse form of OSSN is not only the least common but also the most difficult to diagnose. It is often misdiagnosed and treated as chronic conjunctivitis,3 as seen in our patient, who was treated for 8 months before a biopsy was performed. Moreover, due to the presence of acantholytic cells, she was treated for pemphigus vulgaris of the ocular mucosa. Electron microscopy of dysplastic cells shows fewer desmosomes.1 This explains the perplexity of acantholysis seen in our case.
CASE REPORT
A 55-year-old woman and a manual laborer by occupation came to the dermatology outpatient department with a year-long history of a distressingly painful and red left eye. Severe pain had a major impact on the quality of her health. Multiple ophthalmologists had evaluated her for glaucoma and other scleral and corneal diseases that could contribute to her presenting features. With no such identifiable cause noted, she was treated multiple times as a case of conjunctivitis with no improvement in the redness or pain despite treatment. After 8 months, an oculoplastic conjunctival biopsy was performed, showing acantholytic cells. With the suspicion of early ocular pemphigus, paraneoplastic pemphigus, or ocular cicatricial pemphigoid, a search for underlying malignancy ensued, and prednisolone at a dose of 60 mg/day was started. Pain and redness of the eye, however, did not respond to treatment.
When she presented to our outpatient department, she had diffuse palpebral and conjunctival injection and edema of the lower eyelid of the left eye with no obvious scarring [Figure 1]. The contralateral eye and other mucocutaneous surfaces were not involved, and regional lymphadenopathy was absent. Direct immunofluorescence from conjunctiva, salt split indirect immunofluorescence on normal human skin, and multi-parametric enzyme-linked immunosorbent assay for autoimmune bullous disorders were performed on oral mucosa. All these investigations were non-contributory for diagnosis. On re-evaluation of the tissue block, full-thickness dysplasia and acantholytic dysplasia were noted [Figure 2a and b].
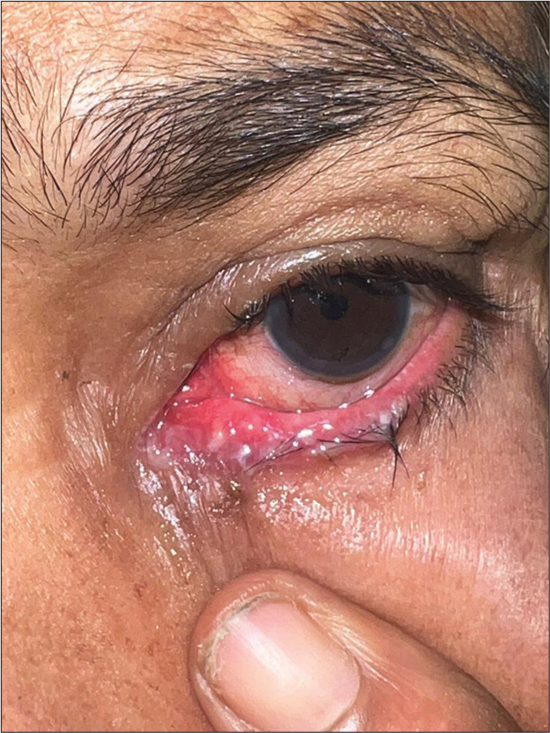
- Diffuse palpebral and conjunctival injection and edema of lower eyelid of the left eye.
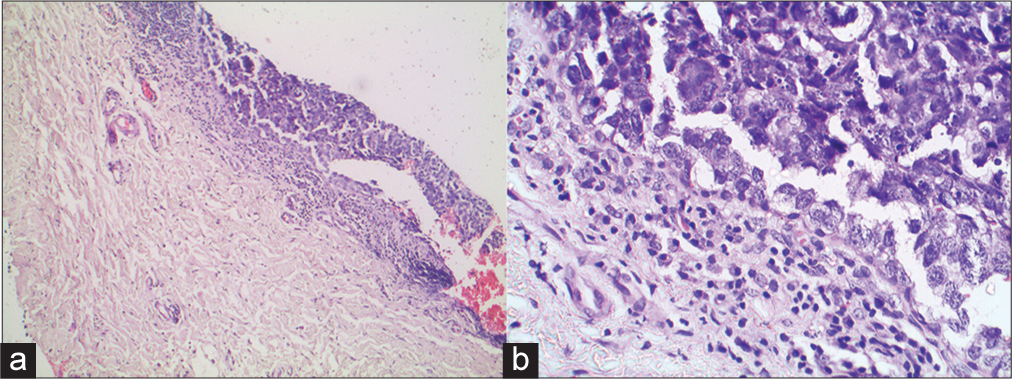
- (a) Histopathology of conjunctival epithelium showing full-thickness dysplasia (Hematoxylin-eosin stain; magnification × 40), (b) Histopathology of conjunctival epithelium showing multiple dysplastic cells (Hematoxylin-eosin stain; magnification × 100).
A final diagnosis of OSSN of diffuse subtype was made. In view of the diffuse nature of the OSSN and biopsy compromised conjunctiva, surgical intervention was not considered. The patient did not consent to a trial of reconstructive surgery; hence, external beam radiotherapy was started.
Electron treatment plans were generated using an eclipse planning system with version 15.06.06 of the dose calculation server using an Electron Monte Carlo calculation Algorithm, with a minimum uncertainty of approximately 1%. Our patient was treated with 6 MeV electron energy of 6 × 6 applicator using a Cerrobend cutter to encompass the diseased conjunctiva and spare the surrounding normal tissue with great effect. Eye shield was used with the Cerrobend shield to immobilize the eye during the whole treatment fraction. A dose of 45 Gy in 25 fractions was given on a daily basis with evaluation of adverse effects before every sitting [Figure 3a-c]. Resolution of redness and pain was significant after 4 weeks of electron beam therapy with no recurrences noted on follow-up over the next 6 months [Figure 4]. Care was taken to protect her vision and she did not develop any adverse effects of radiotherapy.

- (a) Patient receiving external beam radiotherapy. The eye-shield was used with the Cerrobend shield to immobilize the eye during the whole treatment fraction. (b) Cerrobend shield. (c) Close up view of patient with the eye shield.

- Six weeks after external beam radiotherapy, the patient’s left eye shows complete resolution of injection edema of the left eye.
DISCUSSION
OSSN was first proposed as a distinct entity in 1995 after decades of outdated terminologies such as epithelioma, epithelial plaque, precancerous epithelioma of the limbus, and Bowen’s disease.4 It is the 3rd most common oculo-orbital malignancy of the elderly.1 The use of conjunctival intraepithelial neoplasia (CIN) that parallels similar terminology in gynecology still helps in management of preinvasive and invasive OSSN.
Known risk factors for the development of OSSN are elderly age, chronic ultraviolet-B exposure, male gender, cigarette smoking, chronic trauma or inflammation, exposure to certain chemicals, skin types more prone to sunburn, Vitamin-A deficiency, and viruses, especially human papillomavirus, that acts as a co-factor. Mutations in p-53 tumor suppressor gene, telomerase reverse transcriptase gene promoter or hyper-expression of matrix metalloproteinase have been known to contribute toward the oncogenesis of ocular epithelium.1-3,5
For the most part, conjunctival OSSN with a rare extension to the cornea is seen. A vascularized limbal mass is the classical clinical presentation. Morphologically, leukoplakic, gelatinous, placoid/papillary, nodular, and nodulo-ulcerative forms have been described.1,2 These circumscribed lesions are easy to locate and evaluate. The diffuse form of OSSN is the least common and most notorious subtype, as conjunctival redness without any raised mass is the presenting feature. Impersonating chronic conjunctivitis further delays its diagnosis1, causing detrimental delay in patient management.
Symptoms range from red eye, signs of ocular irritation and foreign body sensation to severe pain and visual loss.4 Most OSSN are slow-growing tumors.3 Microscopically, pre-invasive epithelial dysplasia is termed mild, moderate, or severe (CIN I, II, and III, respectively), depending on the thickness of affected epithelium. Severe or full-thickness CIN III is also called carcinoma in situ or Bowen’s disease. Once it penetrates the basement membrane, it is termed invasive OSSN.1
The gold standard for diagnosis of OSSN still remains incisional/excisional biopsy followed by histopathological evaluation.2 CIN I, II, and III are characterized by dysplastic epithelium of the lower third, extending onto the middle third and full thickness, respectively. Invasive OSSN shows nests of well-differentiated or poorly-differentiated squamous cells penetrating the epithelial basement membrane. In addition, these squamous cells can be interspersed with spindle cells and mucoepidermoid cells.1
Electron microscopic features of OSSN include increased mitochondria, endoplasmic reticulum, and tonofilaments but also a reduction in desmosomes1 inevitably explaining the occurrence of acantholysis in dyskeratotic cells, which alternatively, was mistaken for ocular pemphigus in our case.
Exfoliative cytology and impression cytology are the noninvasive methods to assess dysplasia within the cells during treatment.2-4,6
Differential diagnosis of a red, painful eye include a variety of ophthalmological and dermatological conditions. Autoimmune blistering disorders such as pemphigus and pemphigoid can affect unilateral ocular mucosa. Ocular pemphigus can precede or succeed mucocutaneous involvement but is usually non-cicatricial as opposed to ocular cicatricial pemphigoid, which is relentless, cicatricial and can affect vision.7 Keratinized dysplastic cells with varying degrees of cellular atypia and polarity, mitotic figures, and syncytial like grouping of cells can help reinforce the diagnosis of malignancy.8
Surgical excision with a wide margin is the traditional treatment of choice in most OSSN that present with a vascularized limbal mass with the assessment of margins. Adjunctive treatment modalities are cryotherapy, topical anti-metabolites such as fluorouracil and mitomycin-C, immunotherapy, and radiotherapy.1,9 Other modalities such as topical cidofovir, photodynamic therapy, and anti-vascular endothelial growth factor therapy have been tried with inconsistent outcomes.2 Complete excision is neither practical nor possible in diffuse OSSN, and taking into account the patient’s predicament, radiotherapy was the front-runner as the treatment option.
Brachytherapy has been used for OSSN since the 1930s in the form of β-irradiation or γ-radiation sources.4,8 Although not widely used in most OSSN due to the multiple sessions required and intricate modus operandi, it has a peculiar role in diffuse type of OSSN.1 Cup-shaped applicator is placed directly on the ocular surface, and superficial conjunctiva is irradiated after protecting vision.4 Complications of brachytherapy include dry eye, post-irradiation conjunctivitis, cataract, telangiectasia, scarring of sclera, and corneal perforation.8
Generally considered a low grade-malignancy, OSSN recurrences tend to have the same histological grade as that of the primary tumor.4 Surveillance period of 2–7 years can be kept with regular cytology to check for recurrences.
CONCLUSION
Our case was intriguing as her OSSN was first misdiagnosed as conjunctivitis and then as pemphigus on account of acantholysis on histopathology. Acantholysis was, in fact, part of the primary malignant process.
Authors’ contributions
Dr. Swapnil Shah, Dr. Vedprakash Maknikar, Dr. Fahim Goliwale, Dr. Dipankar De and Dr. Debajyoti Chatterjee managed the patient and took full responsibility for the integrity and accuracy of the clinical details. Dr. Shibhani Sudheer Hegde drafted and prepared the manuscript. Dr. Swapnil Shah, Dr. Dipankar De and Dr. Vedprakash Maknikar critically revised the manuscript for its intellectual content. Final manuscript was approved by all the authors.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Ocular surface squamous neoplasia: A review. Cornea. 2003;22:687-704.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical management of ocular surface squamous neoplasia: A review of the current evidence. Ophthalmol Ther. 2018;7:247-62.
- [CrossRef] [PubMed] [Google Scholar]
- Conjunctival/corneal intraepithelial neoplasia. Int Ophthalmol Clin. 2009;49:63-70.
- [CrossRef] [PubMed] [Google Scholar]
- Ocular surface squamous neoplasia. Surv Ophthalmol. 1995;39:429-50.
- [CrossRef] [PubMed] [Google Scholar]
- The aetiology and associations of conjunctival intraepithelial neoplasia. Br J Ophthalmol. 2006;90:109-13.
- [CrossRef] [PubMed] [Google Scholar]
- Epithelial, non-melanocytic and melanocytic proliferations of the ocular surface. Semin Diagn Pathol. 2016;33:122-32.
- [CrossRef] [PubMed] [Google Scholar]
- Ocular surface involvement in pemphigus vulgaris: An interdisciplinary review. Ocul Surf. 2020;18:40-6.
- [CrossRef] [PubMed] [Google Scholar]
- Ocular surface squamous neoplasia. Ophthalmol Clin North Am. 2005;18:1-13.
- [CrossRef] [PubMed] [Google Scholar]
- Antimetabolites in ocular surface neoplasia. Curr Opin Ophthalmol. 1998;9:35-9.
- [CrossRef] [PubMed] [Google Scholar]






