Translate this page into:
Comparison of Local Flaps and Skin Grafts to Repair Cheek Skin Defects
Address for correspondence: Dr. Ali Ebrahimi, Department of Plastic Surgery, Trauma Research Center, Baqiyatallah University of Medical Sciences, PO Box - 1436614313, Tehran, Iran. E-mail: ae_49341@yahoo.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background and Objective:
Selecting the appropriate technique for surgical incisions, and reconstruction of facial defects after skin tumour excision has always been one of the surgeon's biggest concerns. The aim of this study is to compare the results between the local flap and skin graft to reconstruct cheek defects after basal cell carcinoma excision.
Patients and Methods:
In this retrospective study, 40 patients with skin defects resulting from skin tumour (Basal cell carcinoma) excision in cheek zones (16 sub-orbital, 18 bucco-mandibular and six auricular) were treated using local flap (n = 20) and skin graft (n = 20) from October 2010 to April 2012. All patients were followed up for 12 months, postoperatively. In addition, general assessments including complications, patient satisfaction, tissue co-ordination, skin colour and hospitalisation days were obtained.
Results:
Five patients had postoperative hyper-pigmentation complication in the skin graft group and none occurred in the local flap (P = 0.046). In the early postoperative period (2 weeks), mean scores in patient satisfaction, tissue co-ordination and skin colour were statistically significant increase in the local flaps (P < 0.001, P < 0.001, P < 0.001, respectively) and in the later postoperative period (12 months) only mean scores in skin colour significantly increased in the local flaps (P < 0.001). The mean postoperative length of hospitalisation days was 1.7 ± 0.4 days in the local flap group, and 3.63 ± 1.16 days in the skin graft group (P = 0.001).
Conclusion:
In the local flap group: Patient satisfaction, tissue co-ordination and skin colour were improved after 2 weeks. Also in 12-months follow up visits, skin colour was improved significantly and the hyperpigmentation was reduced. Generally, in this study the local flaps had better results in clinical outcomes and patient satisfaction. However, for each cheek defect the surgeon must choose the appropriate reconstruction strategy to avoid undesirable outcomes.
Keywords
Cheek reconstruction
local flap
skin grafts
tumours
basal cell carcinoma
BACKGROUND
Skin cancer is the most common malignancy occurring in humans.[1] The most common malignant tumours of the face are basal cell carcinoma (BCC), squamous cell carcinoma (SCC), and melanoma.[2345] BCC is the commonest skin cancer.[6] Current treatment modalities for skin cancers and premalignant lesions include surgical excision, electrocautery, curettage, cryotherapy, and irradiation, but surgical excision has been reported to be the best treatment modality for cancer treatment and preventing recurrence.[7] Cutaneous carcinomas of the cheek may involve the epidermis, dermis and, subcutaneous tissues that overlie the superficial musculo-aponeurotic system (SMAS) and can also involve deeper structure of the face.[89] There are several reconstruction options after excision of skin tumours in this region of the face including primary repair, skin graft, local flap, regional flaps, distant and free flaps. The choice of reconstructive procedure is dependent upon several factors, including size, location, involvement of deeper structures, etc. Primary repair is used in small defects less than 2 cm when there is no tension on the edges of the defect. Depending on the donor site and the needs of the patient graft can be split-thickness or full-thickness. A split-thickness skin graft contains epidermis and a variable amount of dermis.[10] A full-thickness skin graft includes all of the dermis as well as the epidermis.[10] In skin grafts, the aesthetic outcome can be poor due to colour and texture mismatch of the transplanted skin. Flaps are classically categorised based on their vascular supply, composition, method of transfer and design.[1112] Proper execution of facial reconstruction also relies on appropriate analysis and characterisation of the defect.[12] Local flaps for cheek reconstruction including Rhomberg transposition flap, advancement flap, rotation- advancement flap (Mustarde flap) and v-y advancement (kite flap).[13] Due to the unique characteristics of the cheek subunit, few complex local flap designs can be used to reconstruct the vast majority of defects.[913] For larger cheek defects (>6 cm), we need some type of regional or distant flap.[13] Free flaps are applicable for complex soft tissue and bone defects or through and through defects.[13] The surgeon should choose the simplest type that can achieve the desired effect. With all surgical procedures, complications can occur on reconstruction in the facial areas. Dehiscence generally occurs within the first 2 weeks after surgery. Complications that appear at a later stage usually involve the aesthetic outcome. Typical aesthetic deficits consist of the trapdoor or bulkiness phenomenon for local flaps and colour mismatch between the reconstructed area and the neighbouring skin or atrophy and shriveling of the graft with secondary distortion of the surrounding soft tissue for full-thickness skin graft.[141516]
OBJECTIVE
Selecting the appropriate technique for surgical incisions, and reconstruction of facial defects after skin tumour excision have always been one of the surgeon's biggest concerns. The aim of this study is to compare the results between the local flap and full thickness skin graft for reconstruction of the defect after excision of skin tumours on the cheek.
PATIENTS AND METHODS
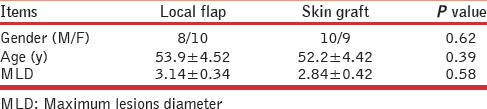
A retrospective review of all patients (n = 40) who presented with skin defects resulting from skin tumour (BCC) excision in cheek zones [Figure 1] (16 sub-orbital, 18 bucco-mandibular and 6 pre-auricular) were reconstructed using local Flap [Figure 2] (n = 20) and skin graft [Figure 3] (n = 20) between October 2010 and April 2012.
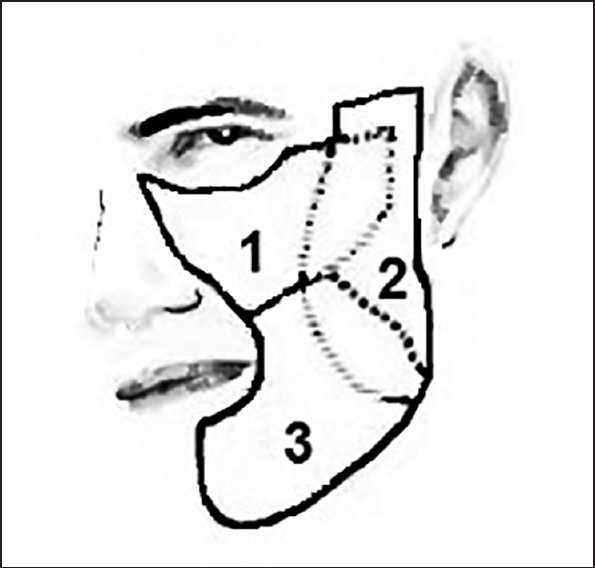
- Aesthetic cheek zones according to Mathez textbook of plastic surgery: 1) Sub-orbital, 2) Pre-uricular and 3) Bucco-mandibular. Areas with dotted lines are overlapped zones between two zones
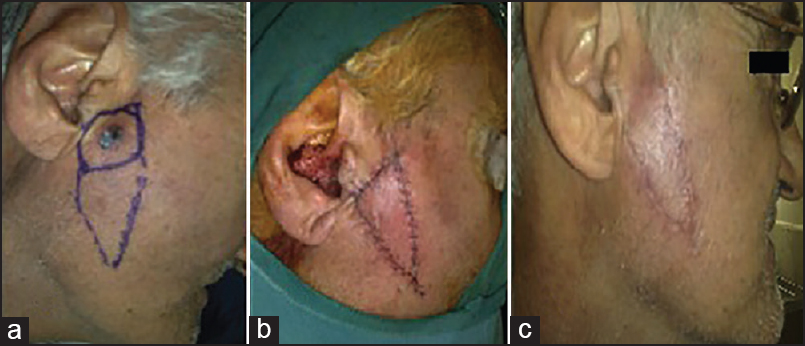
- (a) A man with a basal cell carcinoma in the Pre-auricular zone of the cheek and design of the kite flap (b) Closure of the defect with no distortion of the surrounding structures after operation (c) Six months postoperatively

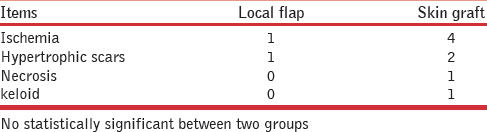
- Longterm aesthetic results of skin graft and local flaps in two middle age women with a basal cell carcinoma in the Sub-orbital zone of the cheek (left) and buccomandibular zone (right)
The present study was conducted at the department of plastic surgery in Baqiyatallah University of medical sciences, Tehran, Iran. This study was approved by the ethical committee of our University. Patients with a history of taking certain medications such as corticosteroids or chemotherapy and the presence of comorbidities such as diabetes, lupus erythematous or scleroderma, those who withdrew from follow-up and patients with defect >6 cm were excluded from the study. We usually performed wide local excision in our facial tumours, in rare cases we did Mohs surgery. Local flap reconstruction included (six Rhomberg transposition flaps, four rotation- advancement flaps (Mustarde flap) and ten v-y advancement (kite flaps)), Skin graft surgery included (12 full-thickness skin graft and eight thick split-thickness skin graft) harvested from post auricular and medial arm respectively. All patients were followed up for 12 months postoperatively. Three patients were lost for follow-up (two patients of local flap and one of skin graft). The study was conducted on patients of a single surgeon and all postoperative examinations were performed in plastic surgery clinic by a surgeon other than the primary surgeon, but for reasons of patient satisfaction, the primary surgeon saw the patient on every visit as well. In addition, general assessments including complications (hypopigmentation, hyperpigmentation, infection, ischaemia, necrosis, keloids and hypertrophic scars), patient satisfaction, tissue co-ordination, skin colour and hospitalisation days were obtained. Assessment of satisfaction, tissue coordination and skin colour were done using a scale ranging from 0 to 10 (0 = no satisfaction, 1-4 = mild satisfaction, 5-7 = moderate satisfaction, 8-9 = satisfaction, 10 = extreme satisfaction).
Preoperative, intra-operative and postoperative photography was performed in all patients and the results were compared between the two groups in terms of skin colour and texture. All data were checked for a normal distribution using the Kolmogorov-Smirnov test. Quantitative variables were compared between groups using the Student's t-test or Mann-Whitney U-test, depending on whether normal or non-normally distributed variables were used, respectively. For qualitative data, Chi-square test and in the absence of circumstances Fisher's exact test was used. Data were analyzed using SPSS 20 software (SPSS, Chicago, IL, USA). A P-value less than 0.05 was considered statistically significant.
RESULTS
Forty patients were included in this study; (20 patients in local flap group and 20 with the skin graft group) [Figures 2 and 3]. The mean age of the patients was 53.02 ± 4.2 years. The mean maximum lesions diameter of the patients was 2.93 ± 0.24 cm. There was statistically no significant difference between the two patient groups in respect to gender, age and maximum lesions diameter [Table 1]. There was no case with complications (hypopigmentation, hyperpigmentation and infection) in two groups after 2 weeks and no case was observed with hypopigmentation in two groups after 12 months of follow-up. Five patients had postoperative hyperpigmentation in the skin graft group and none occurred in the local flap group and there was statistically significant difference between the two patient groups (P = 0.046). Also, there was no significant difference between the two patient groups in respect to complications (ischaemia, hypertrophic scars, necrosis and keloid) [Table 2].
In the early postoperative follow-up visit (2 weeks), mean scores in patient satisfaction, tissue coordination and skin colour were comparable in the two groups and there was statistically significant difference between the two patient groups (P < 0.001, P < 0.001, P < 0.001, respectively) [Figure 4].
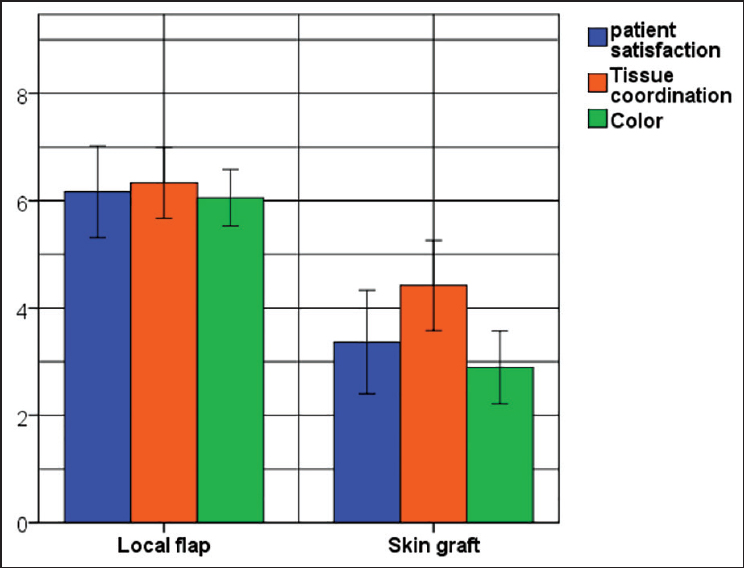
- Means ± SD score for evaluated patient satisfaction, tissue coordination and color two weeks after operation. The results were 6.2 ± 1.7 vs. 3.4 ± 2.0, 6.3 ± 1.3 vs. 4.4 ± 1.7, 6.1 ± 1.6 vs. 2.9 ± 2.0 for local flap vs. skin graft, respectively (P < 0.001, P < 0.001, P < 0.001).
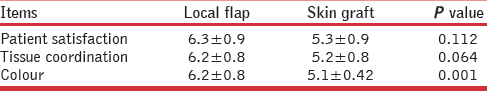
In the later postoperative follow-up visit (12 months), mean scores in patient satisfaction, tissue coordination and skin colour were comparable in the two groups (P = 0.112, P < 0.064, P < 0.001, respectively) [Table 3]. Also, there were significant correlation between the patient satisfaction, tissue coordination and skin colour in 2 weeks and 12-months follow-up (0.55, 0.52 and 0.57, P < 0.001, P < 0.001 and P < 0.001, respectively).
The mean postoperative length of hospital stay was 1.7 ± 0.4 days in the local flap group and 3.63 ± 1.16 days in the skin graft group. There was significant difference between the groups with respect to length of hospital stay (P = 0.001). We had no recurrence of tumour during follow-up and in all patients safe margins were confirmed by frozen section intraoperative and permanent pathologic report postoperatively.
DISCUSSION
The reconstruction of skin and soft tissue defects of the cheek can be challenging.[9] There are several reconstructive options after excision of skin tumours of the cheek, including primary repair, skin grafts, different local flaps, regional flaps, distant and free flaps. The choice of reconstructive procedure is dependent upon several factors, including size, location, involvement of deeper structures, etc.[13] In the present study we assessed patients with cheek defects resulting from skin tumour (BCC) excision that were treated with local flap or skin graft. Patient satisfaction, tissue co-ordination and skin colour were significantly higher in local flap group. In postoperative follow-up patient satisfaction and tissue coordination were similar in both groups, but skin colour was improved in the local flap group. Skin grafting was used successfully in reconstructing defects situated in concavities and over a bony foundation, which provides the underlying structure critical to the flap and prevents excessive contraction.[9] Another study showed that skin grafting was one of the most useful reconstructive modalities for skin and subcutaneous tissue defects; however, postoperative scars were sometimes a determining factor of patient satisfaction; in particular, the colour match between the grafted skin and surrounding recipient skin was important.[17] Split-thickness skin grafting is widely used for primary wound coverage after skin cancer resection or relatively extensive skin defect coverage, such as extensive burns; because donor-site morbidity is lower and wider skin grafts are available.[18] Particular attention should be given when skin graft is considered for defect closure adjacent to eye lid, nasal margin, or oral commissure due to concern of skin graft contraction.[3] In the present study we didn’t have any complications (hypopigmentation, hyperpigmentation and infection) in the two groups at two weeks. Another study reported that when the size of the defect was smaller than 4 cm; flaps can make efficient coverage with fewer complications.[19] In our study hyperpigmentation in the skin graft group was significantly higher compared to local flap group. The ideal facial reconstruction should provide a good colour and texture harmony with adjacent tissues. Optimal aesthetic reconstruction of facial defects is dependent on the availability of donor sites with similar colour, texture, sebaceous quality, and thickness to the defect tissues. We explain advantage and disadvantage of both flaps and grafts to our patients but most of them have more inclination to flap coverage in facial cheek reconstructions due to better cosmetic outcome and second ary morbidity due to harvesting of the graft at the donor site. A great number of local flaps, pedicled flaps and micro-vascular free flaps have been employed over the years for the reconstruction of mid-facial defects.[13] Nevertheless, reconstruction of the mid-face remains a challenging and still varied problem due to the different defects and the complex three-dimensionality of the region.[20]
CONCLUSION
In this study local flaps had better results in clinical outcomes and patient satisfaction as compared to grafts. However, for each cheek defect the surgeon must choose the appropriate reconstruction strategy to avoid undesirable outcomes. We recommend local flap reconstruction in on the cheek that are skin defects less than 6 cm and where there is no fear of recurrence of the tumour.
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- Cutaneous malignancies and their management. Otolaryngol Clin North Am. 2001;34:523-53.
- [Google Scholar]
- Bipedal myocutaneous flap for one-stage reconstruction of the cheek after cancer surgery. J Laryngol Otol. 1988;102:601-2.
- [Google Scholar]
- Cheek reconstruction: Current concepts in managing facial soft tissue loss. Semin Plast Surg. 2008;22:294-305.
- [Google Scholar]
- Use of a folded forehead flap for reconstruction after a large excision of the full thickness of the cheek. Plast Reconstr Surg. 1975;56:629-32.
- [Google Scholar]
- Uses of the trapezius and sternomastoid myocutaneous flaps in head and neck reconstruction. Plast Reconstr Surg. 1979;63:49-57.
- [Google Scholar]
- Usefulness of v-y advancement flap for defects after skin tumour excision. Arch Plast Surg. 2012;39:619-25.
- [Google Scholar]
- Complex local flap design in cheek reconstruction. Oper Tech Otolaryngol Head Neck Surg. 2011;22:53-8.
- [Google Scholar]
- Concepts in local flap design and classification. Oper Tech Otolaryngol Head Neck Surg. 2011;22:13-23.
- [Google Scholar]
- Applications of kite flap in reconstruction of cheek defects after tumour excision. MJMS. 2012;5:313-6.
- [Google Scholar]
- The bilobed flap: A very efficient method in aesthetic reconstruction of small skin defects at the alar and tip regions of the nose. Ann Chir Plast Esthet. 2003;48:211-5.
- [Google Scholar]
- Aesthetic reconstruction of nasal defects using forehead flaps. Facial Plast Surg. 1997;13:111-7.
- [Google Scholar]
- Prefabricated nasolabial flap for reconstruction of full-thickness distal nasal defects. Dermatol Surg. 2005;31:546-52.
- [Google Scholar]
- Repair and Reconstruction in the Orbital Region: A Practical Guide. (3rd ed). London: Churchill Livingstone; 1991.
- [Google Scholar]
- Temporalis myofascial flap in maxillary reconstruction: Anatomical study and clinical application. J Craniomaxillofac Surg. 2009;37:96-101.
- [Google Scholar]






