Translate this page into:
A Split Face Study to Compare the Efficacy of Platelet Rich Plasma Versus Normal Saline Injections in Acne Scars and to Assess the Utility of Ultrabiomicroscopic Sonography in Evaluation of Treatment Response
Address for correspondence: Dr. Meena Bhaskar Makhecha, Department of Dermatology, OPD no 17, Ground floor, HBTMC & Dr R N Cooper hospital, Bhaktivedanta Swami Rd, Juhu, Mumbai 56. E-mail: drmmakhecha2021@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
Multiple studies have proposed the effectiveness of Platelet rich plasma (PRP) in treatment of atrophic acne scars. But an unanswered question is - whether it is the presence of growth factors in PRP or the mechanical factors during the injection that are responsible for its effectiveness? Also, no study compares PRP as a monotherapy against inert solution like normal saline (NS), that too, in a split face pattern using a non-invasive objective evaluation method.
Aims:
Primary – To compare the efficacy of intralesional PRP and NS injections, in the treatment of atrophic acne scars. Secondary - To assess the side effect profile of the PRP injections.
Study Design:
Prospective Interventional Comparative Split Face study
Materials and Methods:
30 out of 33 patients completed the study and 20 of them were subjected to Ultrabiomicroscopic (UBM) analysis. Each patient received intralesional injections of NS and PRP in a split face pattern at two weekly intervals for five sittings. Treatment response was assessed using Goodman And Baron qualitative grading system, photographic evaluation by two blinded dermatologist and UBM analysis (scar depth & length).
Results:
All the three methods showed a statistically significant treatment response. However, there was no significant inter group difference and PRP and NS had similar efficacy in treating acne scars.
Conclusion:
We conclude that subscision like mechanical effect of injecting solution is more important than the nature of the solution in treatment of atrophic acne scars and UBM sonography can be proposed as an objective assessment tool for such studies.
Keywords
Acne scars
NS
platelet rich plasma
PRP
ultrabiomicroscopic sonography
INTRODUCTION
Acne vulgaris can often lead to permanent scarring as an unfortunate complication. Apart from the cosmetic effect, post acne scars have an adverse impact on patients psyche and quality of life.[1] The utility of Platelet rich plasma (PRP) in treatment of various indications like Androgenetic alopecia (AGA), Skin rejuvenation, endometrium regrowth etc has been increasing. The main action of PRP in all these cases is growth factor mediated stimulation of tissue stem cells leading to tissue regeneration.[23] Recently, PRP injections are also being used in the treatment of atrophic acne scars with clinically perceptible results.[4] But, as far as ascertained, no study has evaluated the effectiveness of PRP injections as monotherapy as compared to an inert physiological solution like Normal Saline (NS), in a split face pattern for this indication.[5]
Also, a major lacuna in acne scar treatment literature is the lack of simple, non-invasive objective evaluation method for assessing treatment response as most of the studies use a subjective grading system for scar evaluation.[5]
Aims
A Split face study was conducted with the following aims:
Primary – To ascertain the efficacy of intralesional PRP injections in the treatment of atrophic acne scars as compared to intralesional NS injections using subjective and objective means.
Secondary - To assess the side effect profile of the intralesional PRP injections.
MATERIALS and METHODS
A total of 33 patients were enrolled in the study, out of which, 30 patients completed the treatment and 20 patients underwent Ultrabiomicroscopic sonography (UBM).[6] Patients aged more than 18 years, any gender, and with atrophic acne scars on face were included. Prior institutional ethical clearance was taken. Patients with active acne, keloidal tendency, bleeding diathesis, active infection at the treatment site, those on any immunosuppressive therapy or with history of systemic retinoids intake in previous 6 months and pregnant and lactating women were excluded from the study. Patients were explained in detail about the procedure, time required, possible side effects, and prognosis of the treatment. A written informed consent of all the patients was obtained at the start of the study. Thorough history of each patient was taken including demographic history, disease history – age of onset, frequency, and duration – treatment history, family history, and personal history. Clinical and dermatological examination was performed and grading of the acne scars was done according to the Goodman and Baron’s qualitative global acne scarring grading system.[7] A total of five treatment sessions were given to each patient over a period of 2 months at an interval of 2 weeks each. Treatment area was painted with povidone iodine and cleansed with spirit before the procedure and then was anesthetized using a thick application of topical anaesthetic cream (combination of prilocaine 2.5% and lignocaine 2.5%) under occlusion for about 45 min before the procedure. Autologous pure PRP (P-PRP) (according to the classification proposed by Ehrenfest) was prepared using a double spin method, wherein 6 – 10 ml of whole blood was collected from median cubital vein in a vacutainer containing anticoagulant acid citrate dextrose - A and centrifuged for first spin at 1500rpm for 15minutes at 20°C.[8] It was done to separate plasma with platelets and white blood cells from red blood cells (RBCs). RBCs being heavy settled down at the bottom. The plasma and buffy coat were gently aspirated from each tube and transferred to a second tube (plain vacutainer bulb without anticoagulant). The plasma and buffy coat were centrifuged again at 2000 rpm for 10 mins at 20°C. After centrifugation, upper two third, being poor in platelets, was platelet-poor plasma (PPP) and lower one third, being rich in platelets, was PRP. First, PPP was gently aspirated to avoid its mixing with PRP and then discarded. Then, residual PRP was aspirated and used for injections through a 30-gauge insulin syringe. The platelets in PRP were counted with the help of automated machine. The concentration of platelets in PRP was approximately 4–4.5 times that of the baseline.
No activator was added in PRP before injection, since collagen acts as a natural activator of PRP when used in soft tissue.[9] Each patient was given 0.1- 0.3 ml intralesional injections of PRP in individual scars on right half of face and similarly, intralesional NS was injected on left side of face at each sitting. The amount injected was sufficient to elevate the scar, and the end point was taken as blanching and elevation of the scar. After injecting, the site was gently massaged and compressed for a few seconds to control the bleeding. Ice pack was put when required. Topical antibiotic cream (fusidic acid 2% cream) was applied to the treated area. After the procedure, the patients were prescribed topical sunscreen.
Clinically, response to treatment was graded using the standard Goodman and Baron (G &B) quantitative grading scale for post acne scarring done at the start of treatment and one month after treatment completion.[7] Digital photographs were taken (three shots each of profile and side views at a distance of 30 cm and 15 cm respectively) at the start of treatment and one month after treatment completion. The photographs were evaluated by two separate, non-treating, blinded dermatologists on an arbitrary six-point scale (0: No improvement, I: < 20%, II: 20 -40%, III: 40 – 60%, IV: 60–80%, V: 80–100%). A pre and post treatment UBM was performed on selected scars (Ice-pick or box car scars) using a 50 Hz probe. The parameters assessed were: 1. Dermal thickness underlying the scar 2. The diameter of the scar 3 The echotexture of scar & 4. The presence of any other dermal structures, like cysts and calcifications.
The severity of pain experienced by the patient during the procedure was assessed using a 10 cm length visual analogue scale (VAS). The VAS consists of a straight line with the endpoints defining extreme limits such as ‘no pain at all’ and ‘pain as bad as it could be’. The patient is asked to mark his pain level on the line between the two endpoints. The distance between ‘no pain at all’ and the mark then defines the subject’s pain.[10] Adverse effects like post inflammatory hyperpigmentation or any other were noted during the treatment period and one month following the last session.
RESULTS
The continuous variables with repeated measures were analysed by the Schreier-Ray-Hare Test. Categorical data was analysed using Chi-square test and Fisher Exact test. P < 0.05 (2-tailed) was used to identify statistical significance. UBM parameters were analysed by two –way repeated measure ANOVA. All analyses were performed using IBM SPSS Version 21.0 and Microsoft Office Excel 2007.
The mean age of the patients in the study group was 26.1 years. Out of total 33 patients, 17 were males and 16 were females. 79 % of the patients were of Fitzpatrick skin type 4.[11] The most common type of scars were Ice-pick scars (64.2%), Boxcar scars (25.5%), and Rolling scars (10.2%).
Primary outcome measures
In terms of evaluation on the basis of G & B grades, 26.7% (8/30) of patients had improvement by 1 grade and 3.3% (1/30) patients had improvement by 2 grades on PRP side. Similarly, 26.7% (8/30) of patients had improvement by 1 grade and 3.3% (1/30) patients had improvement by 2 grades on NS side. Thus, G & B grades in both groups improved significantly after treatment (P 0.00102), but there was no significant difference (P 0.842) in between the two treatment groups.
According to photographic evaluation by blinded dermatologists, 26.7% (8/30) had 60–80% improvement,50% (15/30) of patients had 40–60% of improvement, 20% (6/30) had 20–40% improvement and 3.3% (1/30) patients had 0–20% improvement on PRP side. While on NS side, 23.3% (7/30) had 60–80% improvement, 60% (18/30) of patients had 40–60% improvement, 13.3% (4/30) had 20–40% improvement and 3.3% (1/30) patients had 0–20% improvement. A significant improvement in the grade of scars was observed over time (P 0.016) in both the groups. However, the treatment groups did not show any inter-group significant difference (P 0.857). [Figure 1].
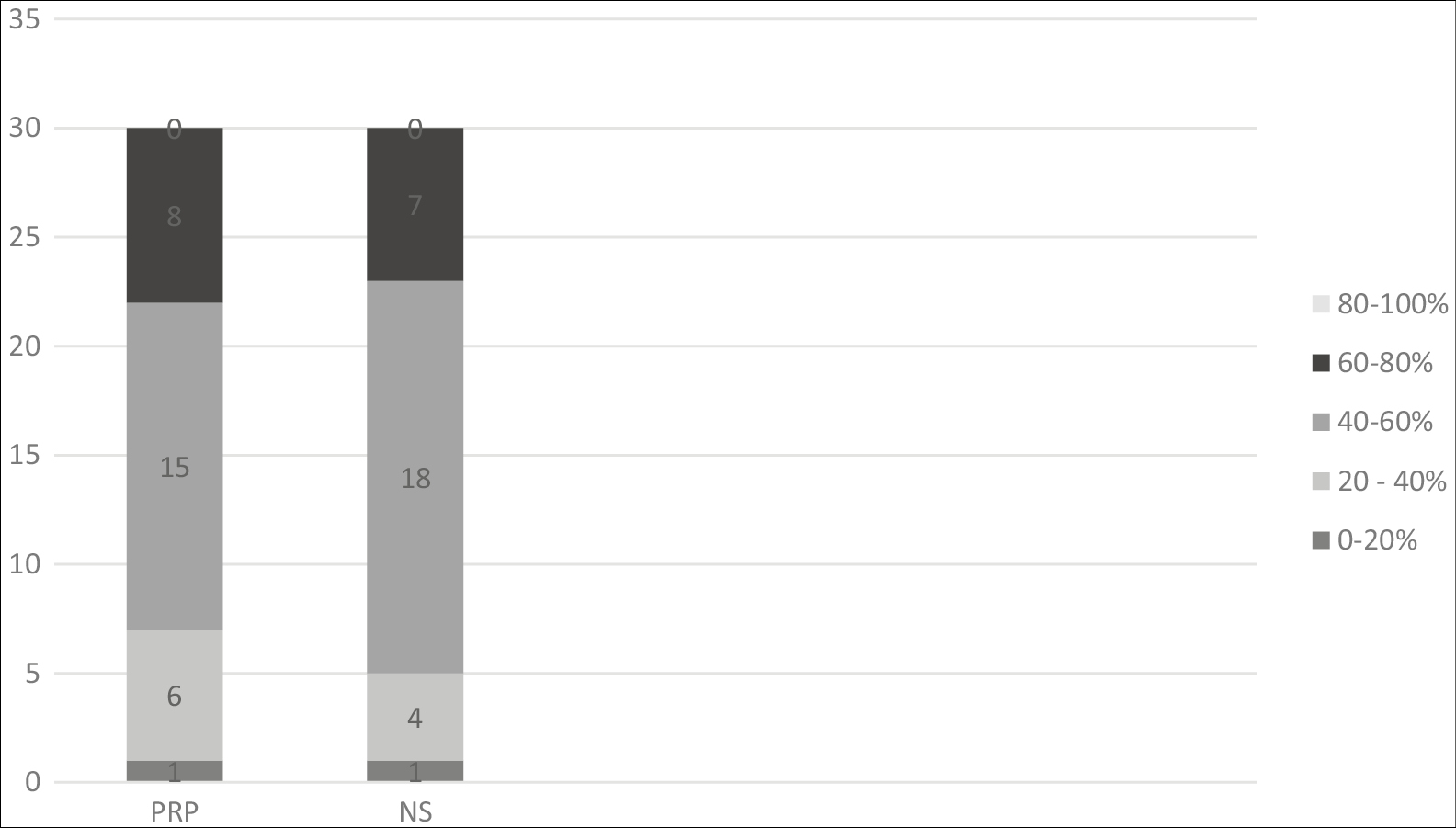
- Graph showing overall improvement in each group as per expert evaluation. 1 patient in both the groups had 0 to 20% improvement, 6 patients in PRP and 4 patients in NS group had 20% to 40% improvement, 15 patients in PRP and 18 patients in NS group had 40% to 60% improvement, 8 patients in PRP and 7 patients in NS group had 60% to 80% improvement
In 20 patients who were evaluated with UBM, there was a mean improvement of 25.35% (0.364mm) and 25.65% (0.343mm) in scar thickness (in the underlying dermis) in PRP and NS groups respectively. Statistical analysis showed a significant improvement in the scar thickness from pre-treatment levels to post-treatment (P 0.039, partial η2 = 0.205). However, the treatment groups did not show a significant inter group difference (P 0.286, partial η2 = 0.060). There was a mean improvement of 24.98% (0.44mm) and 27.48% (0.37mm) in length of the scars on PRP and NS sides. But the difference was not statistically significant (P 0.209, partial η2 =0.082). The echotexture of the treated scars became more hyperechoic compared to baseline in all the patients. The number of cysts and calcifications remained the same before and after treatment.
Secondary outcome measures
The main side effects of the treatment were pain during the procedure and post inflammatory hyperpigmentation (PIH). Most patients in PRP group had VAS score 6 (n = 16), whereas in NS group, most frequent VAS score was 4 (n = 4) The VAS scores were significantly higher in PRP group compared to NS group (P 0.000003). [Table 1]. 3 out of 33 patients dropped out of study due to severe pain (VAS = 10) perceived on PRP side. None of the patients developed severe PIH. On PRP side, 10 patients (33.3%) developed mild PIH & 5 (16.7%) developed moderate PIH. On NS side, 10 patients developed mild PIH (33.3%) & 2 (6.7%) patients developed moderate PIH [Figure 2]. The odds ratio (0.686) did not show any significant difference in the incidence of PIH between the treatment groups.
| Pain Score | Number of participants (Percentage) | p value | |
|---|---|---|---|
| Left side (Group NS) | Right side (Group PRP) | ||
| 4 | 16 (48.5) | 0 (0) | <0.0005*
0.000003 |
| 6 | 11 (33.3) | 16 (48.5) | |
| 8 | 6 (18.2) | 12 (36.4) | |
| 10 | 0 (0) | 5 (15.2) | |
*Significant at 0.05 level of significance. For pain score more than or equal to 6 Fischer-exact test applied.
The severity of pain during injections was significantly higher in PRP group compared to Normal Saline group (P 0.000003)
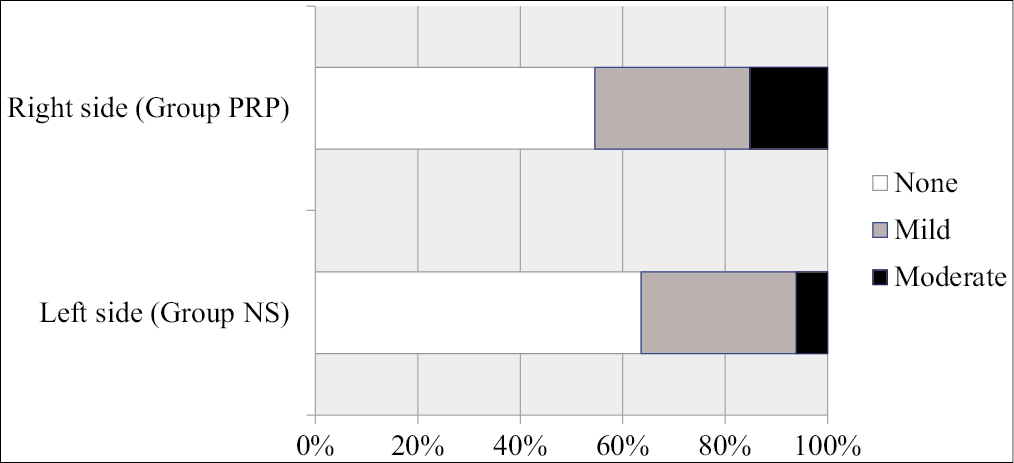
- Graph showing incidence of post-inflammatory hyperpigmentation in the two treatment groups.
- The odds ratio (0.686) did not show any significant difference in the incidence of PIH in between the treatment groups
The odds ratio (0.686) did not show any significant difference in the incidence of PIH in between the treatment groups
DISCUSSION
In this study, 30 % of patients in both the groups showed improvement in G & B grades. It is difficult to report minute improvements in scar using the four grades of G & B grading. Hence, additionally, a photographic evaluation method on a six-point scale by two non-treating, blinded dermatologists was used to improve the accuracy of the assessment. An improvement of more than 20% in appearance of acne scars was recorded in 96.7% and 96.6% patients in PRP and NS groups respectively. Overall, it was observed that rolling and boxcar scars had more appreciable improvement then ice pick scars, but the individual scar-wise statistics were not maintained [Figure 3]. The changes in UBM parameters were also coherent with clinical findings. All patients who were evaluated with UBM, showed Improvement in scar thickness on both the sides (P=0.039). The diameter of majority of scars decreased on both sides, but the difference was not statistically significant (P=0.286). Increased dermal thickness of the scar and increased hyperechogenic texture on USG, both, are indicators of increased collagen content underlying the scar[12] [Figure 4]. The main advantage of UBM is that it is possible to detect and quantify minute changes in scar characteristics which may be missed by subjective grading systems used so far. Thus, the observations by all the three methods consistently showed that both NS and PRP had significant improvement in acne scars and PRP injections have no better efficacy than NS injections.
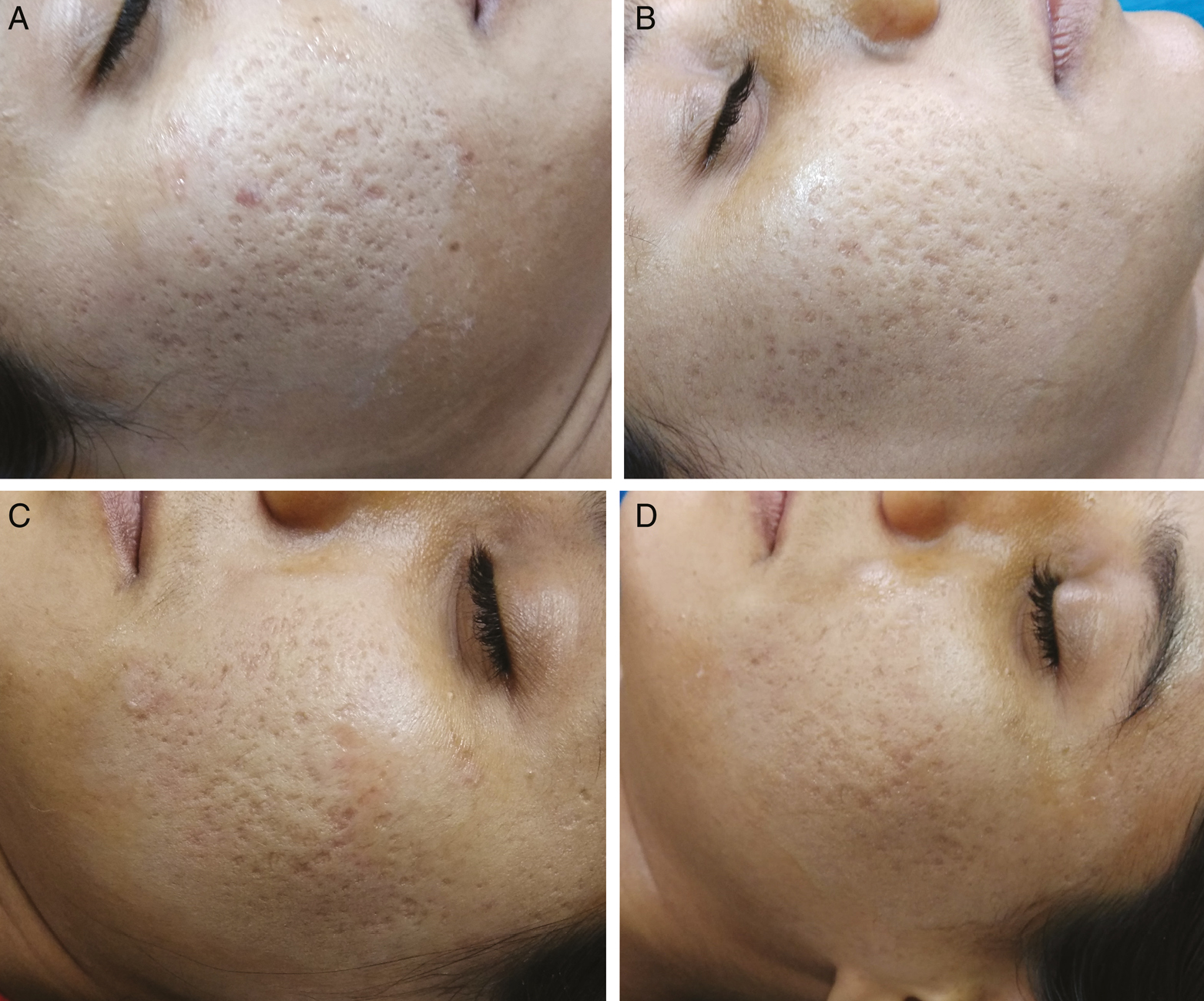
- 24-year-old female right side of face (A & B), treated with PRP injections & left side of face (C & D), treated with NS injections. A: Pre-treatment photograph before first treatment session, showing multiple scars of all the three types with G&B grade 4. B: Post-treatment photograph 1 month after the last treatment session, showing remarkable improvement of 60–80% and shift to G&B grade 3. C: Pre-treatment photograph before first treatment session, showing multiple scars of all the three types with G&B grade 4. D: Post-treatment photograph 1 month after the last treatment session, showing remarkable improvement of 60–80% and shift to G&B grade 3
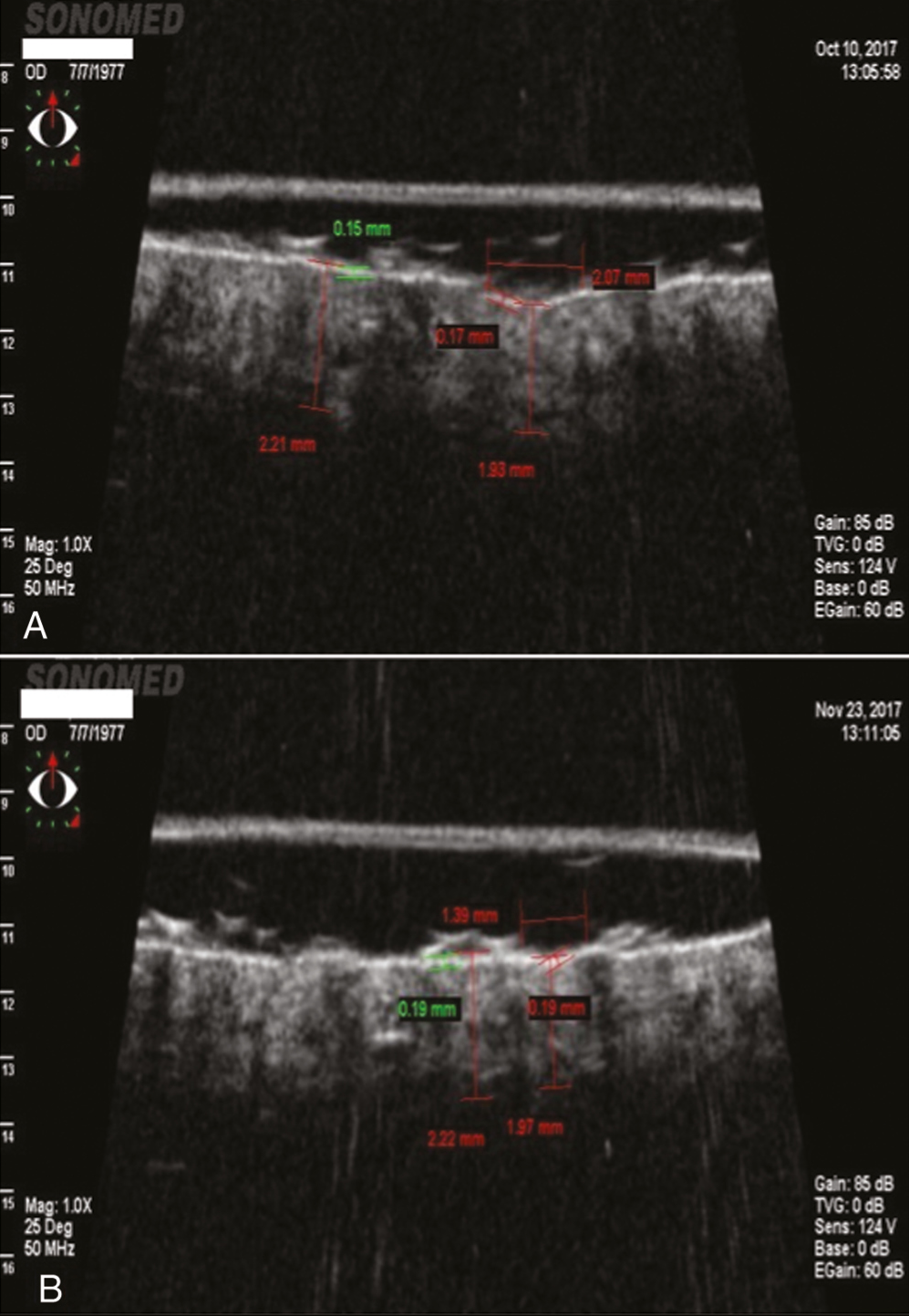
- Pre & Post treatment photographs of UBM analysis of acne scar. A: Pre-treatment photograph before first treatment session, showing a scar of 2.07 mm diameter and 1.93 mm in thickness. B: Post-treatment photograph of the same scar 1 month after the last treatment session, showing reduction in diameter of the scar to 1.39 mm and increased thickness of 1.97 mm
The intralesional treatments can be split into two components:
The process of injection and
The property of the Injecting fluid i.e., PRP/ NS
While giving any intralesional injection into a scar, there is a certain amount of subscision effect. This is due to the trauma caused by injecting needle and tissue separating effect of the injected solution. It leads to disruption of fibrotic collagen fibres tethering the scarred skin to underlying structures and improvement in appearance of the scar. Also, the clot formed during injection serves to provide a scaffold for trapped white blood cells (WBC`s) and Platelets to release growth factors. A study conducted by Baghreni et al, also had similar outcomes.[13] Hence, any intralesional injection treatment for acne scar will have certain baseline improvement due to sheer subscision effect of the injecting needle and the injected solution.
The main constituents of PRP are growth factors and bioactive factors present in the Alpha granules (Platelet-derived growth factor, Transforming growth factor-β, vascular endothelial growth factor and epithelial growth factor) and the dense granules (serotonin, histamine, dopamine, calcium and adenosine) respectively.[14] These are responsible for successful action of PRP in dermatological indications like AGA and ageing skin.[2] In AGA, there is androgen mediated miniaturisation of hair follicles,[15] and in ageing skin, primarily, there is a relative paucity of dermal fibroblast function leading to inability to maintain dermal structural integrity.[16] In both these indications, PRP growth factors act by stimulating hair stem cells, dermal fibroblasts, endothelial cells, and epidermal cells leading to reversal of miniaturisation, cellular proliferation, matrix formation, and collagen synthesis.[2]
Dermal fibroblasts are one of the major targets of growth factors present in PRP. Platelet derived growth factor (PDGF) present in PRP acts on PDGF-BB receptor of dermal fibroblast to stimulate Wnt2 and Wnt4 mRNA expression. These in turn, have chemotactic, mitogenic, angiogenic, and stimulatory effects, leading to modification of extracellular matrix by stimulating collagen, collagenase and glycosaminoglycan synthesis.[1718]
In acne, inflammation is present in follicular and perifollicular areas, extending from subepidermal region to subcutaneous tissue, depending on the severity and site of involvement. This leads to development of atrophic scars with absent epidermal appendages such as hair follicles, sweat glands and compromised subcutaneous adipose tissue which are the seat of dermal stem cells for tissue regeneration. Also, there is replacement of normal basketweave collagen with thick fibrous collagen and loss of significant amount of elastin and fibroblasts in the dermis.[1920] Hence, majority of target cells for PRP action are missing in acne scars. These explains why the presence of active components in PRP failed to give better results than inert NS solution.
Thus, from the understanding of pathological differences between various indications of PRP, and observations of this study, it can be inferred that in case of atrophic acne scars, physical factors implicated during the process of injection contribute more to improvement in scar appearance, rather than the type of injecting solution.
On the other hand, the severity of pain was significantly more on PRP side in all the patients in this study. This needs to be weighed against the observation that both PRP and NS had statistically similar treatment outcomes.
To the best of our knowledge, this is the first study to use UBM for objectively evaluating treatment response in acne scars. It is a non-invasive mode of investigation. Hence, it becomes a convenient procedure to assess cosmetically important areas of the body like face, thus, avoiding other invasive interventions like histopathology.
Limitations
Small sample size and short follow up period are the major limitations of this study.
CONCLUSION
From the results of this study, it is concluded that probably it is the mechanical, subscision like effect of injecting solution that is responsible for treatment response in acne scars. The growth factors in PRP may have augmenting effect on normal ageing tissue, but when replaced by fibrosis, they may not have optimum effect. Since, this is the first study which objectively compares PRP with NS injections for treatment of atrophic acne scars, more extensive studies with a larger sample size and a longer follow up are required to further establish this evidence.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We thank Dr Kalpana Bhatt for conducting Ultrabiomicroscopic Sonography of patients at her diagnostic centre.
The part of this manuscript was presented as an Award Paper at ASCICON 2018, Daman
CTRI/2017/10/009991
REFERENCES
- Assessment of life quality index among patients with acne vulgaris in a suburban population. Indian J Dermatol. 2016;61:163-8.
- [Google Scholar]
- Platelet-rich plasma in dermatology: Boon or a bane? Indian J Dermatol Venereol Leprol. 2014;80:5-14.
- [Google Scholar]
- Treatment of thin endometrium with autologous platelet-rich plasma: A pilot study. JBRA Assist Reprod. 2017;21:54-6.
- [Google Scholar]
- Platelet-rich plasma and its utility in the treatment of acne scars: A systematic review. J Am Acad Dermatol. 2019;80:1730-45.
- [Google Scholar]
- Postacne scarring: A qualitative global scarring grading system. Dermatol Surg. 2006;32:1458-66.
- [Google Scholar]
- Classification of platelet concentrates (platelet-rich plasma-PRP, platelet-rich fibrin-PRF) for topical and infiltrative use in orthopedic and sports medicine: Current consensus, clinical implications and perspectives. Muscles Ligaments Tendons J. 2014;4:3-9.
- [Google Scholar]
- Platelet gel-released supernatant modulates the angiogenic capability of human endothelial cells. Blood Transfus. 2008; 6:12-7.
- [Google Scholar]
- Updated August 12, 2007. http://en.wikipedia.org/wiki/Fitzpatrick_scale
- Ultrasound image of the skin, apparatus and imaging basics. J Ultrason. 2013;13:212-21.
- [Google Scholar]
- Introduction of a novel therapeutic option for atrophic acne scars: Saline injection therapy. Glob Dermatol. 2015;2:225-7.
- [Google Scholar]
- The evidence behind the use of platelet-rich plasma (PRP) in scar management: A literature review. Scars Burn Heal. 2018;4:2059513118808773.
- [Google Scholar]
- Androgenetic alopecia: Pathogenesis and potential for therapy. Expert Rev Mol Med. 2002;4:1-11.
- [Google Scholar]
- Fibroblast heterogeneity: Implications for human disease. J Clin Invest. 2018;128:26-35.
- [Google Scholar]
- Skin tissue engineering: Wound healing based on stem-cell-based therapeutic strategies. Stem Cell Res Ther. 2019;10:111.
- [Google Scholar]
- Epidermal Growth Factor (EGF) and Platelet-Derived Growth Factor (PDGF) as tissue healing agents: Clarifying concerns about their possible role in malignant transformation and tumor progression. J Carcinogen Mutagen. 2011;2:1-14.
- [Google Scholar]
- Acne scars: Pathogenesis, classification and treatment. Dermatol Res Pract. 2010;2010:893080.
- [Google Scholar]






