Translate this page into:
Efficacy of Topical 5% 5-Fluorouracil with Needling versus 5% 5-Fluorouracil Alone in Stable Vitiligo: A Randomized Controlled Study
Address for correspondence: Dr. Mohammad Adil, B-9, Rizvi Apartments, Medical Road, Aligarh 202002, Uttar Pradesh, India. E-mail: dr.mohd.adil@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
Vitiligo is a chronic disease of great cosmetic concern presenting with depigmented macules and patches. It is often recalcitrant to medical treatment.
Aim:
The aim of the study was to study the efficacy and safety of topical 5% 5-fluorouracil with needling versus topical 5% 5-fluorouracil alone in stable vitiligo.
Materials and Methods:
This interventional prospective study was conducted from July 2018 to June 2019. Total of 60 patients, with stable vitiligo of age older than 10 years, were randomly assigned into two groups of 30 patients each. Group A was treated with needling followed by topical 5% 5-fluorouracil over vitiligo patches. The procedure was performed every 2 weeks for 3 months. Group B was treated with topical 5% 5-fluorouracil alone. Clinical improvement was assessed monthly till 6 months by serial clinical photographs and grading score.
Results:
Initiation of repigmentation started at 1 month in 76 patches (65%) in Group A, whereas in group B, it was seen in 45 patches (38.7%), which was statistically significant (P = 0.0001). Excellent improvement (>75% repigmentation) was noted in 55 patches (47%) in Group A as compared to 5 patches (4.3%) in group B at the end of 6 months (P = 0.03).
Conclusion:
Needling with 5% 5-fluorouracil appears to be simple, safe, and effective treatment in vitiligo. It can be used in poor responders to conventional therapy.
Keywords
5-Fluoroucil
needling
therapeutic wounding
vitiligo
INTRODUCTION
Vitiligo is a commonly acquired, idiopathic, heritable depigmentary disorder of skin and/or mucous membrane. It is a chronic disease of great social and cosmetic concern. The prevalence of vitiligo in India varies from 0.1% to 8.8%.[1] The diagnosis of vitiligo is usually clinical. It is characterized by depigmented macules due to the selective destruction of melanocytes.[2] Several factors have been proposed for the disease such as autoimmune hypothesis, oxidative stress theory, genetic factors, autocytotoxicity, neurohumoral hypothesis, and melanocytorrhagy.[3] As it is often recalcitrant to medical treatment alone, many surgical techniques and modifications have been used to treat stable recalcitrant vitiligo ever since 1964.[4] Stability of vitiligo has been defined by various authors as the duration varying from 6 months to 2 years during which there is no new lesion, no enlargement of the existing lesion, and no Koebnerization.[567]
Though a lot of surgical treatment modalities are available for vitiligo, patients are often apprehensive to undergo extensive procedure such as grafting. Therapeutic wounding of lesion helps in stimulation of melanocytes of the surrounding area and hair follicles to migrate, proliferate, and repigment the skin.[5] Needling followed by topical application of 5% 5-fluorouracil (5-FU), a combination of medical and surgical modalities, provides a promising, effective, and safe modality of treatment.
The aim of this study was to assess the efficacy and safety of topical 5% 5-FU with needling versus 5% 5-FU alone in stable vitiligo.
MATERIALS AND METHODS
Study design
This was a hospital-based interventional comparative study conducted in outpatient department of dermatology over a period of 1 year from July 2018 to June 2019. Clearance for the study was obtained from the institutional ethics committee.
Sample size
Sample size was calculated using the Sealed Envelope power calculator for binary outcome superiority trial. On the basis of previous studies,[8] this was obtained considering 48% percentage success in experimental group and 12% success in control group, at significance level of 5% and power 90%. The sample size thus calculated was 29 in each group.
Study subjects
A total of 60 patients with vitiligo attending the outpatient department of dermatology during the study period, who satisfied the following criteria, were enrolled in the study: age older than 10 years and stability of lesions for a duration of at least 1 year. Patients with vitiligo patches on mucous membrane, Koebner phenomenon, keloid or hypertrophic scar tendency, and other uncontrolled systemic illnesses were excluded from the study. They were asked about the duration of disease, total number of patches, presence of white hair, and prior treatments taken. Informed written consent was obtained from each patient.
Study intervention
Patients were randomly assigned into two groups of 30 patients each using “chit in the box” method. Group A (117 patches) received treatment with 5% 5-FU along with needling, whereas patients in Group B (116 patches) were treated only with topical 5% 5-FU.
In group A, topical lignocaine spray was applied on the patch 20 min before the procedure. The affected area was cleaned and sterilized using betadine solution. A thick paste of 5% 5-FU cream was applied on the patch. This was followed by microneedling with 26-gauge needle with punctures made as close as possible to each other. This resulted in pinpoint bleeding points, which was wiped using betadine gauze. Mixture of 5% 5-FU and topical antibiotic cream (1:1 ratio) was applied on the treated area and dressed for 2 days. Patients were advised to apply the mixture of 5-FU and antibiotic cream twice daily for the next 13 days. Maximum of six sessions of therapy was done at 2-week interval.
Group B patients were advised for twice daily application of 5% 5-FU cream only.
Follow-up
Patients were followed for 3 months after the last session. Assessment was done at baseline and thereafter every month using clinical photographs and by subjective assessment score of repigmentation [Table 1]. A CONSORT flowchart showing participant status through the trial is given in Figure 1.
| Repigmentation | Grade | Response |
|---|---|---|
| Absent | G0 | No response |
| <25% | G1 | Poor |
| 25%–50% | G2 | Good |
| 50%–75% | G3 | Very good |
| >75% | G4 | Excellent |
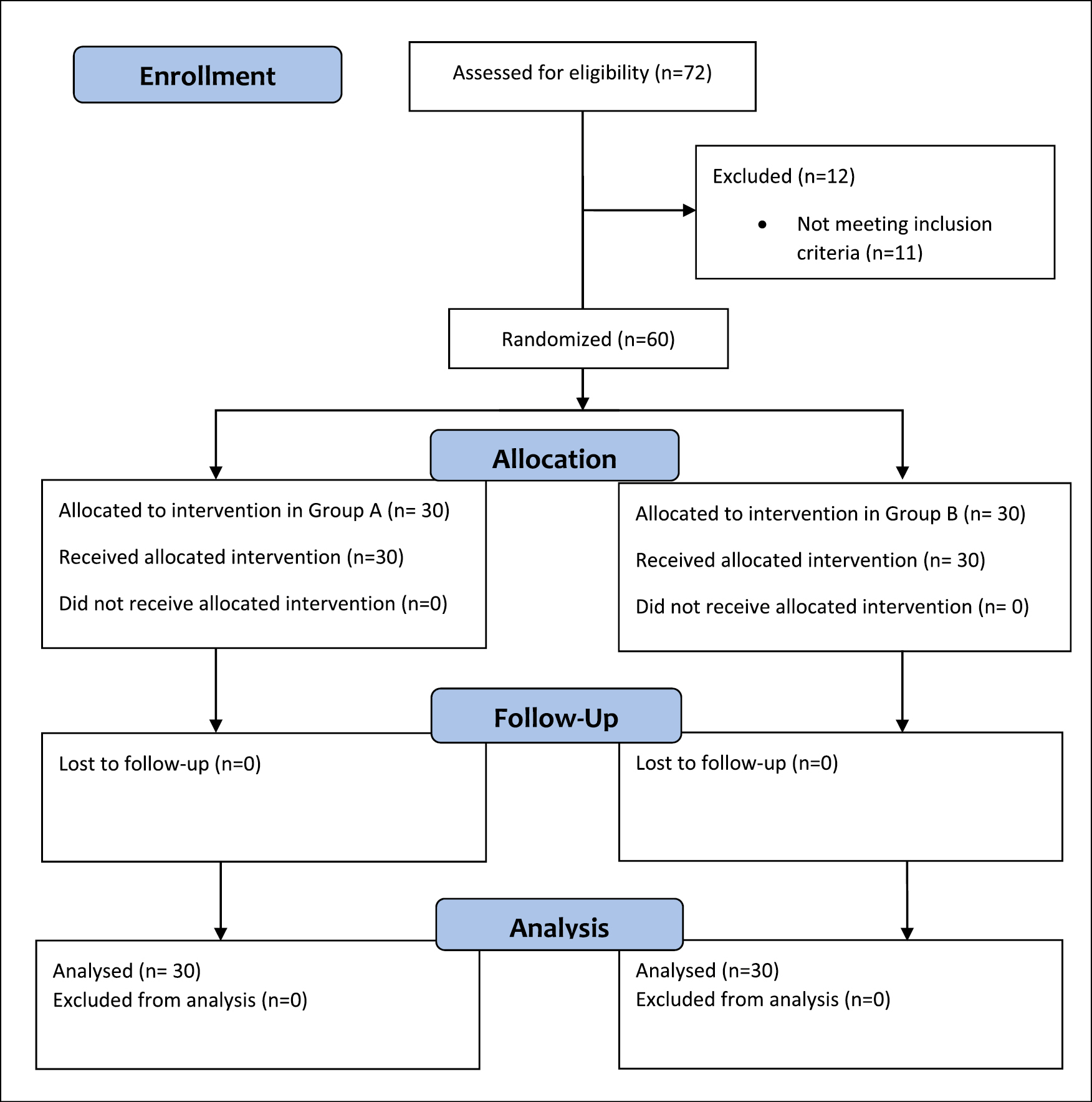
- CONSORT flowchart showing participant status through the trial
Statistical analysis
Data were statistically analyzed using the Statistical Package for Social Sciences (SPSS) software, version 25.0 (IBM Corp., Armonk, New York, USA). The parameters of mean, standard deviation, frequencies, range, ratio, or percentages were used for analyzing descriptive statistics. Both t test and chi-square test were used for analytical statistics as needed, and P ≤ 0.05 was considered as significant. The primary efficacy was analyzed for grades of repigmentation in the vitiligo patches at the end of 6 months. Assessment was also done for the response of treatments at different body sites.
RESULTS
Both Group A and Group B patients were comparable in terms of age (P = 0.06) and sex distribution (P = 0.791). The mean age in Group A and Group B was 29.4 and 24.2 years, respectively. We found vitiligo to be more prevalent in females comprising 18 (60%) patients in Group A and 19 (63.3%) patients in Group B. The mean duration of vitiligo was 7.25 years in Group A and 5.90 years in Group B. The most common morphological type in our study was vitiligo vulgaris (37 of 60, 61.7%) followed by focal vitiligo (12 of 60, 20%). More details regarding the clinical characteristics of both the groups are mentioned in Table 2.
| Clinical data | Group A | Group B | P value |
|---|---|---|---|
| Age (mean ± SD) years | 29.4 ± 10.52 | 24.2 ± 10.17 | 0.06 |
| Gender | |||
| Male | 12 (40%) | 11 (36.7%) | 0.791 |
| Female | 18 (60%) | 19 (63.3%) | |
| Duration (mean ± SD) years | 7.25 ± 6.35 | 5.90 ± 3.80 | 0.323 |
| Type of vitiligo | |||
| Vulgaris | 18 (60%) | 19 (63%) | 0.971 |
| Focal | 7 (23%) | 5 (17%) | |
| Segmental | 2 (7%) | 3 (10%) | |
| Acral | 3 (10%) | 3 (10%) | |
| Site of patches | |||
| Head and neck | 22 (18.8%) | 17 (14.6%) | 0.434 |
| Trunk | 54 (46.1%) | 57 (49.1%) | |
| Limbs | 30 (25.6%) | 36 (31.1%) | |
| Acral | 11 (9.5%) | 6 (5.2%) | |
| Leukotrichia | |||
| Present | 5 (16.7%) | 6 (20%) | 0.74 |
| Absent | 25 (83.3%) | 24 (80%) |
SD = standard deviation
After 1 month of therapy, initiation of repigmentation was noted in 76 patches (65%) in Group A and 45 patches in Group B (38.7%) (P < 0.0001) [Table 3].
| Response on patches | Group A | Group B | P value |
|---|---|---|---|
| After 1 month | |||
| G0 | 41 (35%) | 71 (61.2%) | 0.0001 |
| G1 | 76 (65%) | 45 (38.7%) | |
| After 6 months | |||
| G4 | 55 (47%) | 5 (4.3%) | 0.03 |
| G3 | 54 (46.2%) | 10 (8.6%) | |
| G2 | 7 (6.0%) | 40 (34.5%) | |
| G1 | 1 (0.8%) | 61 (52.6%) | |
| Side effects | |||
| Pain | 12 (40%) | 0 (0%) | |
| Erythema | 20 (66.6%) | 18 (60%) | |
| Itching | 10 (33.3%) | 9 (30%) | |
| Ulceration | 2 (6.6%) | 2 (6.6%) | 0.25 |
At the end of 6 months, a statistically significant difference was observed between the two groups with better outcome in Group A, in which 47% of the patches had excellent response (>75% repigmentation) and 46.2% had very good response (50%–75% repigmentation). In Group B, 4.3% patches had excellent response and 8.6% had very good response (P = 0.03) [Table 3]. Loss of pigmentation was not seen in any patient.
Ulceration of lesions was seen in two patients in Groups A and B. Pain, erythema, and itching were more common in Group A, but no statistically significant difference was observed between the groups with regard to the adverse effects (P = 0.25) [Table 3]. Koebner’s phenomenon was not seen in any patient.
Site-wise analysis revealed that excellent response was most often seen in patches over the trunk followed by head and neck and limbs in both the groups. None of the acral lesions showed excellent response to any of the treatments [Figure 2].
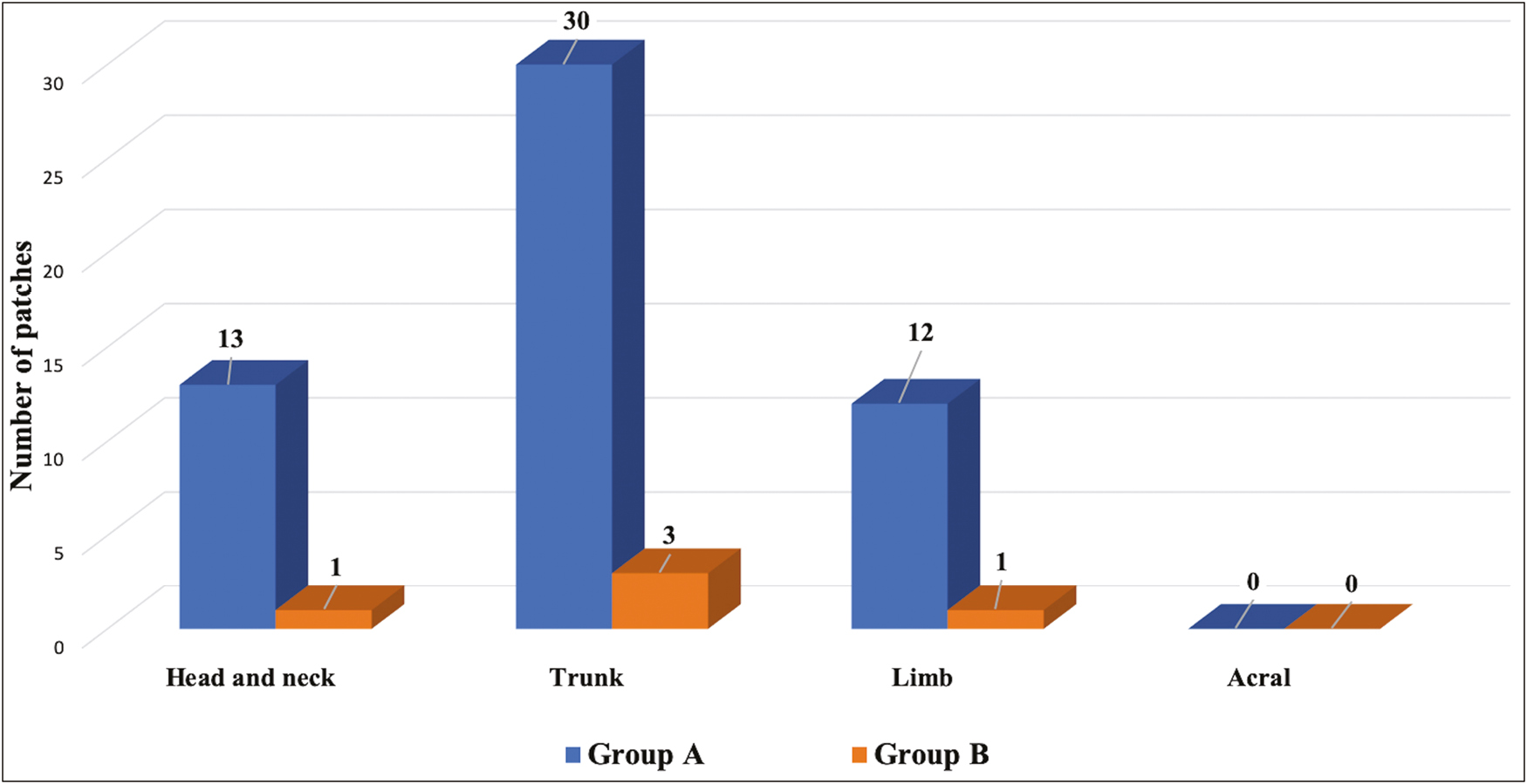
- Excellent response with respect to location of the patch
DISCUSSION
Vitiligo is an autoimmune disease produced as a result of interaction of environmental, genetic, and neural factors, leading to the destruction of melanocytes and appearance of depigmented macules. Vitiligo has a profound psychosocial impact on life, inculcating lowered self-esteem in patients.[9] In an Indian study of 30 patients, it was found that 10% patients of vitiligo had depression, one had anxiety, and one had suicidal ideation.[10] It is thus important to provide them with best possible modality of treatment and help them to cope up better. Therapy for vitiligo has to be chosen based on the nature and stability of disease, extent of involvement, age of the patient, and so on, from a myriad of medical and surgical modalities.
Tsuji and Hamada[11] introduced the method of application of 5-FU after therapeutic wounding as the treatment of vitiligo. Topical 5-FU has been used earlier either alone or in combination with dermabrasion and lasers.[1213] FU show selective and differential cytotoxicity toward epidermal cells. Melanocytes are less vulnerable to fluorouracil than keratinocytes. The mechanism of repigmentation suggested that 5-FU causes overstimulation of melanocytes of follicles, which migrates during epithelialization and induces pigmentation.[14] It is found in in vitro studies that 5-FU in low concentration selectively destroys keratinocytes in 3 weeks, whereas melanocytes continue to multiply and form pigment.[13]
Needling induces strong inflammatory response and local edema, leading to increased intercellular spaces of the basal layer. Active melanocytes migrate from pigmented epidermis through these spaces. The inflammatory mediators such as leukotrienes C4 and D4 and matrix metalloproteinases from keratinocytes help in melanocyte migration and proliferation.[1215] Several trials combining microneedling with another treatment modality have shown improved effectiveness in achieving regimentation in vitiligo. These also demonstrated lesser duration of treatment with reduced side effects.[8161718]
Our study constituted patients of age varying from 11 to 43 years, and the mean age of Group A and Group B patients was 29.4 and 24.2 years, respectively. A female predominance was observed in our study (60% in Group A and 63.3% in Group B). Similar study conducted by George et al.[13] noted female predominance in their study. A higher number of female patients have been found in clinico-epidemiological studies of vitiligo conducted by Handa and Dogra[19] and Gandhi et al.[20] This probably reflects the increased social stigma of vitiligo in female patients, and thus early treatment-seeking behavior.
Vitiligo vulgaris (61.7%) was the most common morphological pattern, followed by focal vitiligo (20%) in our study. These findings are consistent with a study conducted by Shashikiran et al.[18] who observed vitiligo vulgaris in 58% patients. George et al.[13] also found maximum number of patients of vitiligo vulgaris (73.3%) followed by focal vitiligo (26.7%).
At the end of 1 month, initiation of repigmentation in the form of erythema over the patches started in 76 patches (65%) of group A and 45 patches of group B (38.8%). However, Mina et al.[8] reported a start of repigmentation within 6 weeks in 44% patches of vitiligo treated with 5-FU combined with microneedling. The response to needling appears to be faster than effect of fluorouracil combined with microdermabrasion as studied by Garg et al.[21] who noted the start of repigmentation in 50% patches within 2 months. The faster response after needling could be due to the better penetration of the topical drug after needling.
At the end of 6 months, excellent repigmentation (>75% repigmentation) was noted in 47% patches of Group A and only 4.3% patches of Group B patients, whereas <50% repigmentation was seen in 6.8% and 87% patches of Group A and Group B respectively [Figures 3 and 4]. The results of our study are comparable to a study conducted by Shashikiran et al.[18] in which more than 75% repigmentation was reported in 49% of the patches. However, they noticed <50% repigmentation in 25% patches in their study. Mina et al.[8] noted excellent repigmentation in 48% patches treated with combined microneedling and 5-FU.
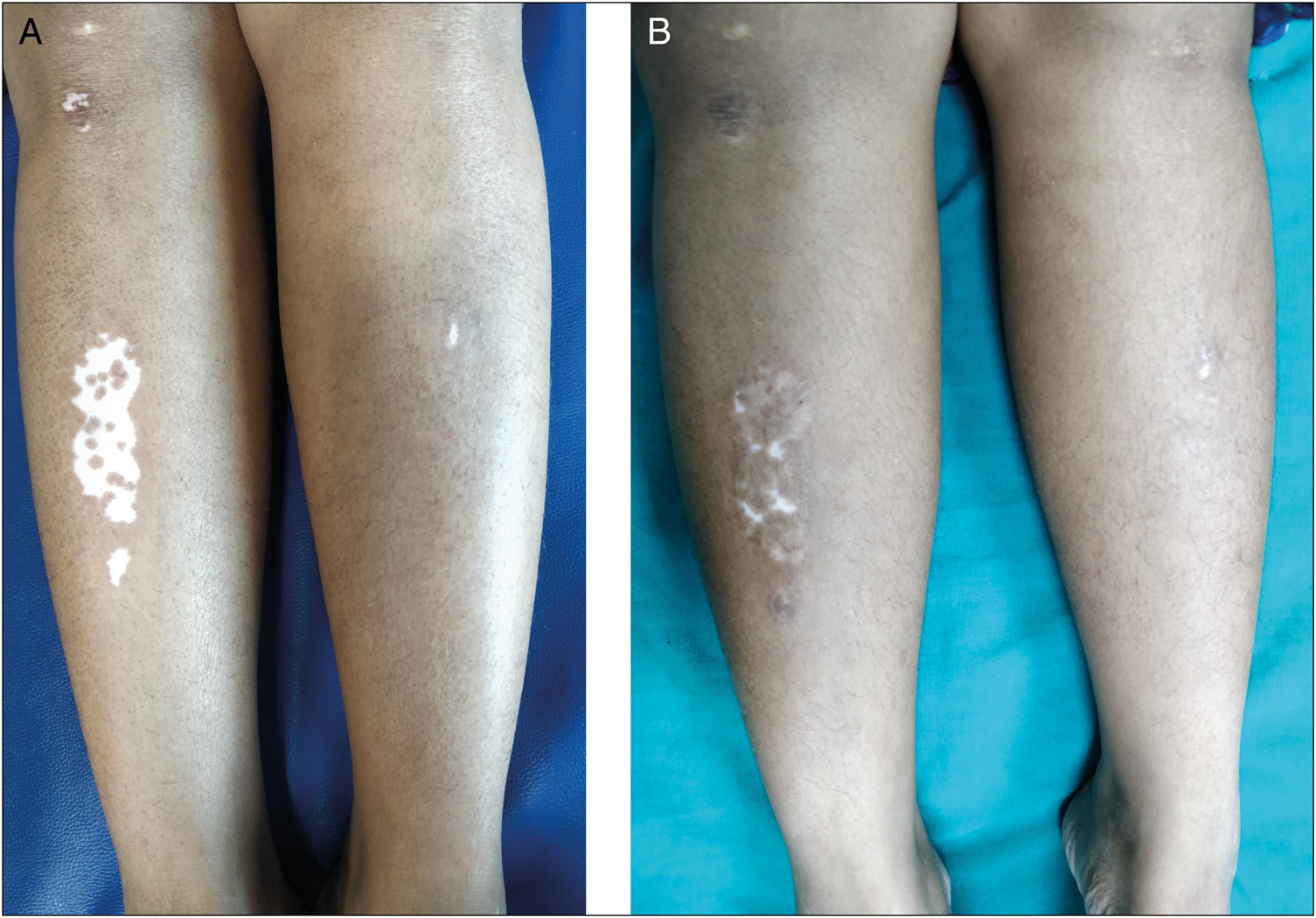
- G4 response (>75% repigmentation) in a vitiligo patch over the lower limb: (A) at baseline; (B) at 6 months
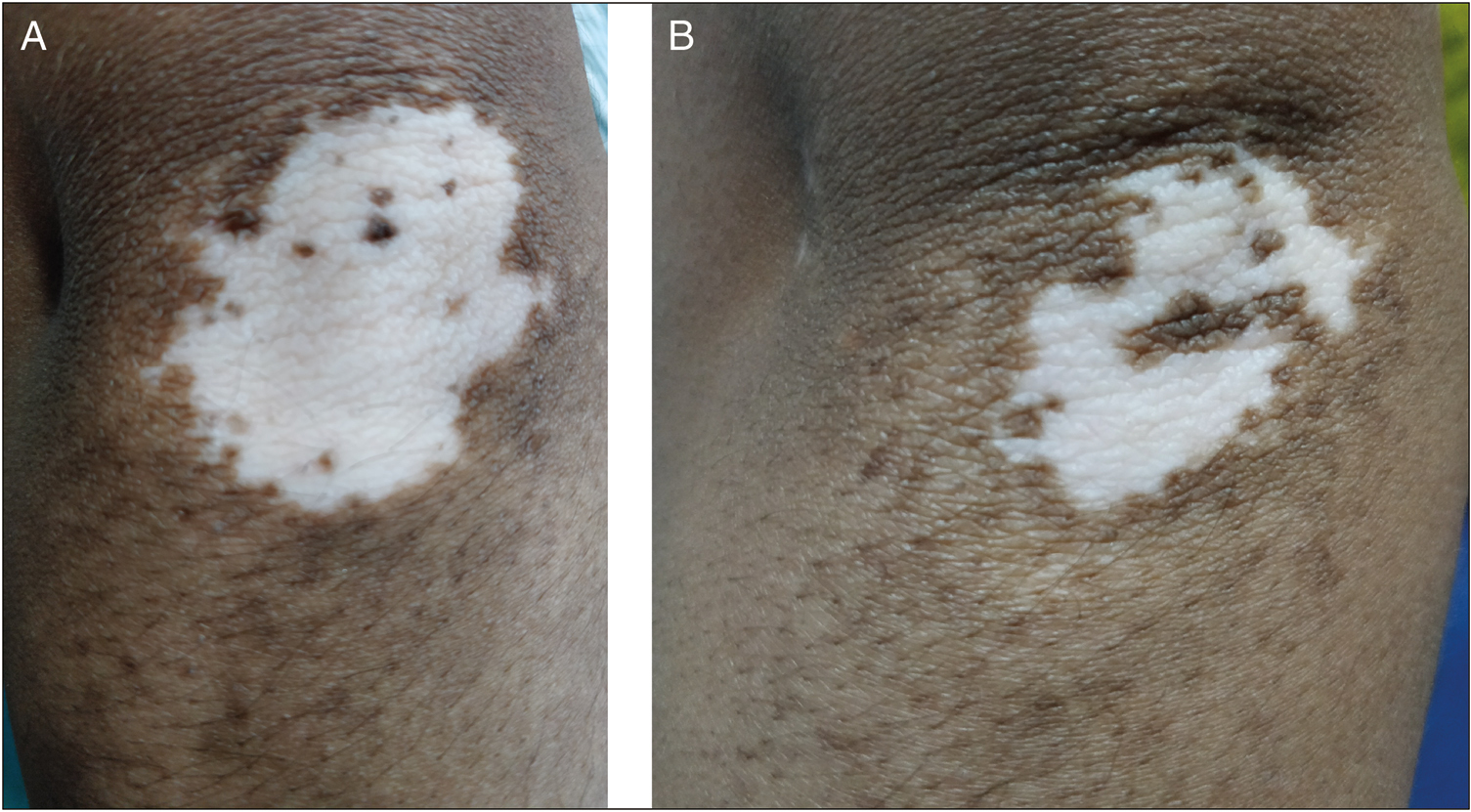
- G3 response (50%–75% repigmentation) in a vitiligo patch over the elbow: (A) at baseline; (B) at 6 months
Similar result was reported by Yones et al.[22] in a study of efficacy of dermabrasion plus topical 5-FU in stable vitiligo, in which they found excellent repigmentation in 45% patients.
A study conducted by George et al.[13] on the efficacy of laser dermabrasion followed by topical 5-FU in the treatment of stable vitiligo found nearly complete repigmentation in 40% patients.
Santosh et al.[23] found that after 3 months of treatment of vitiligo with 5-FU after microneedling of the lesion, approximately 60% of patients (30) had hyperpigmentation in the vitiligo lesions. There was almost complete pigmentation in very small patches; larger ones had less pigmentation and 40% (20) did not have any pigmentation from the previous state.
Only one patient of 27 (3.7%) showed excellent improvement in vitiligo patch treated with microneedling with dermapen after 5-FU application in an Egyptian study. Approximately 70% patients showed some improvement in the color of lesions. These patients showed 18.5% improvement when treated with microneedling alone.[24] Ghiya et al.[25] reported excellent response in 60% children of stable localized vitiligo treated with 5-FU solution followed by dermaroller. The high response rate can be attributed to the fact that patients received treatment every 15 days for 6 months.[25]Table 4 compares the various trials involving 5-FU after therapeutic wounding in vitiligo.
| Study | Author, year | Excellent repigmentation at the end of study period |
|---|---|---|
| Needling with 5% 5-FU | Current study | 47% patches at the end of 6 months |
| Mina et al.,[8] 2018 | 48% patches at end of 6 months | |
| Shashikiran et al.,[18] 2018 | 49% patches at the end of 6 months | |
| Santosh et al.,[23] 2018 | 60% patients at the end of 3 months | |
| Attwa et al.,[24] 2019 | 3.7% patients at the end of 3 months | |
| Ghiya et al.,[25] 2016 | 60% patients at the end of 6 months | |
| Dermabrasion with topical 5-FU | Sethi et al.,[26] 2007 | 73.3% patches at the end of 6 months |
| Yones et al.,[22] 2013 | 45% patients at the end of 3 months | |
| Garg et al.,[21] 2011 | 25% patches at the end of 2 months (4 sessions) | |
| Laser dermabrasion followed by topical 5-FU | George et al.,[13] 2017 | 40% patients at the end of 3 months |
| Mohamed et al.,[27] 2015 | 49.8% patches at the end of 5 months | |
| Intradermal 5-FU with NB-UVB therapy | Abd El-Samad and Shaaban,[28] 2012 | 48.3% patients at the end of 4 months |
NB-UVB = narrow band-ultraviolet B
In our study, maximum number of truncal lesions showed the best response, and acral lesions were the least responsive. This was consistent with the results of Shashikiran et al.[18] Leukotrichia and bony locations have been linked to the poor response of treatment in literature.[29]
In our study, pain was experienced by 12 (40%) patients of Group A and none of the patients in Group B, whereas erythema, itching, and ulceration were observed in few patients of both the groups. The adverse effects of erythema, itching, and ulceration were in accordance with a study by Shashikiran et al.[18] However, they recorded pain during the procedure in all the patients (100%). The lesser occurrence of pain in our study can be attributed to the use of topical anesthetic sprayed before the procedure. Mina et al.[8] observed ulceration in 4% patients, which is consistent with our findings. Sethi et al.[26] reported erythema and serous discharge in all patients, formation of pseudomembrane, and hypertrophic scarring in their study. Loss of pigmentation was not seen in any of our patients probably due to the short follow-up period after the intervention. No systemic side effect was reported in our study, thereby making use of topical FU along with needling safe and effective therapeutic modality in the treatment of vitiligo.
Limitations of our study included an unblinded design and a short follow-up period. This study also did not evaluate the efficacy of the intervention on mucosal vitiligo. Further, we did not use any tool that measures changes in vitiligo from the patient’s perspective. The use of a 26-gauge needle might be economically convenient but it is prone to produce an inferior wound than a dermaroller or a dermapen.
We found that needling followed by topical application of 5-FU has much higher efficacy than 5-FU alone in vitiligo. It is a useful therapy in poor responders to conventional therapy. However, the stability of repigmentation has to be analyzed with longer period of follow up.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Vitiligo: compendium of clinico-epidemiological features. Indian J Dermatol Venereol Leprol. 2007;73:149-56.
- [Google Scholar]
- Autologous miniature punch skin grafting in stable vitiligo. Indian J Dermatol Venereol Leprol. 1992;58:310-4.
- [Google Scholar]
- Repigmentation in vitiligo vulgaris by autologous minigrafting: results in nineteen patients. J Am Acad Dermatol. 1995;33:990-5.
- [Google Scholar]
- Treatment of “stable” vitiligo by timed surgery and transplantation of cultured epidermal autografts. Arch Dermatol. 2000;136:1380-9.
- [Google Scholar]
- Comparison between the efficacy of microneedling combined with 5-fluorouracil vs. microneedling with tacrolimus in the treatment of vitiligo. J Cosmet Dermatol. 2018;17:744-51.
- [Google Scholar]
- The psychosocial impact of vitiligo in Indian patients. Indian J Dermatol Venereol Leprol. 2013;79:679-85.
- [Google Scholar]
- Psychiatric morbidity in psoriasis and vitiligo: a comparative study. J Dermatol. 2001;28:419-23.
- [Google Scholar]
- The effect of ER:YAG plus 5-fluorouracil on the outcome of punch grafting in nonsegmental vitiligo: a left–right comparative study. Egypt J Dermatol Venerol. 2016;36:4-10.
- [Google Scholar]
- Efficacy of laser dermabrasion followed by topical 5-fluorouracil in the treatment of stable vitiligo. Int J Health Sci Res. 2017;7:144-7.
- [Google Scholar]
- Differential effects of 5-fluorouracil on human skin melanocytes and malignant melanoma cells in vitro. Acta Derm Venereol. 1986;66:474-8.
- [Google Scholar]
- Successful treatment of vitiligo by needling with topical 5 fluorouracil. Pigment Disord. 2016;3:242.
- [Google Scholar]
- 5-fluorouracil as an adjuvant therapy along with microneedling in vitiligo. J Am Acad Dermatol. 2019;80:e75-6.
- [Google Scholar]
- Microneedling with dermaroller 192 needles along with 5-fluorouracil solution in the treatment of stable vitiligo. J Am Acad Dermatol. 2019;81:e67-9.
- [Google Scholar]
- Efficacy of topical 5% fluorouracil needling in vitiligo. Indian J Dermatol Venereol Leprol. 2018;84:203-5.
- [Google Scholar]
- Epidemiology of childhood vitiligo: a study of 625 patients from north India. Pediatr Dermatol. 2003;20:207-10.
- [Google Scholar]
- A study of clinico-epidemiological and dermoscopic patterns of vitiligo in pediatric age group. Indian J Paediatr Dermatol. 2017;18:292.
- [Google Scholar]
- Combination of microdermabrasion and 5-fluorouracil to induce repigmentation in vitiligo: an observational study. Dermatol Surg. 2011;37:1763-6.
- [Google Scholar]
- Efficacy of dermabrasion plus topical 5-fluorouracil in stable vitiligo. Gulf J Dermatol Venereol. 2013;20:31-4.
- [Google Scholar]
- Treatment of vitiligo with 5-fluorouracil after microneedling of the lesion. Int J Sci Stud. 2018;5:125-7.
- [Google Scholar]
- Evaluation of the additional effect of topical of 5-fluorouracil to needling in the treatment of localized vitiligo. J Cosmet Dermatol. 2020;19:1473-8.
- [Google Scholar]
- Comparative evaluation of the therapeutic efficacy of microneedling alone or microneedling combined with topical 5-fluorouracil in localized stable childhood vitiligo. Adv Hum Biol. 2016;6:25-8.
- [Google Scholar]
- Comparative evaluation of the therapeutic efficacy of dermabrasion, dermabrasion combined with topical 5% 5-fluorouracil cream, and dermabrasion combined with topical placentrex gel in localized stable vitiligo. Int J Dermatol. 2007;46:875-9.
- [Google Scholar]
- Carbon dioxide laser plus topical 5-fluorouracil: a new combination therapeutic modality for acral vitiligo. J Cosmet Laser Ther. 2015;17:216-23.
- [Google Scholar]
- Treatment of localized non-segmental vitiligo with intradermal 5-flurouracil injection combined with narrow-band ultraviolet. Br J Dermatol Treat. 2012;23:443-8.
- [Google Scholar]






