Translate this page into:
A resident’s guide to skin cancer minor surgery
*Corresponding author: Celine Jose, Department of Plastic Surgery, Norfolk and Norwich University Hospital NHS Foundation Trust, Norwich, United Kingdom. celinejose.3@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Jose C, Asher CM. A resident’s guide to skin cancer minor surgery. J Cutan Aesthet Surg. doi: 10.25259/JCAS_150_2024
Abstract
Local anesthetic skin cancer surgery is essential diagnostically and therapeutically in dermatology and plastic surgery. Proper training requires vigilant oncological control and the implementation of optimal reconstructive principles. This article illustrates key principles of the surgical approach to resection and reconstruction of a skin cancer defect. These techniques aim to optimize patient comfort, reduce the risk of inadvertent oncological compromise and highlight approaches to reconstruction in different anatomical areas. Local anesthetic skin cancer surgery is essential in the treatment of skin cancer. It also offers an opportunity for even the most junior resident doctors to perform minor procedures. Improved understanding of ways to maintain oncological control and how to approach reconstruction in different anatomical areas is essential to optimizing patient-centered outcomes and improving the confidence of those performing the surgery.
Keywords
Minor procedure
Scar orientation
Skin cancer
Skin surgery
INTRODUCTION
Local anesthetic lists are a daily facility within skin cancer units in the United Kingdom (UK) and are an excellent training opportunity for even the most junior resident doctors.1 There are an estimated 22,000 cancer patients, including those with skin cancer, awaiting appointments according to Cancer Research UK,2 so the expanded use of residents to participate in the diagnosis and treatment of skin cancer is an avenue worth exploring.
Despite their ambitious aims to deal with the more complex skin cancer and reconstructive cases, residents in dermatology and plastic surgery need to have a solid foundation of basic surgical skills in the context of oncological surgery when conducting even the simplest of cases.
COMMON SKIN CANCERS
Basal cell carcinoma (BCC) is a common and slow-growing, locally invasive skin cancer with a low risk of metastasis.3 It typically appears as pearly or translucent nodules with telangiectasia on sun-exposed areas.
Squamous cell carcinoma (SCC) carries a higher risk of metastasis and typically presents as keratotic nodules with a central crater of crust with a shorter period of growth.3
Melanoma leans toward the more aggressive end of the spectrum of skin cancers arising from melanocytes. They typically have a pigmented appearance with irregular borders and color distribution. Potential symptoms include itching, bleeding, or simply a sudden change in the appearance of a preexisting mole. It can progress quickly and has high metastatic potential.4
Early diagnosis and treatment of skin cancer is crucial for reducing morbidity, mortality, and recurrence rates. Patients often need ongoing follow-up in the community or under a member of the skin cancer multidisciplinary team due to likely actinic field change posing the risk of further skin cancers. Surgery is often the first-line treatment for many skin cancers because it facilitates histological diagnosis and offers definitive treatment.
There are several definitions that residents need to appreciate.
DEFINITIONS
Diagnostic excision biopsy
An excision of the entirety of the lesion with a 1–2 mm margin of normal surrounding skin and a cuff of fat.5
Mark the lesion, including the surrounding unstable skin, and mark the excision margin before local anesthetic administration.
Therapeutic excision biopsy
This is a therapeutic excision with the intent to treat and, therefore, reduce the risk of local recurrence. However, it is based on a clinical diagnosis without prior histological diagnosis.
Excision margins will vary depending on the lesion and can be facilitated by guidelines.6,7 As this is based on a clinical diagnosis, it typically applies to three categories of skin lesions:
Benign but symptomatic
Excise with a 2 mm margin and a cuff of fat.
Basal cell carcinoma (BCC)
A typical, nodular, and well-defined BCC is excised with a 4 mm margin and a cuff of fat, high-risk lesions with a 5 mm margin, with fat, to the next tissue plane, which is clinically normal.6
Squamous cell carcinoma (SCC)
These are usually excised with a 4 mm, 6 mm, or 1 cm peripheral margin, down to the fascia, depending on features of aggression. Where reconstruction necessitates a skin graft or flap, consider excision to a deeper plane to minimize the risk of an incomplete deep margin requiring re-excision including the reconstructive tissue. For example, excision to periosteum on the scalp instead of the galea aponeurotica in a mobile, but exophytic clinical SCC which will require a graft.7
The intention of treatment is to obtain clearance and reduce the risk of recurrence. Oncologically, this means obtaining a minimum of 1–2 mm (1 mm for SCC,7 1 mm for nodular BCC, and >2 mm for other histological types of BCC6) from the nearest histologically detected cancer. This results in a 92–95% rate of clearance and a 17–22% reduced rate of reoccurrence.6 A sound clinical assessment of the margins of clinically abnormal skin is best performed with the aid of magnification—using a dermatoscope or surgical loupes and a good-quality light source.6,8 A high index of suspicion for neurovascular invasion or fixity to underlying structures should be considered.
Where melanoma is suspected, a diagnostic excision, as outlined earlier, is performed in the first instance to obtain a Breslow thickness before proceeding with a therapeutic excision.9
LOCAL ANESTHESIA ADMINISTRATION
Inject your local anesthetic in parallel to sensory nerve orientation, giving this 1st injection a moment to work before administering the remainder.10 Subsequent injections should be less sensitive. Avoid injecting into the skin lesion directly, reducing the theoretical risk of seeding potential tumors elsewhere [Figure 1].

- Administering local anesthetic agent in the direction of sensory nerve.
As you inject, observe if the lesion elevates off underlying structures (fascia/bone) or if it remains fixed. Depending on anatomical location and defect size, fixity may increase the complexity of the reconstruction required.
When using adrenaline, allow its hemostatic effects to have time to work. Consider administering the injection, drafting your paperwork, and then scrubbing for the case. This will reduce the tendency to start before it has had any hemostatic effect while maintaining some operative efficiency.
SURGICAL TECHNIQUE
Good oncological practice requires you to obtain a specimen that is histologically examinable and uncrushed without contamination of neighboring skin. Techniques to uphold this include:
Use of a different needle for injection of local anesthetic for each skin cancer being excised on the same patient
Skin preparation of normal skin first, then the cancer site; the reverse will seed “dirty” to clean
Avoid overhandling the specimen with forceps; a skin hook for retraction may be less traumatizing11
Avoid gauze used for absorbing blood also brushing the cancer and then resting on normal skin
Remove instruments used for excision and use fresh instruments and gauze for closure of skin
Where multiple tumors are being excised, use a fresh suture for each closure. The leftover of one suture can be used for the marker suture; a clip can be placed on the specimen for orientation until the marker suture is placed
SCAR ORIENTATION WITH ANATOMICAL CONSIDERATIONS
Limbs
Where possible, mark your elliptical extension in a vertical orientation. Laxity is circumferential, lymphatics run longitudinally, so you preserve more this way, reducing edema. If subsequent excision and reconstruction are required, a vertical orientation is usually favorable [Figure 2].12
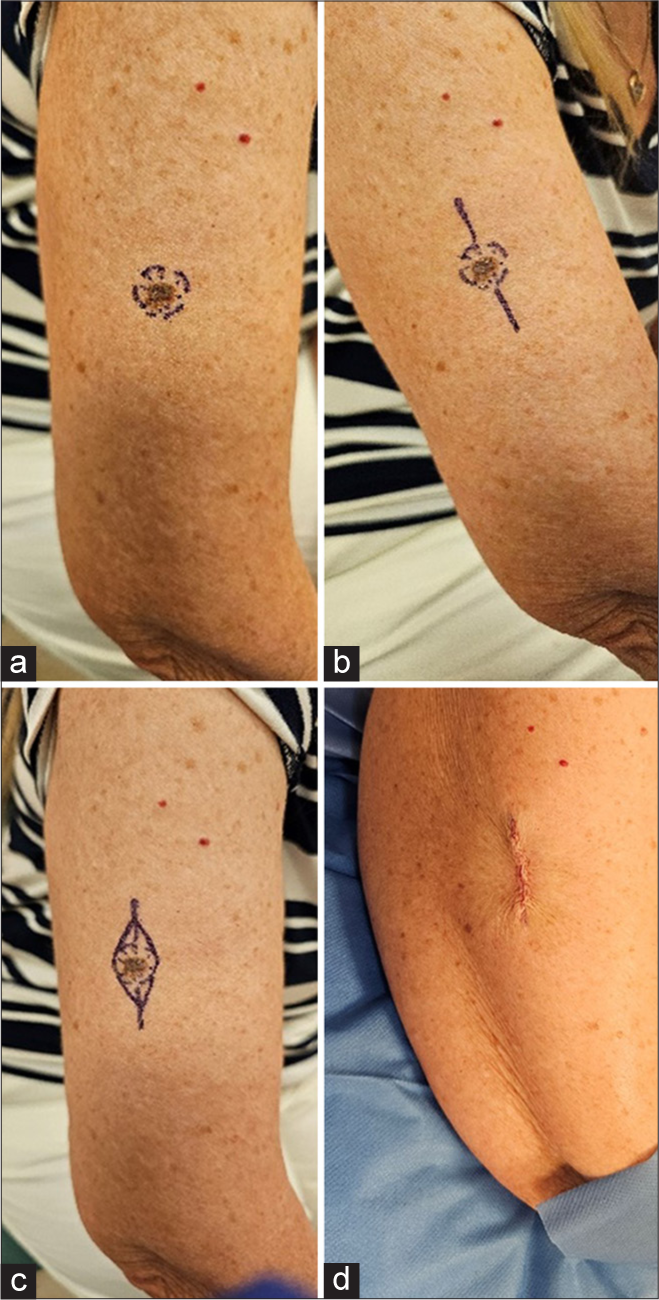
- (a) Skin lesion marked, (b) marking the lesion to make a longitudinal orientation drawing maximum laxity, (c) excision margins marked with edges touching the ellipse, (d) post-excision of lesion – longitudinally oriented scar.
Face
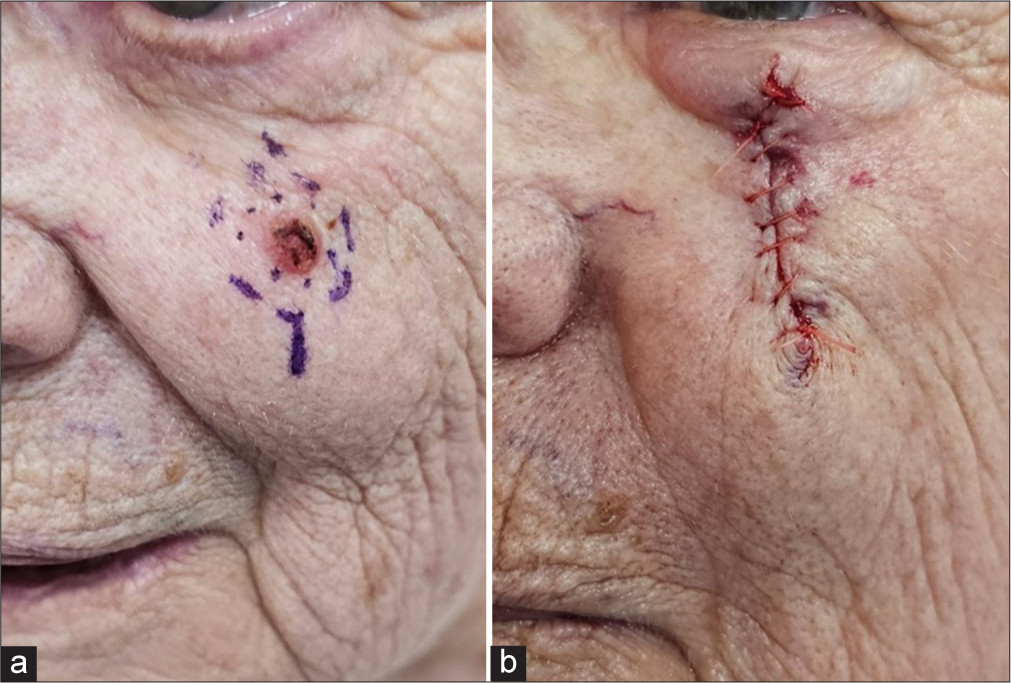
Mark the margins, usually circular, and excise as a circle in the first instance. Skin is elastic, and the orientation of the different muscle fibers of the face often allows you to draw laxity from different directions to support closure without an ellipse. Any excess skin that creates a standing cone (dog ear) can be removed at the end, often a smaller (burrows) triangle than your predicted pre-marked ellipse [Figure 3].

- Skin lesion marked with edges making a circle.
Post-auricular
Tumors within the post-auricular sulcus can be amenable to direct closure by advancing skin from the posterior ear, creating an effect similar to pinnaplasty. However, if you suspect an invasive tumor, it may be preferable to place a skin graft here. This will facilitate earlier identification of a reoccurrence in an anatomical area with an invasive path that can extend to the base of the skull.
Lower lid
A vertical orientation is more favorable to a transverse scar. The latter has a greater risk of causing ectropion [Figure 4].
- Skin lesion marked, (b) post-excision of skin lesion – vertically oriented surgical wound.
Trunk
Assess the direction of the Resting Skin Tension Lines (RSTLs). Mark the lesion’s margins, and extend this into an ellipse into these RSTLs. Consider the movements that will put this wound under the most tension. The closure needs to withstand this [Figure 5].
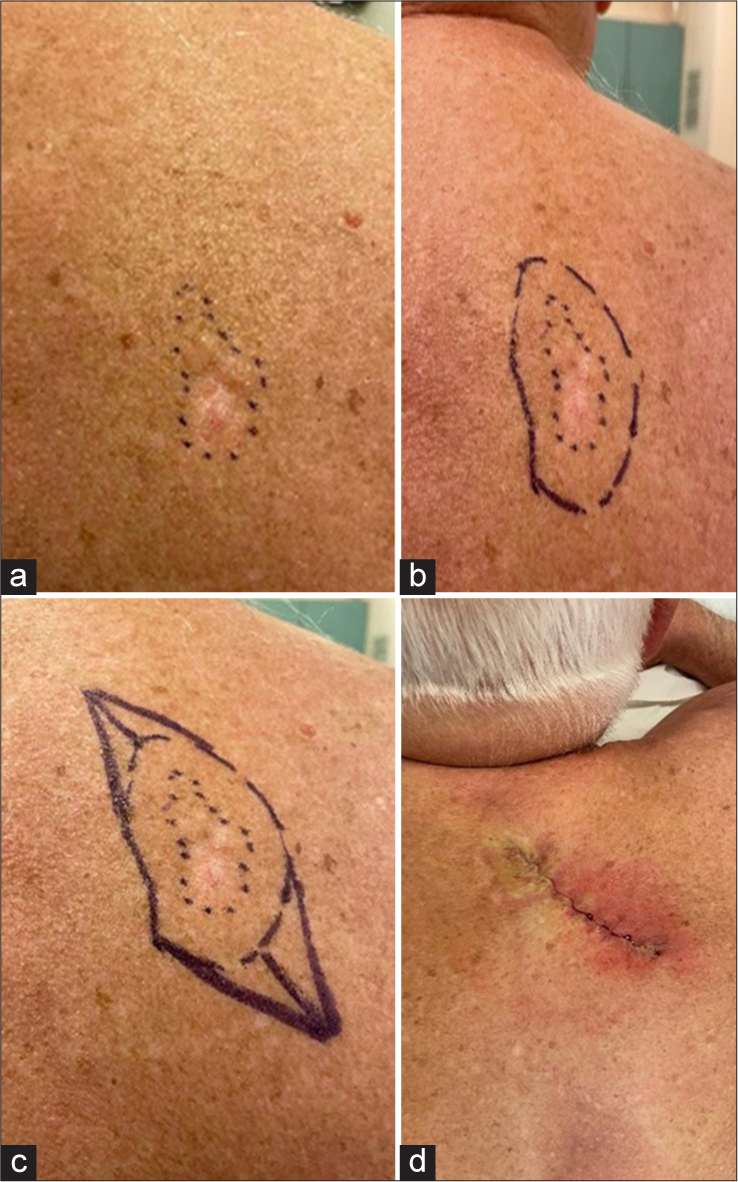
- (a) Edges of skin lesion marked, (b) marking with adequate excision margin, (c) making an ellipse in the direction of resting skin tension line, (d) post-excision of lesion
Mohs surgery
Mohs micrographic surgery is advantageous for lesions on the face, where tissues are often not in excess for reconstruction but routine excision poses the risk of high morbidities, such as in the periocular and nasal regions, and with poorly defined or histologically aggressive skin cancers such as morphoeic, micronodular and infiltrative BCCs, and recurrent tumors.13
It offers the advantage of a targeted, complete excision before reconstruction, without significant delay between diagnosis and treatment, with greater preservation of histologically uninvolved skin.14
LEARNING POINTS
The intent of the procedure, diagnostic or therapeutic, determines the margin for excision.
Give local anesthetic with consideration to the direction of sensory nerves.
Sound oncological surgical practice will prevent the risk of tumor seeding to the local area.
The orientation of scars should be optimized to the anatomical site and local structures 5. Mohs micrographic surgery should be actively considered for high-risk cases.
CONCLUSION
Skin cancer minor surgery provides a valuable training ground for junior residents to develop essential procedural skills within the context of oncological care. A sound understanding of excision principles, appropriate anesthetic techniques and lesion handling is key to achieving clear margins and reducing the risk of recurrence. Careful planning of scar orientation, appropriate margin selection and clear documentation support both patient outcome and clinical learning. Early exposure to structured techniques lays a strong foundation for future practice in skin cancer surgery.
Authors’ contributions
Conceptualization: Christian Marlon Asher, Methodology: Celine Jose, Resources: Christian Marlon Asher (Lead), Celine Jose (equal), Supervision: Christian Marlon Asher, Writing – original draft: Christian Marlon Asher (lead), Celine Jose (supporting), Writing – review & editing: Celine Jose (lead), Christian Marlon Asher (supporting).
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Core training and surgical opportunities: A UK-based analysis. J Clin Transl Res. 2022;8:557-62.
- [Google Scholar]
- Cancer waiting times report 2023. 2023. NHS England. Available from: https://www.england.nhs.uk/statistics/statistical-work-areas/cancer-waiting-times [Last accessed on 2024 Oct 08]
- [Google Scholar]
- Dermatology handbook for registrars, updated edition 2022. Available from: https://cdn.bad.org.uk/uploads/2022/08/24112653/dermatology-handbook-for-registrars-2022.pdf [Last accessed on 2025 Jan 20]
- [Google Scholar]
- A review of epidemiology and cancer biology of malignant melanoma. Cureus. 2021;13:e15087.
- [CrossRef] [Google Scholar]
- Biopsy for malignant melanoma-are we following the guidelines? Ann R Coll Surg Engl. 2008;90:322-5.
- [CrossRef] [PubMed] [Google Scholar]
- British Association of Dermatologists guidelines for the management of adults with basal cell carcinoma 2021. Br J Dermatol. 2021;185:899-920.
- [CrossRef] [PubMed] [Google Scholar]
- British Association of Dermatologists guidelines for the management of people with cutaneous squamous cell carcinoma 2020. Br J Dermatol. 2021;184:401-4.
- [CrossRef] [PubMed] [Google Scholar]
- Marking a surgical margin for excision of a keratinocyte cancer. Aust J Gen Pract. 2021;50:385-7.
- [CrossRef] [PubMed] [Google Scholar]
- NG14: Skin cancer: Assessment and management. 2015. Available from: https://www.nice.org.uk/guidance/ng14/chapter/Recommendations#assessing-melanoma [Last accessed on 2025 Jan 21]
- [Google Scholar]
- How to minimize the pain of local anesthetic injection for wide awake surgery. Plast Reconstr Surg Glob Open. 2021;9:e3730.
- [CrossRef] [PubMed] [Google Scholar]
- Scar orientation: Principles in plastic surgery. J Cutan Aesthet Surg. 2020;13:152-3.
- [CrossRef] [PubMed] [Google Scholar]
- Mohs micrographic surgery versus surgical excision for periocular basal cell carcinoma. Cochrane Database Syst Rev. 2014;2014:CD007041.
- [CrossRef] [PubMed] [Google Scholar]






