Translate this page into:
A comparative study of the efficacy of autologous platelet-rich fibrin matrix versus platelet-rich plasma in the treatment of non-healing leg ulcers
*Corresponding author: Dr. Navya Donaparthi, Associate Professor, Department of Dermatology, Command hospital Air force, Bengaluru, Karnataka, India. navya.donaparthi@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mech S, Kaur G, Arora S, Bhatnagar A, Dabas R, Donaparthi N, et al. A comparative study of the efficacy of autologous platelet-rich fibrin matrix versus platelet-rich plasma in the treatment of non-healing leg ulcers. J Cutan Aesthet Surg. doi: 10.25259/JCAS_38_2024
Abstract
Objectives:
Platelet-rich plasma (PRP) and Platelet-rich fibrin matrix (PRFM) are different generations of platelet concentrates providing growth factors and cytokines aiding tissue repair. However, there is not enough research comparing the efficacy of PRFM and PRP. This study aims to assess and compare the efficacy of platelet rich fibrin matrix (PRFM) with platelet-rich plasma (PRP) for the treatment of patients with non-healing leg ulcers of various etiologies.
Material and Methods:
A comparative, prospective, interventional, randomised, open labelled study was done recruiting a total of 64 consecutive cases of non-healing leg ulcers reporting to the department. One group received PRFM and the other received PRP dressings at 01 weekly interval for 04 sittings. Size and volume of the ulcers were calculated at baseline and weekly following each sitting.
Results:
In the PRP group the volume of ulcer was reduced by 60.66% after four applications, compared to 55.56% reduction in PRFM group. In the PRP group the area of ulcer was reduced by 51.85% after four applications, compared to 46.83% reduction in the PRFM group. There was a constant reduction in size after each application, in both the groups, but the difference finally had a P value >0.05 which was not statistically significant.
Conclusion:
Both Autologous Platelet Rich Fibrin Matrix and Platelet Rich Plasma are effective modalities for treatment of leg ulcers with excellent safety profile. While PRP demonstrated superior efficacy, PRFM was also comparable, showing its potential as a viable alternative.
Keywords
Non healing leg ulcers
Platelet rich Plasma
Platelet Rich Fibrin Matrix
Platelet products
INTRODUCTION
An ulcer is a disruption in the continuity of the skin, including the epithelium, the full thickness of the epidermis, and the dermis either partially or fully and underlying tissues. Non-healing leg ulcers pose a significant challenge in clinical practice, often leading to prolonged patient suffering, especially in the elderly, decreased quality of life, and substantial healthcare costs.1 Non-healing leg ulcer is chronic, recurring condition, a common cause of discomfort and misery in the elderly.2,3 There is no definite consensus regarding the time limit to consider a leg ulcer as chronic; some have considered 4 weeks, some 6 weeks, and some even 3 months of non-healing as the minimum duration for consideration as chronic.2,4,5 The concept of wound bed preparation evolved as a methodical approach in managing chronic wounds, aiming to comprehend the cellular and biochemical disruptions occurring within a wound. Substantial advancements occurred in the 1990s with the introduction of novel technologies for treating chronic wounds, including the development of bioengineered skin and topical growth factors.6 Despite advancements in wound care management, a subset of patients continued to experience delayed wound healing, necessitating innovative therapeutic approaches. Platelet-rich fibrin matrix (PRFM) and platelet-rich plasma (PRP) have emerged as promising adjunctive therapies in the management of non-healing leg ulcers, offering the potential to accelerate wound healing and improve clinical outcomes. PRFM and PRP are autologous blood-derived products enriched with various growth factors, cytokines, and other bioactive molecules essential for wound healing. PRFM is a fibrin-based biomaterial that concentrates platelets and leukocytes within a fibrin matrix, providing sustained release of growth factors and promoting tissue regeneration. PRP, on the other hand, is a plasma fraction enriched with platelets, which can be activated to release growth factors and cytokines involved in the wound healing cascade. The use of PRFM and PRP in non-healing leg ulcers is based on their ability to modulate key biological processes essential for wound repair, including inflammation, cell proliferation, extracellular matrix formation, and angiogenesis. By harnessing the regenerative potential of platelet-derived growth factors (PDGFs), these therapies aim to overcome the biological barriers that impede wound healing and promote tissue regeneration in chronic wounds. Several clinical studies have evaluated the efficacy of PRFM and PRP in non-healing leg ulcers, demonstrating promising results in terms of accelerated wound closure, reduced wound size, and improved healing outcomes. Randomized controlled trial by Anitua et al. reported a significant improvement in wound healing rates and reduction in wound size following the application of PRGF-Endoret, a type of PRP, in patients with chronic leg ulcers.7 Similarly, a meta-analysis conducted by Xie et al. concluded that PRP therapy was associated with a higher likelihood of complete wound healing and reduced healing time compared to standard care in patients with diabetic foot ulcers.8 Furthermore, a study by Driver et al. investigated the effects of PRFM in the treatment of venous leg ulcers and found that PRFM significantly accelerated wound healing and improved ulcer closure rates compared to standard care.9 Similarly, a prospective study by Pereira et al. demonstrated the efficacy of PRP injections in promoting wound healing and reducing pain in patients with refractory diabetic foot ulcers. Despite the growing body of evidence supporting the efficacy of PRFM and PRP in non-healing leg ulcers, several challenges and controversies exist regarding their optimal use, including standardization of preparation techniques, variability in patient response, and cost-effectiveness considerations.10 Furthermore, the mechanism of action underlying the therapeutic effects of PRFM and PRP in wound healing remains incompletely understood, warranting further research to elucidate their biological effects and optimize treatment protocols. Here, we present a comparative study on the efficacy of autologous PRFM versus PRP in the treatment of non-healing leg ulcers.
MATERIAL AND METHODS
In the present study, 64 patients participated for a duration of 3 years. Systematic random sampling was employed for participant selection and sample size was calculated based on the comparison of means between two groups. Ethical clearance was taken from the Institutional Ethical Committee. Non-healing trophic ulcers on the leg of more than 8-week duration were included in the study. Patients with age group below 18 years, having a history of bleeding disorders, anemia, and other hematological disorders, platelet count <1.5 Lakhs/cumm, patients on anticoagulant medications (aspirin, warfarin, heparin), uncontrolled diabetes mellitus, with malignant ulcers, pregnant and lactating females were excluded from this study. A thorough general physical, systemic, and dermatologic examination was carried out after taking informed consent. Ulcer size in terms of length, breadth, and depth was measured at baseline and before each sitting of dressing. The length and breadth were measured through tracing paper, scale, and depth with the help of a sterilized toothpick at the maximum depth of the wound and then measured through scale. Wound area was calculated using the formula for an ellipse: Length × width × 0.7854. Volume was calculated using the formula: Length × width × 0.7854 × depth. Primary infection if any was managed with antibiotics and surgical debridement wherever necessary before starting the treatment.
For the PRP group, under strict aseptic precautions, 8 mL of blood is collected in a sterilized borosilicate glass tube with vacuum containing acid citrate dextrose and a separator gel (PrecurcellTMPRP). PRP was prepared after centrifugation at 3500 rpm for 15 min. Three layers were obtained following this: Upper straw-colored platelet-poor plasma (PPP), red-colored lower fraction containing red blood cells, and the middle white-colored layer containing the PRP above separator gel [Figure 1]. The upper straw-colored layer (PPP) of 3.5 mL was discarded. PRP suspended in remaining 2 mL of plasma was aspirated and injected at the ulcer margin after proper surgical debridement and was dressed with a non-absorbent dressing.
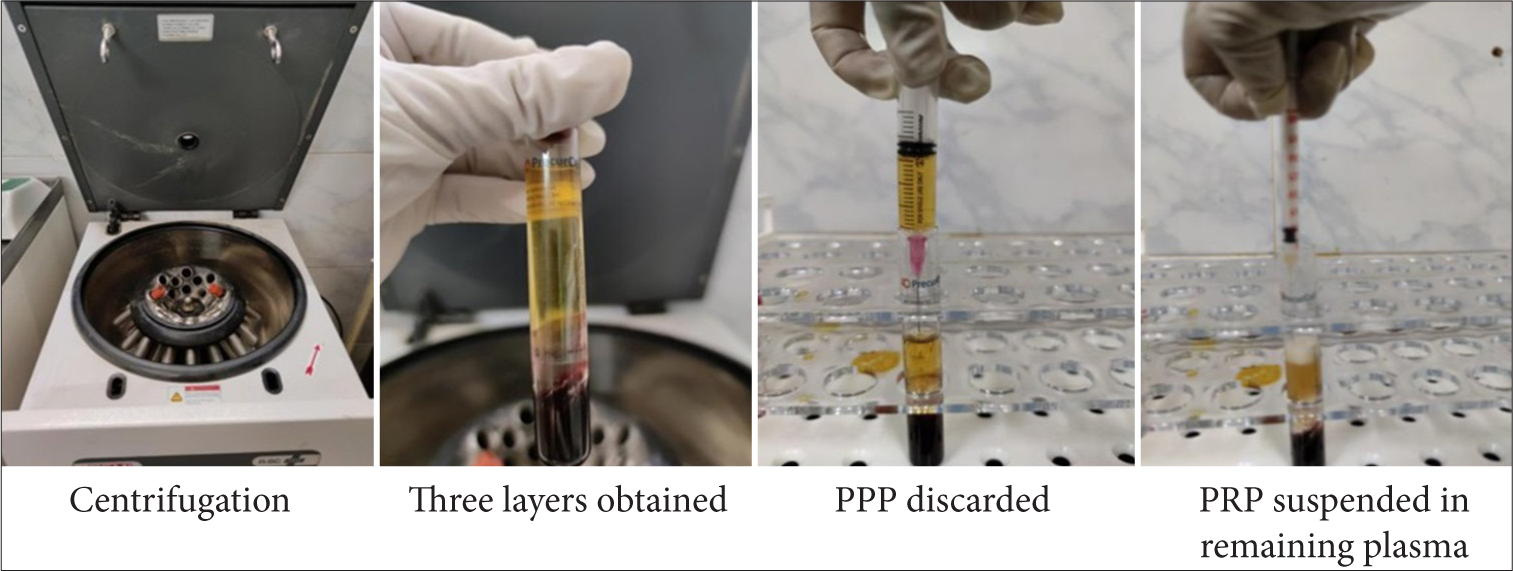
- Preparation of platelet-rich plasma. PPP: Platelet poor plasma, PRP: Platelet rich plasma
For the PRFM group, the procedure was the same as the PRP group till preparation of PRP. Then, 2 mL of the prepared PRP suspended in remaining plasma Centrifugation Three layers obtained PPP discarded PRP was transferred to a tube containing 2 mL of calcium gluconate (fibrin tube) which was left undisturbed for 15 min and visible solidified clot, PRFM was collected [Figure 2]. The fibrin gel was placed over the ulcer base and covered with a sterile non-absorbable dressing to be left in situ for 7 days. Adequate rest was ensured during the treatment course.

- Preparation of platelet-rich fibrin matrix. PRP: Platelet rich plasma, PRFM: Platelet rich fibrin matrix.
The procedure was repeated every week up to a maximum of 4 sittings. At the beginning and every week, the healing of the ulcer was assessed, area and volume were calculated, and photographs were taken. The percentage reduction in ulcer volume was calculated after subtracting the final volume from initial volume then dividing by initial volume and thereafter multiplying by 100.
RESULTS
In this study, a total of 32 patients suffering from leg ulcers underwent treatment with PRFM, while an additional 32 patients with leg ulcers were treated with PRP. Among the 64 subjects enrolled, the age group with the highest proportion (39%) was 60–69 years old. Interestingly, the distribution of age was observed to be similar in both treatment groups, with the highest proportion of patients falling within the 60–69 age bracket, accounting for 41% in the PRFM group and 38% in the PRP group.
Regarding the demographic profile, a majority of the subjects (61% out of 64) were identified as retired army personnel. The onset of ulcers was noted to be spontaneous in 72% of cases, with 81% in the PRFM group and 63% in the PRP group. Other contributing factors to ulcer onset included infections (16%) and trauma (13%), with varying percentages in each treatment group.
Ulcer types varied among the subjects, with chronic venous ulcers being the most prevalent at 66%, followed by diabetic ulcers at 13%. Other ulcer types included arterial ulcers (6%), post-infectious ulcers (2%), and post-traumatic ulcers (11%). Notably, the duration of ulcers ranged from 6 months to 7 years.
In terms of ulcer characteristics, the PRFM group exhibited an equal distribution of single and multiple ulcers (50% each), while the PRP group primarily presented with single ulcers (81%). Bacterial growth was observed in half of the subjects, with various bacterial strains identified, necessitating antibiotic therapy based on culture and sensitivity reports.
The primary objective of the study was to assess the reduction in ulcer volume and size following multiple applications of PRFM and PRP. Results indicated a gradual decrease in both ulcer volume and size with each application in both treatment groups. Although the differences observed after each treatment session or after the final application were not deemed statistically significant (P > 0.05), it is noteworthy that the percentage reduction from baseline was notably higher in the PRP group compared to the PRFM group.
Specifically, in the PRP group, there was a remarkable 60.66% reduction in ulcer volume [Table 1] and a significant 51.85% reduction in ulcer area [Table 2] after four applications, in contrast to a 55.56% reduction in volume and a 46.83% reduction in area observed in the PRFM group. These findings underscore the potential efficacy of PRP in promoting ulcer healing compared to PRFM. The representative clinical pics of both groups are depicted in Figures 3-6.
| Mean volume of ulcers at baseline and every week for 04 weeks | Mean volume in PRFM group in cm≥ | Mean volume in PRP group in cm≥ | p-value | PRFM | PRP | ||
|---|---|---|---|---|---|---|---|
| Change from baseline in cm≥ | Change from baseline in percentage | Change from baseline in cm≥ | Change from baseline in percentage | ||||
| Baseline | 12.6±9.6 | 12.2±12.0 | 0.8884 | - | - | - | - |
| First week | 10.2±7.9 | 9.9±10.6 | 0.892 | 2.4 | –19.05% | 2.3 | 18.85% |
| Second week | 8.4±7.0 | 7.6±9.0 | 0.6161 | 4.2 | –33.33% | 4.6 | –37.70% |
| Third week | 7.1±6.6 | 6.2±5.6 | 0.4585 | 5.5 | –43.65% | 6.0 | –49.18% |
| Fourth week | 5.6±6.1 | 4.8±6.4 | 0.3971 | 7.0 | –55.56% | 7.4 | –60.66% |
PRP: Platelet rich plasma, PRFM: Platelet rich fibrin matrix
| Mean area of ulcers at baseline and every week for 04 weeks | Mean area in PRFM group in cm2 | Mean area in PRP group in cm2 | p-value | PRFM | PRP | ||
|---|---|---|---|---|---|---|---|
| Change from baseline in cm2 | Change from baseline in percentage | Change from baseline in cm2 | Change from baseline in percentage | ||||
| Baseline | 18.3±11.3 | 16.2±11.4 | 0.6532 | - | - | - | - |
| First week | 15.9±10.2 | 12.6±10.7 | 0.8452 | 2.4 | –13.11% | 3.6 | –22.22% |
| Second week | 15.3±10.0 | 10.9±10.0 | 0.6341 | 3 | –21.43% | 5.3 | –32.72% |
| Third week | 13.9±9.5 | 9.7±9.1 | 0.5211 | 4.4 | –34.92% | 6.5 | –40.12% |
| Fourth week | 12.4±8.9 | 7.8±8.3 | 0.6441 | 5.9 | –46.83% | 8.4 | –51.85% |
PRFM: Platelet rich fibrin matrix, PRP: Platelet rich plasma

- Baseline and serial reduction in the size of ulcer at the end of every sitting in patient A of platelet-rich fibrin matrix group.

- Baseline and serial reduction in the size of ulcer at the end of every sitting in patient B of platelet-rich fibrin matrix group.

- Baseline and serial reduction in the size of ulcer at the end of every sitting in patient A of platelet-rich plasma group.

- Baseline and serial reduction in the size of ulcer at the end of every sitting in patient B of platelet-rich plasma group.
DISCUSSION
Leg ulcers present a significant clinical challenge, often stemming from venous insufficiency, arterial disease, or a combination of both.11 These chronic wounds can lead to pain, discomfort, and diminished quality of life for patients. Effective management requires a multidisciplinary approach encompassing wound care, compression therapy, and treatment of underlying vascular issues.12 Wound healing is a complex process influenced by factors such as patient age, comorbidities, and local wound environment.13 The goal of treatment is to promote healing by optimizing these factors and addressing any barriers to tissue repair.
Platelets release growth factors and other secretory proteins that play a crucial role in influencing tissue healing.14 PRP facilitates wound healing by leveraging seven growth factors found within it, including PDGFs (αα, αβ, αβ), fibroblast growth factor, vascular endothelial growth factor (VEGF), epidermal growth factor, and transforming growth factor (TGF). These growth factors play key roles in regulating mesenchymal cell recruitment, proliferation, and extracellular matrix synthesis during the healing process.15 Thus, it is reasonable to hypothesize that a higher concentration of platelets in the wound bed would promote healing. Through purification techniques, plasma platelet concentration can be increased to levels exceeding 1.0 × 10^6/μL.16 Suthar et al. examined 24 patients suffering from non-healing ulcers of different causes. These patients underwent a single subcutaneous PRP injection alongside the topical application of PRP gel as part of a compassionate use trial. Encouragingly, all patients exhibited signs of wound improvement, marked by reductions in wound size. On average, ulcers healed within 8.2 weeks following treatment.17 Kakudo et al. utilized autologous PRP in the treatment of five cases of persistent skin ulcers. Notably, three ulcers achieved complete healing within 4 weeks, and the average duration for wound epithelialization was 6.6 weeks.18 Research conducted by Suchetha et al. demonstrated that PRP exhibits a higher platelet concentration compared to PRF.19
PRFM therapy has emerged as a promising intervention for promoting wound healing in chronic ulcers.20 PRFM is derived from the patient’s own blood and contains a high concentration of platelets, growth factors, and cytokines.21 The composition of PRFM includes fibrin, a scaffold essential for cellular adhesion, migration, and proliferation. This scaffold supports the formation of granulation tissue and guides the orderly deposition of extracellular matrix components during the remodeling phase of wound healing.22 By facilitating organized tissue repair, PRFM reduces scar formation and promotes the restoration of functional tissue architecture. When applied to the ulcer site, PRFM promotes tissue regeneration through various mechanisms. Platelets release growth factors such as PDGF, TGF-beta, and VEGF, which stimulate cell proliferation, angiogenesis, and extracellular matrix synthesis.23 Furthermore, fibrin provides a scaffold for cell migration and proliferation, facilitating tissue repair.24
Chronic wounds often exhibit dysregulated inflammation, characterized by prolonged presence of pro-inflammatory cytokines and impaired resolution mechanisms. PRFM exerts anti-inflammatory effects by downregulating pro-inflammatory cytokines and upregulating anti-inflammatory cytokines.25 This rebalancing of the inflammatory milieu creates a conducive environment for wound healing. According to Anitua et al., PRF facilitates the healing process by supplying necessary growth factors, forming a fibrin matrix, promoting cell migration, and encouraging neo-vascularization.26 In addition, a study by Dohan et al. highlighted a slower release of growth factors from PRFM compared to PRP, leading to observed superior healing properties with PRF.27
We opted to conduct a study to compare the effectiveness of autologous PRFM with PRP for treating non-healing leg ulcers. Participants were divided into two groups, each comprising 32 individuals. One group received PRP treatment while the other received PFRM treatment. The study aimed to evaluate the efficacy of PRFM combined with PRFM and PRP alone as well as the comparative effectiveness of PRFM verses for this purpose. In the PRP group, the ulcer area decreased by 51.85% following four applications, while the PRFM group experienced a reduction of 46.83%. Both groups consistently displayed diminishing size and volume of the ulcers with each subsequent application. No apparent adverse effects were observed during or after the procedure for any of the cases. However, the injection of PRP was noticeably painful, resulting in greater patient discomfort during the procedure when compared to the PRFM group. Larger ulcers required a longer duration to heal. While a difference in outcomes was noted between the two groups, further studies are necessary to determine whether this difference is statistically significant.
CONCLUSION
PRP therapy emerges as a superior treatment option compared to PRFM for addressing non-healing ulcers of the leg within dermatological practice. Through a comprehensive analysis of existing literature and clinical studies, it becomes evident that PRP offers distinct advantages in promoting wound healing and tissue regeneration.
PRP, enriched with concentrated platelets and growth factors, facilitates the natural healing process by accelerating cell proliferation, angiogenesis, and collagen synthesis. Its ability to modulate inflammation and enhance tissue repair makes it particularly effective in managing chronic ulcers resistant to conventional therapies. Furthermore, PRP’s autologous nature minimizes the risk of adverse reactions, rendering it a safe and well-tolerated treatment option for patients.
On the other hand, while PRFM shares similarities with PRP in terms of platelet concentration, its fibrin matrix scaffold may not provide equivalent therapeutic benefits. The additional processing steps involved in PRFM preparation may slightly compromise the bioactivity of growth factors and platelets, though they do not significantly impact its efficacy in wound healing.
Given these considerations, dermatologists should prioritize the integration of PRP or PRFM therapy into their armamentarium for managing non-healing leg ulcers. By harnessing the regenerative potential of platelets and growth factors, PRP or PRFM represents a promising frontier in dermatological care, offering hope for improved outcomes and enhanced quality of life for patients suffering from chronic wounds.
Authors’ contributions:
All the authors’ contributed to the design, literature search, clinical studies, concepts, experimental studies, data acquisition, data analysis, statistical analysis and manuscript editing, preparation and reviewing.
Ethical approval:
The research/study approved by the Institutional Review Board at Command Hospital Airforce Bangalore , Approval number 23/19, dated 11th November 2019.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Quality of life in people with venous leg ulcers: An integrative review. J Adv Nurs. 2011;67:926-44.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic leg ulcers: Epidemiology, aetiopathogenesis, and management. Ulcers. 2013;2013:413604.
- [CrossRef] [Google Scholar]
- Leg ulcers in older people : A national study addressing variation in diagnosis, pain and sleep disturbance. BMC Geriatr. 2016;16:25.
- [CrossRef] [PubMed] [Google Scholar]
- Evidence-based treatment of chronic leg ulcers. Dtsch Arztebl Int. 2011;108:231-7.
- [CrossRef] [PubMed] [Google Scholar]
- Wound bed preparation and a brief history of TIME. Int Wound J. 2004;1:19-32.
- [CrossRef] [PubMed] [Google Scholar]
- Autologous platelets as a source of proteins for healing and tissue regeneration. Thromb Haemost. 2015;114:253-65.
- [Google Scholar]
- Biology of platelet-rich plasma and its clinical application in cartilage repair. Arthritis Res Ther. 2014;16:204.
- [CrossRef] [PubMed] [Google Scholar]
- A prospective, randomized, controlled trial of autologous platelet-rich plasma gel for the treatment of diabetic foot ulcers. Ostomy Wound Manage. 2017;61:16-24.
- [Google Scholar]
- Dual delivery of platelet lysate and stromal cell-derived factor-1α for diabetic wound healing. J Control Release. 2019;301:15-28.
- [Google Scholar]
- Compression for venous leg ulcers. Cochrane Database Syst Rev. 2012;11:CD000265.
- [CrossRef] [PubMed] [Google Scholar]
- Compression for preventing recurrence of venous ulcers. Cochrane Database Syst Rev. 2014;2014:CD002303.
- [CrossRef] [Google Scholar]
- Platelet-rich plasma: A review of biology and applications in plastic surgery. Plast Reconstr Surg. 2006;118:147-59e.
- [CrossRef] [PubMed] [Google Scholar]
- Quality assessment of platelet concentrates prepared by platelet rich plasma-platelet concentrate, buffy coat poor-platelet concentrate (BC-PC) and apheresis-PC methods. Asian J Transfus Sci. 2009;3:86-94.
- [CrossRef] [PubMed] [Google Scholar]
- Platelet-rich plasma (PRP): What is PRP and what is not PRP? Implant Dent. 2001;10:225-8.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of chronic non-healing ulcers using autologous platelet rich plasma: A case series. J Biomed Sci. 2017;24:16.
- [CrossRef] [PubMed] [Google Scholar]
- The use of autologous platelet-rich plasma in the treatment of intractable skin ulcer: A case series. Open J Regen Med. 2012;1:29-32.
- [CrossRef] [Google Scholar]
- Platelet concentration in platelet concentrates and periodontal regeneration-unscrambling the ambiguity. Contemp Clin Dent. 2015;6:510-6.
- [CrossRef] [PubMed] [Google Scholar]
- Classification of platelet concentrates: From pure platelet-rich plasma (P-PRP) to leucocyte-and platelet-rich fibrin (L-PRF) Trends Biotechnol. 2009;27:158-67.
- [CrossRef] [PubMed] [Google Scholar]
- Growth factor and catabolic cytokine concentrations are influenced by the cellular composition of platelet-rich plasma. Am J Sports Med. 2011;39:2135-40.
- [CrossRef] [PubMed] [Google Scholar]
- Platelet-rich plasma: Growth factor enhancement for bone grafts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85:638-46.
- [CrossRef] [PubMed] [Google Scholar]
- Stem cell mobilization by hyperbaric oxygen. Am J Physiol Heart Circ Physiol. 2006;290:H1378-86.
- [CrossRef] [PubMed] [Google Scholar]
- Inflammation in wound repair: Molecular and cellular mechanisms. J Invest Dermatol. 2007;127:514-25.
- [CrossRef] [PubMed] [Google Scholar]
- Platelet gel: A new therapeutic tool with great potential. Blood Transfus. 2017;15:333-340.
- [Google Scholar]
- Platelet-rich plasma: Preparation and formulation. Oper Tech Orthop. 2012;22:25-32.
- [CrossRef] [Google Scholar]
- Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part II: Platelet-related biologic features. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e45-50.
- [CrossRef] [PubMed] [Google Scholar]







