Translate this page into:
Efficacy and safety of microneedling radiofrequency in patterned hair loss
*Corresponding author: Balakrishnan Nirmal, MD Consultant Dermatologist and Head, Dermal Square skin hair nail clinic, Madurai, India. nimu2swash@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Nirmal B, Shahin Mubeena S, Antonisamy B. Efficacy and safety of microneedling radiofrequency in patterned hair loss. J Cutan Aesthet Surg. 2024;17:189-93. doi: 10.25259/jcas_44_23
Abstract
Objectives:
We aimed to assess the improvement of patterned hair loss with microneedling radiofrequency (MNRF) and its adverse effects in patients.
Material and Methods:
An open-label study was conducted to evaluate the efficacy and safety of MNRF for the treatment of androgenetic alopecia. Patients diagnosed with patterned hair loss received three MNRF treatment sessions once monthly. Efficacy was assessed by comparing before and after photographs and trichoscopy.
Results:
Twenty-four patients were recruited. Excellent improvement in hair growth was observed in 14 patients, fair improvement in seven patients, and no improvement in three patients without significant adverse effects. Slight pain lasting for a day was the most common adverse event following MNRF.
Conclusion:
Overall, significant improvement was observed in the majority of the patients without significant side effects.
Keywords
Microneedling radiofrequency
Patterned hair loss
Alopecia
INTRODUCTION
Patterned hair loss is a common disorder of hair loss affecting both sexes characterized by miniaturization of hair follicles causing the transformation of terminal to vellus hairs resulting in patterned hair loss.1 The disorder is not only a cosmetic concern but it also causes impairment of the quality of life of patients resulting in anxiety, depression, or even suicide.2 Minoxidil and finasteride are the only US Food and Drug Administration (FDA)-approved medications for the treatment of patterned hair loss that constitute the backbone of therapy.3 Other non-surgical therapies for patterned hair loss include dutasteride, spironolactone, platelet-rich plasma, microneedling, and low-level laser therapy.4-6
Microneedling, a concept introduced in 1995 by Orentreich, is a technique consisting of repeated puncturing of skin using sterile microneedles. Microneedling is proposed to improve hair growth through the release of growth factors.7 Newer modalities combine mechanical puncturing of microneedling with fractional radiofrequency resulting in the release of energy from tips of microneedles called microneedling radiofrequency (MNRF). MNRF induces wound healing mechanisms through thermal damage. Following wounding, the stem cell population expresses molecular markers of follicle differentiation and activates the Wnt/β-catenin pathway resulting in hair growth.8 Energy-based devices have gained popularity due to limited non-invasive alternative therapeutic options available in the management of patterned hair loss.
MATERIAL AND METHODS
Aim and objectives
Our aim and objectives were to assess the efficacy of MNRF in the treatment of patterned hair loss concerning age, sex, and stage of hair loss. We also aimed to look at the most common adverse effects following the therapy.
Study design
The study was designed as a prospective study using MNRF for the treatment of patterned hair loss in 24 patients from January 2021 to May 2022. Patients attending the dermatology outpatient department with a clinical diagnosis of patterned hair loss above 18 years and willing to participate in the study were included in the study. Pregnant ladies and lactating mothers were excluded from the study. Patients with concomitant scalp inflammatory disorders such as psoriasis and folliculitis were deferred from the procedure.
Ethical considerations
A written and signed informed explanatory consent was taken from all the patients before initiation of therapy.
Treatment protocol
Patients received 3 MNRF treatment sessions at once monthly intervals. A eutectic mixture of local anesthetic cream (25 mg prilocaine and 25 mg lidocaine) was applied topically to the scalp under occlusion for 60 min before the procedure. MNRF (Dermaindia, India) was delivered using a disposable tip containing 81 non-insulated microneedle electrodes, power of 2–6 W, microneedle penetrating depth of 1.5 mm, and pulse duration of 300 ms.
Efficacy evaluation
Global assessment
Photographs were taken under controlled light by the same investigator (NB) in the same position. Two investigators (NB, SM) performed the clinical assessment based on the photographs taken at baseline and 1 month after 3rd session.
Trichoscopic assessment
Trichoscopic images (Escope, India) were taken at baseline, and 1 month after the last session at the same scalp location (15 cm from the glabella), and then the images were compared [Figure 1].
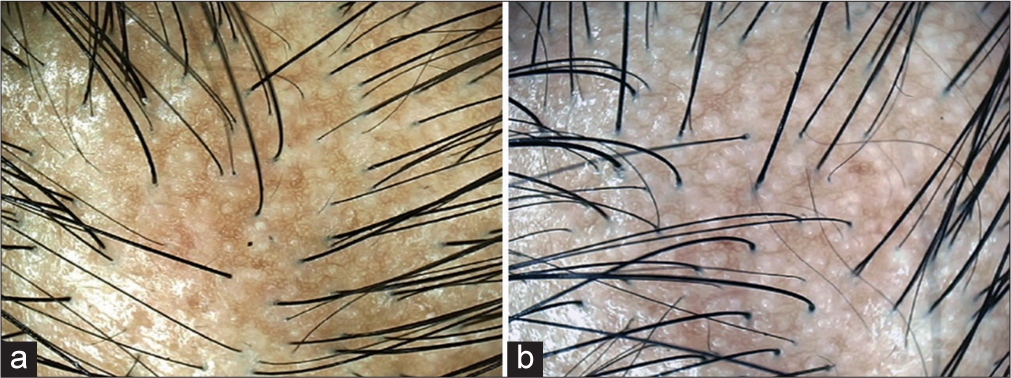
- Trichoscopic evaluation (Escope, India ×100). (a) Before treatment. (b) After treatment showing fair improvement (+1).
The assessment was measured on a seven-point scale and graded as follows:
Excellent improvement (+3)
Good improvement (+2)
Fair improvement (+1)
No change (0)
Slightly worsened (−1)
Moderately worsened (−2)
Significantly worsened (−3).
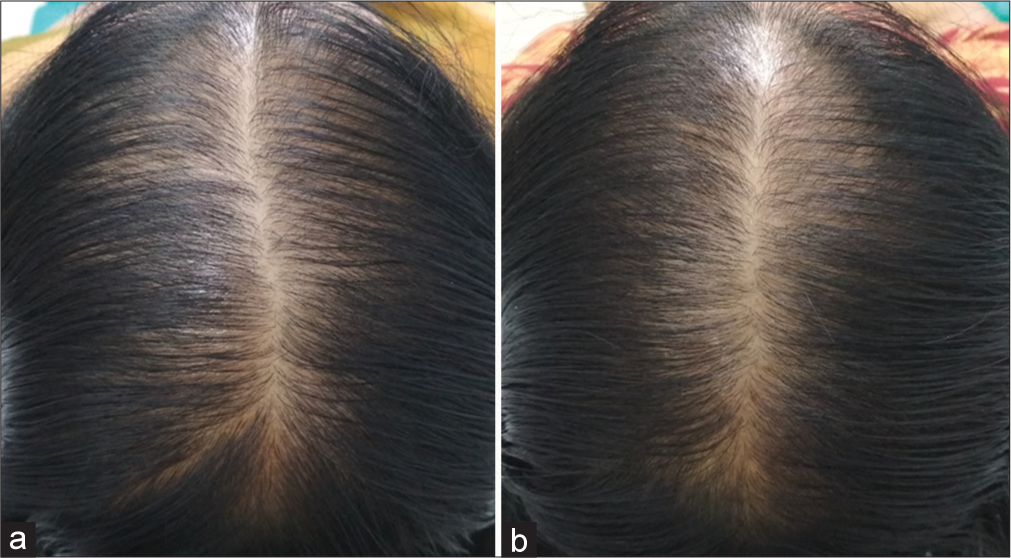
Participants were also asked to give their assessment of the procedure using the same seven-point scale 1 month after the last session [Figures 2-6]
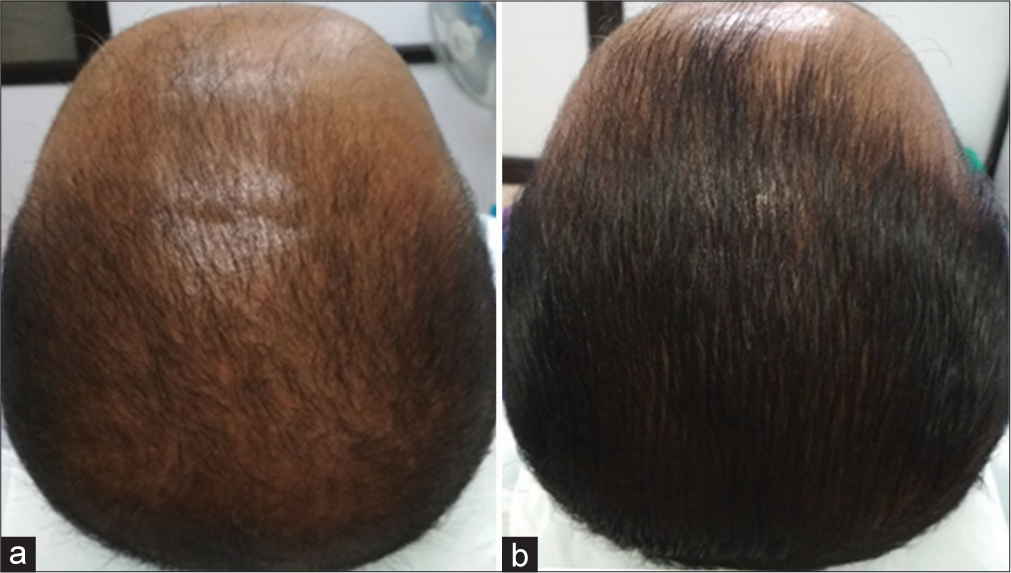
- Excellent improvement (+3). (a) Before treatment. (b) After treatment.
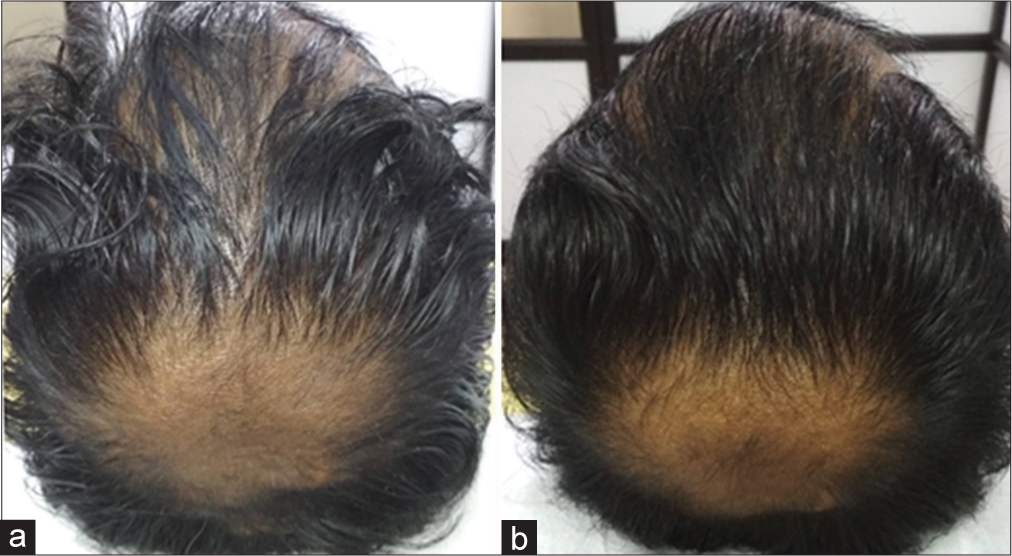
- Good improvement (+2). (a) Before treatment. (b) After treatment.
- Fair improvement (+1). (a) Before treatment. (b) After treatment.
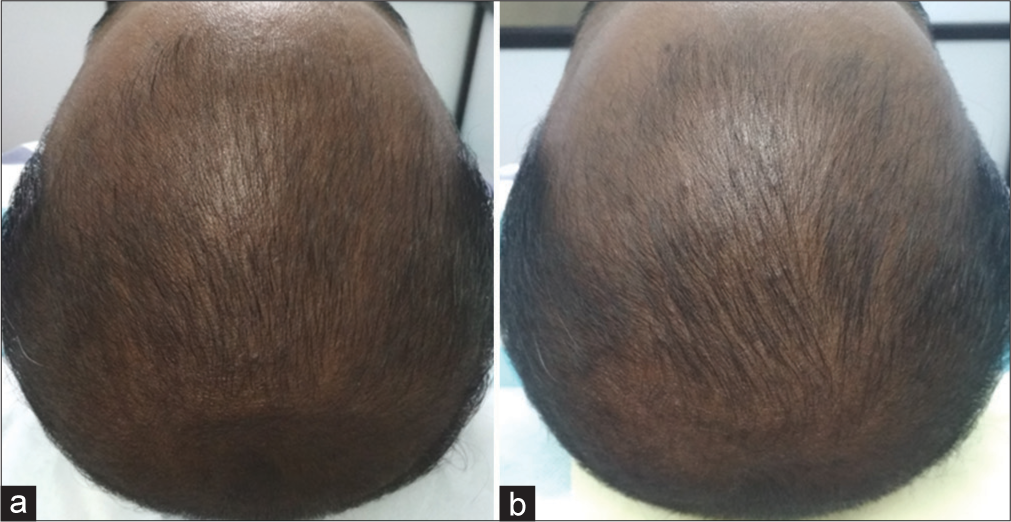
- No change (0). (a) Before treatment. (b) After treatment.

- Slight Worsening (−1). (a) Before treatment. (b) After treatment.
Safety assessment
Patients were instructed to report any adverse events including bleeding, persistent pain, erythema, erosion, crusting, scaling, folliculitis and broken hair shafts following thermal damage. Patients were also asked to rate pain according to a visual analog pain scale (0 meaning no pain and 10 meaning the most severe pain).
Statistical analysis
Data were summarized as mean and standard deviation or median and range depending on the distribution of variables. Spearman rank correlation (rho) was performed between age and patient satisfaction score on improvement. A Chi-square test was performed to test the association between sex and alopecia grade with patient satisfaction score on improvement. Weighted-Kappa statistics were used to determine the interobserver agreement between investigators (1 and 2) and between investigators and patient satisfaction scoring. P < 0.05 was considered statistically significant. Statistical analysis was performed using STATA/IC 16.0 (StataCorp, College Station, Texas 77845, USA).
RESULTS
Patient demographics
The median age of patients was 26.5 years (range 21–58) and 22 males and 2 females participated in the study [Table 1].
| Age |
|---|
| Median=26.5 years (range 21–58) |
| Sex |
| Males=22 |
| Females=2 |
| Grade of alopecia |
| Hamilton–Norwood scale for males (n=22) |
| Type III=3 |
| Type IV=9 |
| Type V=7 |
| Type VI=2 |
| Type VII=1 |
| Ludwig scale for females (n=2) |
| Type II=1 |
| Type III=1 |
The number of patients in each grade of alopecia includes Hamilton–Norwood scale Type III (n = 3), Type IV (n = 9), Type V (n = 7), Type VI (n = 2), Type VII (n = 1), Ludwig scale Type II (n = 1), and Type III (n = 1).
Comparison of patient satisfaction and inter-observer variation
There was excellent/good improvement in 14 patients, fair improvement in seven patients, and no improvement/slight worsening in three patients. Global photographs showed clinical improvement in most participants, with hair regrowth in 91.67% (22/24) of participants [Table 2].
| Grading of improvement | Investigator 1 | Investigator 2 | Patient self-assessment |
|---|---|---|---|
| Excellent improvement (+3) | 2 | 3 | 2 |
| Good improvement (+2) | 13 | 12 | 12 |
| Fair improvement (+1) | 7 | 5 | 7 |
| No change (0) | 0 | 3 | 3 |
| Slight worsening (−1) | 2 | 1 | 0 |
| Moderate worsening (−2) | 0 | 0 | 0 |
| Significant worsening (−3) | 0 | 0 | 0 |
Kappa statistics was used to monitor the agreement between observers 1 and 2, patient and observer-1, and patient and observer-2. Weighted kappa scores between these three categories were 93.8%, 93.8%, and 89.6%, respectively, showing good agreement between them [Table 3].
| Comparison | Kappa analysis (%) |
|---|---|
| Investigator 1 versus Investigator 2 | 93.8 |
| Investigator 1 versus patient | 93.8 |
| Investigator 2 versus patient | 89.6 |
Evaluation of improvement with respect to age, sex and alopecia grade.
There was no significant difference between age (P = 0.8771), sex (P = 0.909), and grade of alopecia (P = 0.895) with clinical improvement.
Adverse effects
Slight pain (average pain score 3) lasting for a day was the commonest adverse event following MNRF. One patient reported folliculitis and one reported scaling and dryness following treatment.
DISCUSSION
MNRF produces its effects through dual mechanisms including mechanical wounding by microneedling and thermal injury by radiofrequency.8 Following wounding, hair follicles express molecular markers of follicle differentiation through Wnt/β-catenin pathway activation. Cytokines (interleukins and tumor necrosis factor-α) and inflammatory cells (macrophages) have an important role in the process. Microneedling causes upregulation of hair growth-related genes.9 Moderate transient inflammation produces induction of the anagen phase. Wounding following thermal injury triggers the regeneration of hair follicles. MNRF causes inflammation resulting in increased blood flow and follicular vascularization. Radiofrequency released by MNRF results in the vibration of polar molecules and converts vibrating energy to thermal energy creating thermal zone columns . Fractional thermolysis and microchannels induced by MNRF facilitate the transdermal delivery of topicals through the creation of holes in the stratum corneum. In addition, MNRF can have a direct impact on bulge stem cells and dermal papilla.
Yu et al. reported combining MNRF with minoxidil to be more effective in terms of hair thickness, hair density, and slowing the progression of androgenetic alopecia in 19 patients attributed to direct effects of MNRF and increased efficacy of minoxidil as a result of enhanced penetration through thermal channels created by needles.8 Lim et al. observed a significant increase in hair density, hair thickness, and hair count following MNRF in 19 out of 20 patients included in the study.10
These results were in line with our study where 22 out of 24 patients (91.67%) of patients showed improvement following therapy. However, caution should be exerted not to damage the follicular and perifollicular structures using higher fluence, especially with non-insulated needles. The grading of improvement in our study was not significant with age, sex, and severity of alopecia suggesting that the improvement is independent of these variables.
CONCLUSION
Good-excellent improvement was observed in the majority of the patients without significant side effects. Limitations of the study include not having a control group and a relatively small sample size. Future studies can be undertaken combining MNRF with platelet-rich plasma and growth factor concentrate as results can be mutually additive. The part of the scalp exhibiting maximum improvement with the procedure can also be evaluated in further studies. Thus, MNRF could potentially provide an effective and safe addition to the therapeutic armamentarium of patterned hair loss.
Authors’ Contributions
Nirmal B: Study conception and design, data collection, analysis and interpretation of results, manuscript preparation. S Shahin Mubeena: Analysis and interpretation of results. Belavendra Antonisamy: Analysis and interpretation of results, statistical analysis.
Ethical approval
The research/study complied with the Helsinki Declaration of 1964.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Androgenetic alopecia: An update. Indian J Dermatol Venereol Leprol. 2013;79:613-25.
- [CrossRef] [PubMed] [Google Scholar]
- Male pattern androgenetic alopecia in an Indian context: A perspective study. J Eur Acad Dermatol Venereol. 2007;21:473-9.
- [CrossRef] [PubMed] [Google Scholar]
- A review of the treatment of male pattern hair loss. Expert Opin Pharmacother. 2020;21:603-12.
- [CrossRef] [PubMed] [Google Scholar]
- The effectiveness of treatments for androgenetic alopecia: A systematic review and meta-analysis. J Am Acad Dermatol. 2017;77:136-41.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment options for androgenetic alopecia: Efficacy, side effects, compliance, financial considerations, and ethics. J Cosmet Dermatol. 2021;20:3759-81.
- [CrossRef] [PubMed] [Google Scholar]
- Evidence-based (S3) guideline for the treatment of androgenetic alopecia in women and in men-short version. J Eur Acad Dermatol Venereol. 2018;32:11-22.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy and safety of scalp microneedling in male pattern hair loss. Skin Appendage Disord. 2023;9:18-26.
- [CrossRef] [PubMed] [Google Scholar]
- A pilot split-scalp study of combined fractional radiofrequency microneedling and 5% topical minoxidil in treating male pattern hair loss. Clin Exp Dermatol. 2018;43:775-81.
- [CrossRef] [PubMed] [Google Scholar]
- A randomized evaluator blinded study of effect of microneedling in androgenetic alopecia: A pilot study. Int J Trichology. 2013;5:6-11.
- [CrossRef] [PubMed] [Google Scholar]
- Nonablative radiofrequency for the treatment of androgenetic alopecia: An open-label study. Dermatol Rev. 2021;2:1-3.
- [CrossRef] [Google Scholar]







