Translate this page into:
Expert Consensus on Soft-tissue Repositioning Using Absorbable Barbed Suspension Double-needle Threads in Asian and Caucasian Patients
Address for correspondence: Dr. Salvatore Piero Fundaro, MultiMed Poliambulatorio e Day Surgery, Via Fornaciai 29/d Bologna, Italy. E-mail: dr.fundaro@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Bioabsorbable barbed suspension double-needle threads have recently been thrust into the limelight as a minimally invasive alternative for skin repositioning. When compared to surgical face lifting, use of these threads requires reduced procedural and recovery time, no general anesthesia, confers immediate patient satisfaction, with no cutaneous incisions and no apparent scars, and is more tolerable. There is currently limited literature providing clinical guidance on the use of these suspension threads; hence, this consensus document was developed as the first publication to discuss the technical aspects of facial rejuvenation using the double-needle barbed bioabsorbable and hydrolyzable thread composed of copolymer poly (ε-caprolactone-co-L-lactic acid) or PCxLyA, that is, Definisse threads. The Board of Aesthetic Leaders and Investigators (BALI) is a panel of dermatologic surgery and plastic surgery experts who convened last July 2018 in Indonesia to discuss the aforementioned challenges. A thorough literature search was done where a review of specific technical recommendations based on prevailing practice and available guidelines pertaining to suspension threads were described and are summarized in this paper. A detailed list of pretreatment recommendations in the assessment of both Asian and Caucasian facial types, aging facial types, guidance on insertion techniques, and aftercare instructions for clinicians to review has been included here.
Keywords
Asian
bioabsorbable barbed suspension double-needle thread
Caucasian
consensus guidelines
poly (ε-caprolactone-co-L-lactic acid)
The use of barbed thread suspension threads repositioning and tightening of facial tissue is now recognized as an important tool for aesthetic medicine. Threads can be used to achieve a nonsurgical soft-tissue repositioning to a certain extent. Procedural and technical aspects have been outlined to help learning practitioners understand the versatility of the thread for use in Asian and Caucasian facial types.

INTRODUCTION
Facial soft-tissue repositioning has mainly been achieved through surgical face lifting, a complex and radical procedure that is socially stigmatized, associated with surgical risks (e.g., infection, necrosis, hematomas, seromas, facial nerve injury, scarring, anesthetic reactions) and unwanted downtime.[123] To address these concerns, advanced minimally invasive procedures have emerged recently. In this article, the Board of Aesthetic Leaders and Investigators (BALI) discusses the technique of facial tissue repositioning and rejuvenation using double-needle barbed bioabsorbable and hydrolyzable threads from poly (ε-caprolactone-co-L-lactic acid) or PCxLyA, that is, Definisse threads (RELIFE S.r.l., Florence, Italy).
BALI, a group of international dermatologic surgery and plastic surgery experts from around the world, convened last July 2018 in Indonesia to identify pointers for treating aging concerns in both Asian and Caucasian patients. Through focus group discussions, consensus-building sessions, teleconferencing, and online polling sessions, they outlined recommendations useful for tissue repositioning using bioabsorbable double-needle PCxLyA suspension threads.
MATERIALS AND METHODS
Concurrently, a literature search of the Medline, Embase, and Google Scholar databases was done using the search terms “Asian,” “Caucasian,” “eastern,” “western,” “global,” “management,” “thread lifting,” “suspension threads,” “review,” “meta-analysis,” “systematic review,” “evidence-based,” and “aesthetics.” Materials included recent meta-analyses, clinical practice guidelines, reviews, and clinical trials relevant to thread lifting. The search involved a selection of journal articles published before August 31, 2018. Finally, specific recommendations were described based on prevailing best practices.
DISCUSSION
Choosing needles and threads
Soft-tissue repositioning using bioabsorbable threads does not require long procedural and recovery time, general anesthesia, is well tolerated and leads to immediate patient satisfaction.[45] Suspension threads safely reposition facial tissue by anchoring and lifting ptotic facial tissue with lasting effects.[56] Although several threads (e.g., Anti-Ptosis or Aptos, monofilament barbed, cone anchoring system) have been developed, they follow the same principle of repositioning and interposing soft tissue around a thread consequently triggering an inflammatory response and fibrosis.[378910] Since then, a few techniques using varying materials applied to specific areas, such as the mid-face, lower face, or neck area, have been introduced.[5]
Bidirectional threads have eliminated the need for skin incisions by introduction of a cranial anchoring stitch on fascia. It also reduced the migration and visibility of threads often seen in monodirectional threads. More recently, absorbable copolymers with customizable mechanical properties have been produced. Poly (ε-caprolactone) is a semicrystalline material displaying rubbery properties, whereas poly (L-lactic acid) is a crystalline, hard, and brittle material. When combined as a copolymer, it becomes an attractive replacement for common threads because of its controllable elasticity and adjustability due to the capacity to change the ε-caprolactone/lactic acid molar ratios.[11]
Threads are also categorized based on mode of absorption and surface smoothness.[35,6111213] Nonabsorbable threads such as polypropylene, remain unhydrolyzed in the skin, whereas absorbable threads are prone to enzymatic hydrolysis. Polydioxanone (PDO), poly-L-lactic acid, polyglycolic acid, poly-lactic-polycaprolactone acid (PCxLyA) are examples. Their stability in vivo depends on the microstructure of the polymer from which they are made so they have varying decomposition rates. PDO takes approximately 6 months to be absorbed, whereas PCxLyA decomposes for several weeks to months.[11]
Smooth threads do not have barbs or cones and are used for tissue bio-revitalization only. Biostimulation with PDO wires during the first 12-month posttreatment causes neocollagenesis and fibrillogenesis and retraction of the fibrosed dermis producing a tightening effect.[14] However, the long-term safety (i.e., undermined skin texture) and efficacy (i.e., sustainability of the lift effect after dissolution of the thread) of this technique requires more in-depth scientific studies. Nonsmooth threads have small projections that radiate outward from the center of the thread that anchor and lift sagging skin.[1213,15] The thread is introduced into the tissues in the opposite direction of the splay of the barb, allowing it to glide without engaging the tissues. Pulled in the opposite direction, the threads embed in the fatty fibrous adipose tissues transferring the force, anchor in the tissues, and maintain the suspension, to elevate the overlying dermis and skin.[4] Depending on the barb direction, threads can be subcategorized as either bidirectional or monodirectional.
Bidirectional threads have barbs in opposite directions and a central smooth area used to facilitate insertion. The bidirectional and convergent thread may be inserted via a needle/cannula (free-floating thread) or via two needles located at two ends of the thread (double-needle thread). Once inserted, the barbs are fixed into place by bidirectional traction.[15] Monodirectional threads have barbs angled in one direction. This type needs a fixing point created with a stitch on the opposite side of the barbed part to reduce the tendency to move forward and migrate often leading to dislocation and spontaneous extrusion. Some come with a straight needle at one extremity of the barbed part and a curved thread needle for fixing the stitch on the other end.
The Definisse double-needle threads
Definisse double-needle threads are absorbable, monofilament, suspension barbed threads of synthetic origin with convergent bidirectional spines. The 12 cm thread has two parts with bidirectional and convergent spines that are found on each side. At the central part of this thread, there is a smooth area that is approximately 1 cm long. The 23-cm variant has spines along its length on both sides and a central smooth part that is 1.5 cm long. At each extremity, there is a straight cut-edge double-needle that is (1) 100 mm long with a diameter of 0.8–0.83 mm for the 12-cm-long thread and (2) 150 mm long with a diameter of 1.26–1.28 mm for the 23-cm-long thread [Figure 1].
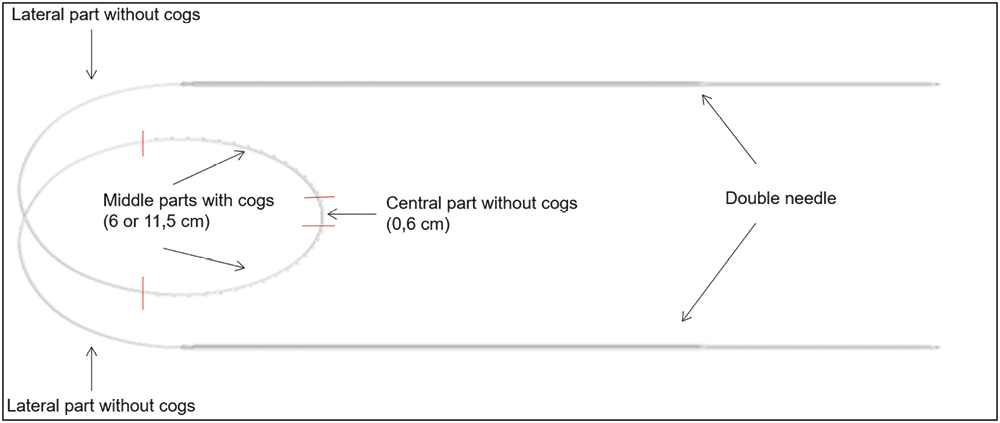
- Definisse double-needle threads
- Two variations: 12 cm with two 6-cm-long parts with bidirectional,convergent spines; 23 cm with two 11.5-cm-long parts with bidirectional, convergent spines; a straight cut edge needle is at each extremity; central portion has no barbs
Two straight needles are used to insert the thread in different directions depending on the technique used. This specific insertion modality and the ability to create an angle between the two thread tracks allow for various insertion patterns and the creation of anchoring points that increase thread grip. When the thread is pulled, an angled path creates a compression of the tissue located between the two sides of the angle that increases the pressure of the barbs on soft-tissue connective fibers. This point is often referred to as the “angle of strengthening.”
Anatomical considerations
The subcutaneous layer comprises subcutaneous fat, which provides volume and mobility to the skin, and by the fibrous retinacula cutis, which connects the dermis with the underlying superficial musculoaponeurotic system (SMAS). Superficially, the subcutaneous layer has fine retinacula cutis fibers. The fibrotic network of the retinacula cutis becomes sparser while thicker fibrotic branches emerge as one goes deeper (i.e., pre-SMAS). This specific organization of the retinacula cutis affects the interaction between the barbs and the fibrotic network of the subcutaneous fat.
The subcutaneous fat of the face is highly partitioned, that is, not a confluent mass and has distinct anatomical compartments.[16] These compartments are delineated by ligaments or septa that arise from periosteal plane and pass through the superficial fascia and insert into the dermis of the skin.[1718] The superficial fat compartments are localized between the skin and the plane of the SMAS.[192021] The superficial fat compartments are the infraorbital fat (IF), superficial medial cheek fat (SMCF), nasolabial fat (NLF), middle cheek fat (MCF), lateral temporal-cheek fat (LTCF), superior jowl fat (SJF), and inferior jowl fat (IJF) compartments. Beneath the SMAS plane, the deep fat compartments extend and adhere to the periosteum. The deep fat compartments are the medial suborbicularis oculi fat (M-SOOF), lateral suborbicularis oculi fat (L-SOOF), deep medial cheek fat (DMCF), and buccal fat (BF) compartments [Figure 2A].[2223] IF, SMCF, and NLF are referred to collectively as the “malar fat pad.”[24] In younger individuals, the malar fat pad is supported in its location by multiple fibroelastic fascial septa. These septa extend through the fatty cheek mass originating from the underlying superficial fascia that invests the facial expression muscles into the overlying dermis.[25]
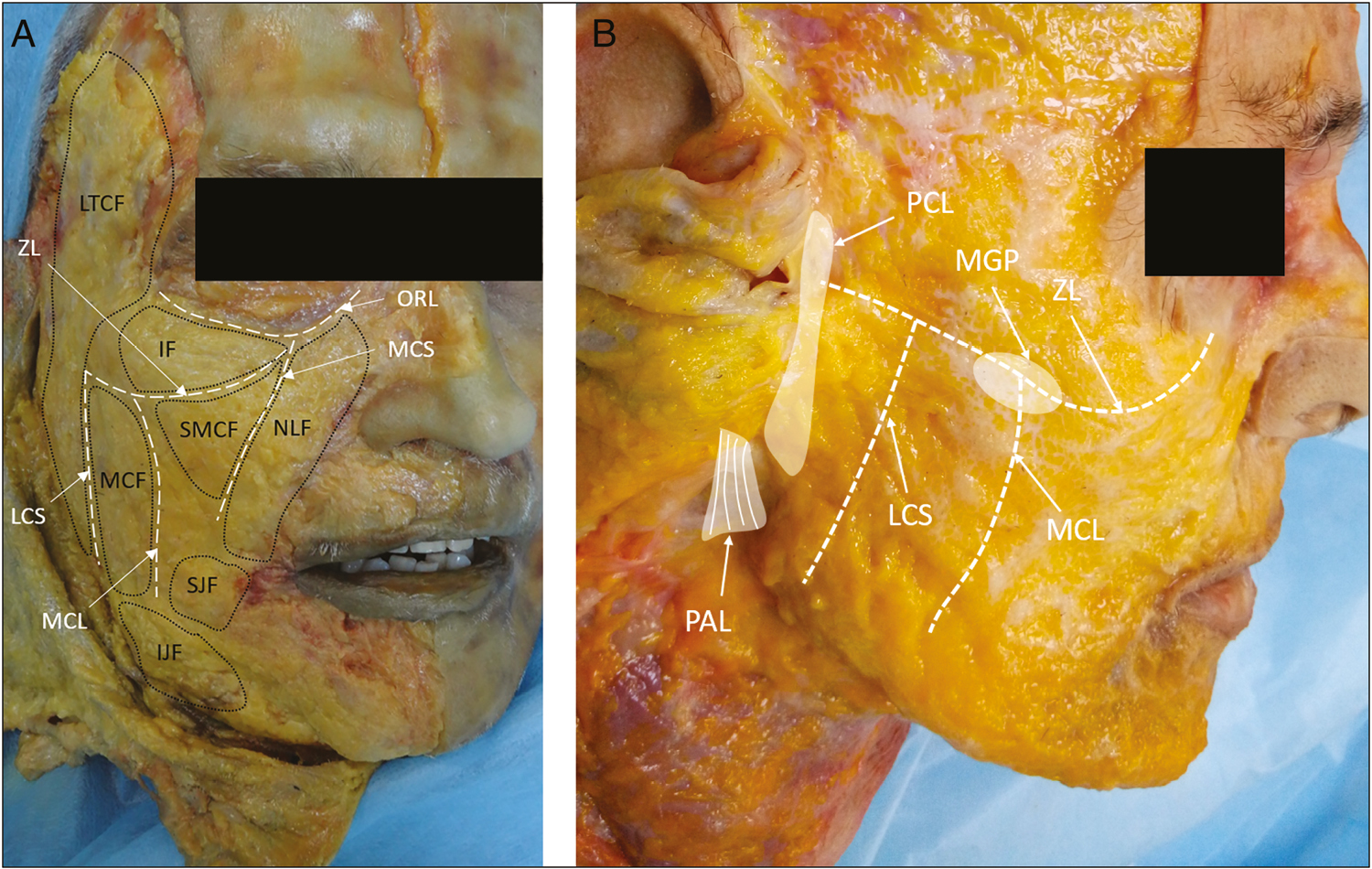
- (A) Superficial fat compartments (B) Main ligaments used as anchoring points
- IF = infraorbital fat, SMCF = superficial medial cheek fat, NLF = nasolabial fat, MCF = middle cheek fat, LTCF = lateral temporal-cheek fat, SJF, IJF = superior, inferior jowl fat, ORL = orbicularis retaining ligament, ZL = zygomatic ligament, MCS = medial cheek septum, MCL = masseteric cutaneous ligament, LCS = lateral cheek septum, ZL = zygomatic ligament, MGP = Mc Gregor patch, PCL = parotid cutaneous ligament, PAL = platysma auricular ligament
Fat compartments undergo specific changes due to aging.[2627] The SMCF and NLF undergo a global increase in volume and ptosis.[28] These changes enlarge the lower malar fat pad, often described as “hypertrophic.” This is seen as marked deepening of the nasolabial fold.[2528] The MCF is loosely adherent to SMAS plane and its aging is characterized by slight ptosis, caudal migration, and fat augmentation.[28] These changes produce an increase of the convexity in the central portion of the cheek often evident in ectomorphs. Both the SJF and IJF undergo ptosis and hypertrophy that lead to the formation of marionette’s line and jowl defects. Finally, the LTCF lies on and is adherent to the parotid fascia without any deep fat compartment in between. A hypotrophic involution of this compartment occurs in contrast to the superficial fat compartments. The LTCF is adherent to parotid fascia and is a fixed fat compartment, which makes it a good place to anchor threads.
The ligaments of the face serve as anchoring points for the barbed threads and are of two types: the osteocutaneous ligaments that connect the periosteum to the dermis passing through all anatomical layers of the face, and fasciocutaneous ligaments that coalesce between the superficial and deep fasciae of the face.[29]
The ligaments located in the upper and lateral part of the cheek offer a strong anchoring point reinforcing the thread-repositioning capability of the superficial fat compartment. The main retaining structures used as anchoring points are[293031323334]: (1) the Mc Gregor patch, (2) the platysma auricular ligament, (3) the parotid cutaneous ligament, and (4) the zygomatic ligament [Figure 2B].
Patient suitability and assessment
The facial shape, aging features, asymmetry, and anatomy (e.g., skin thickness, neurovascular roadmaps, salivary gland size, and placement) should be evaluated. The extent of anatomical modification guides the choice of modality for repositioning and helps one identify the fat compartments needing repositioning and along which vectors. Inappropriate correction will likely lead to suboptimal results.
“Ideal” patients are between 30 and 60 years and should have trophic skin, compact facial fat, and with nonsevere signs of aging. Good bone projection, normotrophic, or hypertrophic facial fatty tissue usually have better results as opposed to thin, hypoelastic, fibrotic, dry skin, with extremely hypotrophic superficial fat compartments, and highly relaxed facial ligaments.[35]
The authors use the Aging Type Classification (ATC) scale to determine a patient’s suitability for this procedure [Table 1].[36]
| Type | Appearance | Anatomic changes |
|---|---|---|
| Type 1: Hypotrophic | • Cheek appears flat or concave • NLFs and marionette lines appear due to “pseudoptosis” (i.e., loss of underlying soft tissue) of the skin, which becomes redundant • Jawline skin sags |
• Hypotrophy of superficial (SMCF, SLF, MCF, SJF and IJF) and deep fat compartments (medial and lateral SOOF and DMCF) |
| Type 2: Hypotrophic/ptotic | • Cheek appears concave at the infraorbital area while appearing convex and ptotic at the nasolabial compartment • Lower cheek slightly convex |
• Hypotrophy of deep fat compartments • NLF and SMCF ptosis • Ptosis of MCF, SJF and IJF |
| Type 3: Ptotic/hypertrophic | • Infraorbital area appears flat or slightly concave • Convex nasolabial region • Prominent nasolabial fold • Convex lower cheek |
• Hypertrophy and ptosis of SMCF and NLF • Hypertrophy and ptosis of MCF, SJF and IJF • Slight hypotrophy of deep fat compartments (L-SOOF, M-SOOF, DMCF) |
| Type 4: Hypertrophic/ptotic | • Cheek appears concave only at the nasojugal groove but convex elsewhere and at the nasolabial region • Convex lower cheek with demarcation of the LTCF |
• Hypertrophy with secondary ptosis of the superficial and deep fatty tissues of the cheeks • Ptosis of the nasolabial fold accentuated by hypertrophy • Hypotrophic LTCF |
DMCF = deep medial cheek fat, IJF = inferior jowl fat, L-SOOF = lateral suborbicularis oculi fat, LTCF = lateral temporal-cheek fat, MCF = middle cheek fat, M-SOOF = medial suborbicularis oculi fat, NLF = nasolabial fat, SJF = superior jowl fat, SMCF = superficial medial cheek fat
Types 1 and 2 are appropriate as the first choice for volume augmentation of hypotrophic fat compartments. After volume restoration, especially in the case of skin sagging, they may be treated with suspension threads. In type 3 patients, aging is characterized mainly by the ptosis of hypertrophic superficial fat compartments in combination with a volume reduction of deep fat. The repositioning of superficial fat with threads could be the first therapeutic choice followed by volume restoration of deep compartments with fillers. Type 4 patients are characterized by an excessive facial volume and consequent soft-tissue ptosis; therefore, the only choice is volume repositioning with suspension threads. Often, the results would depend on the weight of fatty tissue and on the quality of retinacula cutis and its interaction with threads. If there is high volume of fat is or if the quality of the SMAS is compromised, soft-tissue repositioning may have limited effects.
Assessment of the patient’s medical and surgical history is fundamental.[37] Physicians should watch out for dermatological issues and allergic history to lidocaine, epinephrine, or thread materials. Generally, ruling out recognizable personality disorders and abuse of illicit substances is a must.[38]
Facial aging of Asian and Caucasian faces
Asians have facial features and specific attractiveness parameters that differ from those of Caucasians. They have a wider face with shorter vertical height and a flat or concave medial maxilla. They have a lack of brow, nasal, and chin projection. Caucasian faces generally have more pronounced three dimensionality with larger, more deeply set eyes, greater anterior projection of the brow, nose, maxilla, and chin. Caucasians also tend to have narrower faces and greater vertical height. In addition, because Asians have a greater infraorbital volume, larger midface width, and fuller lips, these provide for a more stable youthful look. These, along with stronger facial septa and ligament system, a thicker SMAS fibrotic network, more compact facial fat compartments, and a thicker skin enable them to resist environmental insults and show delayed signs of physiological and anatomical aging.[394041424344]
Because of their facial dimensions and anatomy, insertion techniques that reposition soft tissues laterally are less preferred because these will further widen the face. The goal for these patients is to achieve a more vertical repositioning of soft tissue using vertical vector techniques and to reduce the volume along the jawline and redistributing it in midface.[35]
Thread insertion techniques in detail
The space between the dermis and the SMAS is the insertion plane. In this space, the subcutaneous tissue is divided into various fat compartments by the ligaments and the septa of the face [Figure 3]. It is important to avoid inserting too superficially or too close to the dermis.[35] A deep insertion on normal or thick skin, close to the SMAS plane, reduces the interaction between thread and retinacula cutis and decreases the visibility and palpability of the thread.
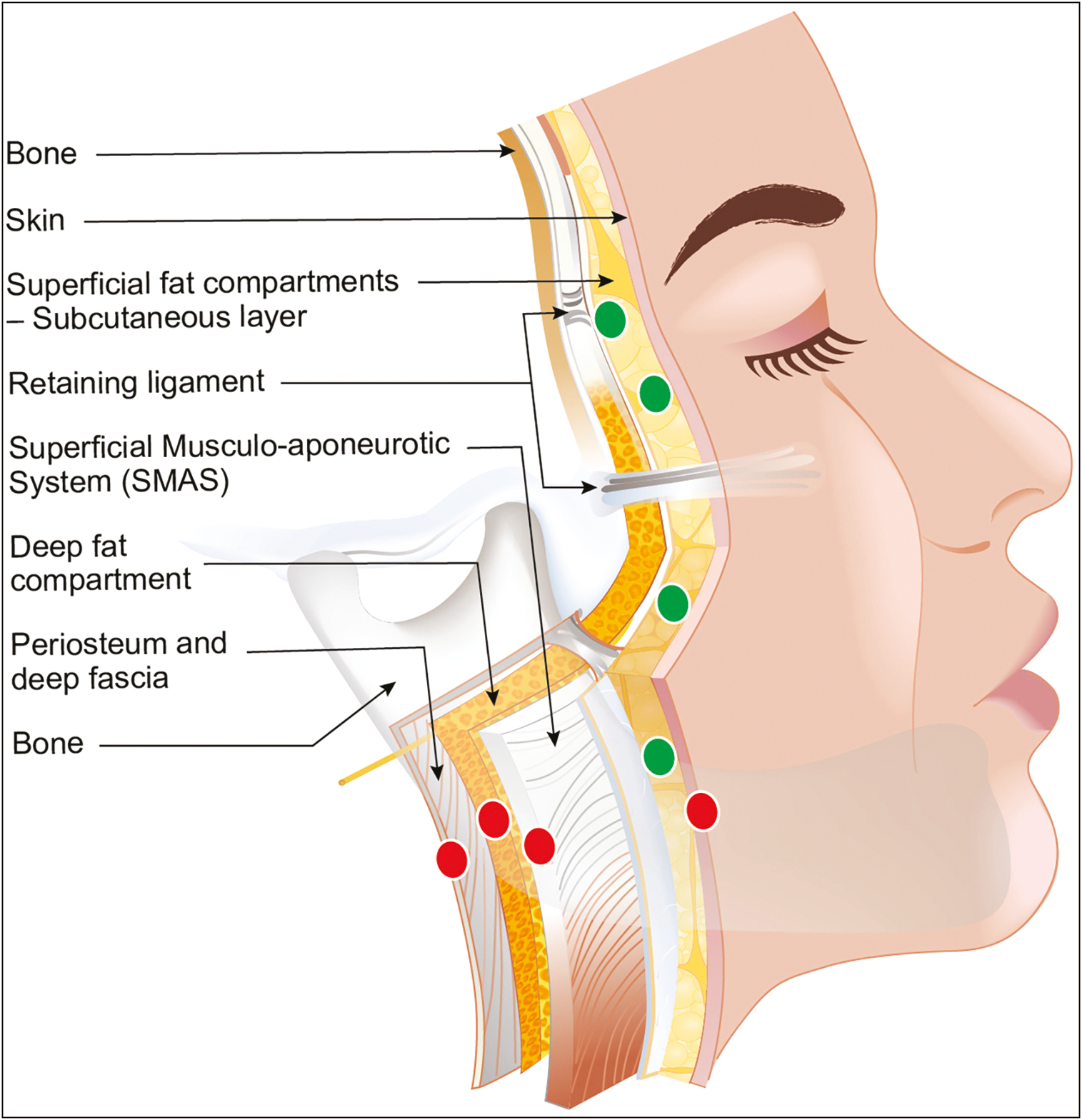
- The correct insertion plane is at the subcutaneous plane (green dots); insertion that is too superficial or under the SMAS plane (red dots) is ineffective because apart from failure to reposition, it can lead to injury of important structure
The main insertion techniques are classified as lateral vector or vertical vector technique [Figure 4]. These techniques are based on the principal direction of the repositioning vectors specific for each technique [Table 2]. The lateral vector (LV) technique includes the (1) jawline reshaping (JR), (2) malar reshaping (MR), and (3) lateral reshaping (LR) techniques. The vertical vector (VV) techniques includes the (1) oval reshaping––vertical technique (OR-V) and oval reshaping––H technique (OR-H).
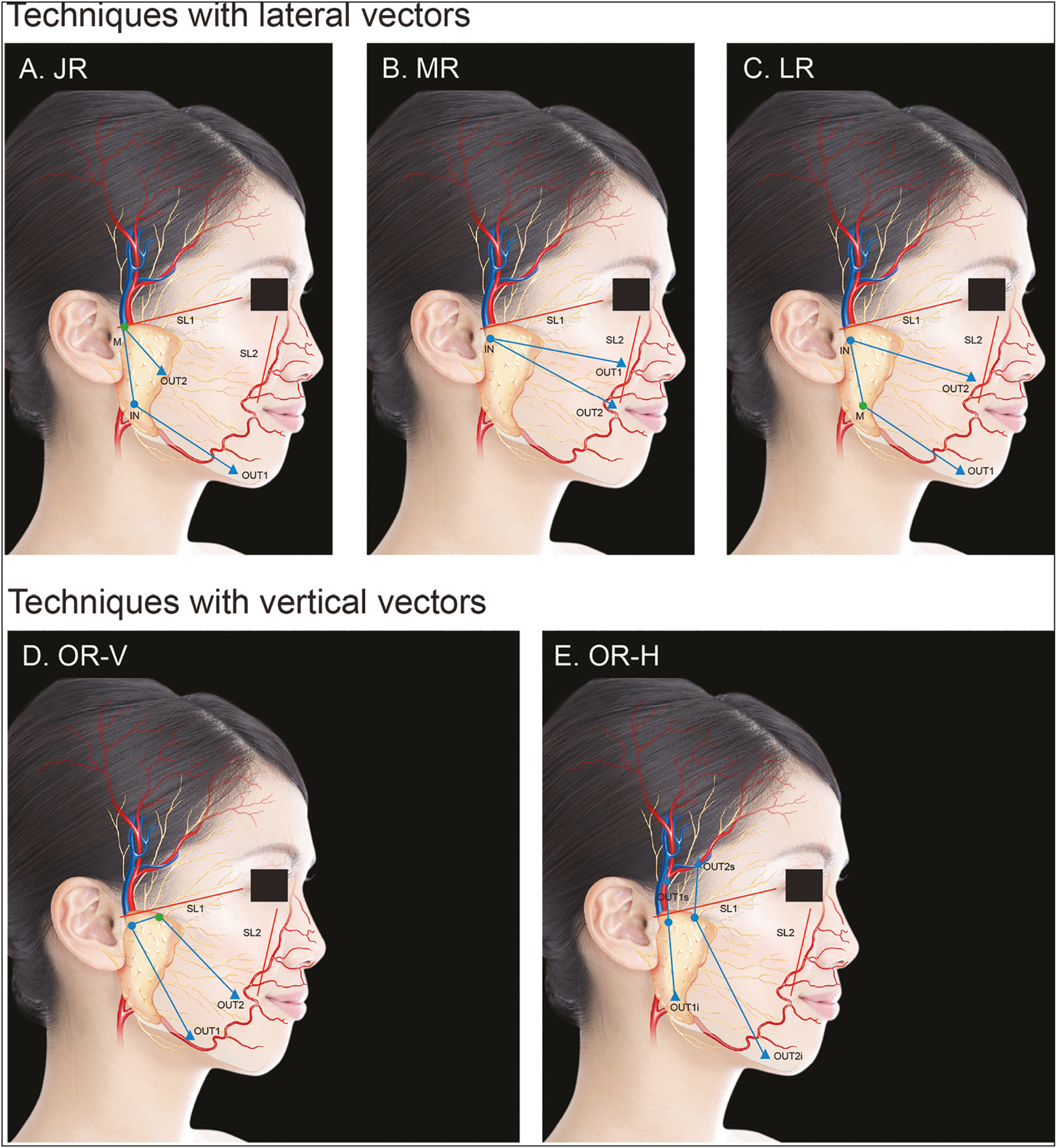
- Landmarks of the different insertion techniques
- Techniques A, B, and C are based on lateral vectors and are indicated in patients that need facial width enlargement, as often done in Caucasians; D and E are based on vertical vectors and provide a vertical repositioning of soft tissues and are often indicated in Asians
- SL = safety lines, IN = entry point, OUT = exit point, M = intermediate point; blue lines = reshaping lines
| Jawline reshaping (JR) technique |
|---|
| Purpose: |
| • For reshaping of the frame of the jawline and repositioning ptotic tissues of the lower face |
| • Indicated in Asian and Caucasian patients (types 1, 2, 3, and 4). |
| • Increases the width and definition of mandibular angles, which is not preferred by many Asians |
| Thread: |
| • Double-needle 12-cm threads |
| Technique: |
| • The IN is marked at the infra-auricular region between the ear lobe and the posterior border of the platysma muscle. In this area, Furnas identified the platysma auricular ligament and described it as an “intricate fascial condensation that often attaches intimately to the overlying skin.”[30] This trapezoidal structure provides a firm anchorage between the platysma and the dermis of the inferior auricular region. It is a strong fixation point into the area where the thread creates an angle. |
| • The OUT1 is in the upper preauricular area, close to the sideburns and OUT2 along the jawline, at the medial border of the IJF. OUT2 should be located always laterally to the marionette line to avoid traction on the skin fold of the marionette lines. To increase the anchoring action and to create a strong fixation point at the more cranial part of the thread, the J stitch is done at OUT2. |
| • The RLs join the IN with OUT1 and OUT2 as it indicates where the needle traverses into the subcutaneous tissue mindful of the supra-SMAS plane. The section of the thread following RL2 runs along the preauricular area where it is anchored at the parotid cutaneous ligament. |
| •After the insertion, the external portion of the thread at the cranial exit point, where the J stitch has been performed, is pulled: This allows the barbs to grasp the fibro-adipose tissue of the pre and infra-auricular areas. At OUT2, the external part of the thread is pulled, whereas the palm of the other hand gently repositions the superficial soft tissues along the thread closer toward the entry point. |
| • When the anchoring part has stably grasped the surrounding tissues and the suspension part has achieved adequate tissue repositioning, the excess threads are cut with the rest seen disappearing into the skin. |
| Malar reshaping (MR) technique |
| Purpose: |
| • For reshaping the facial frame by lifting the superficial fat compartments of the malar and cheekbone area superiorly and laterally |
| • Indicated mainly in Caucasian and Asian patients type 3 and 4 |
| Thread: |
| • Double-needle 12 cm threads |
| • Larger facial areas may need 23 cm long threads |
| Technique: |
| • The IN point is in the upper preauricular area close to SL1. This area corresponds to the zygomatic arch, along which the lateral portion of zygomatic cutaneous ligament runs. The presence of a ligamentous structure at IN increases the anchoring strength. |
| •The two OUTs are located close to the SL2 and laterally to the nasolabial fold. The distance between these OUTs is determined based on the patient’s clinical characteristics and goals of treatment. If both are located at the level of nasolabial fat, the action will be more focused on the malar fat pad repositioning and nasolabial fold improvement. If OUT2 is moved downward, at the level of SJF, the repositioning will target repositioning of this fat compartment to soften the marionette line. The two halves of the thread run through the superior and inferior portion to the McGregor patch surrounding this strong ligamentous structure located over the zygomaticotemporal suture and along the upper margin of the masseter muscle. |
| • The first half of the thread is inserted along the RL1, from IN and OUT1, whereas the second half along IN and OUT2. Once inserted, the two ends will be pulled together, whereas the malar fat pad is draped and repositioned toward the IN point by the other hand. Once the correct repositioning of tissues is achieved, the excess threads are cut with the rest seen disappearing into the skin. |
| Lateral reshaping (LR) technique |
| Purpose: |
| • For reshaping the facial frame by lifting the superficial fat compartments of a large part, that is, the upper and lower areas, of the cheek superiorly and laterally |
| • Indicated mainly in Caucasian patients type 3 and 4 |
| • Increases the width of the face so it is less indicated in Asians |
| • For repositioning of the NLF and SMCF and of SJF and IJF along the jawline to reshape the soft tissues of mandibular angle |
| • More useful in Caucasian patients [Figure 5] |
| Thread: |
| • Double-needle 23-cm threads |
| Technique: |
| • IN is located close to the sideburns in the upper pre auricular zone. M is located at the infra-auricular region between the ear lobe and the posterior border of the platysma muscle on the platysma auricular ligament. |
| • OUT1 is located along the jawline at medial border of IJF. OUT2 is close to SL2 and the nasolabial fold. The craniocaudal location of OUT2 can vary according to the manner of malar fat pad repositioning. |
| • The RLs run from IN to M and OUT1 (RL1) and from IN to OUT2 (RL2). The two parts of the thread are inserted along these RLs. IN uses the pretragal portion of the zygomatic ligament for strengthening. The portion between IN and M uses the parotid cutaneous ligament and the M is located over the platysma auricular ligament: Anchoring into these strong ligaments allows for a wide and stable area for lifting. |
| • The first half of the thread is inserted along RL1, from IN and OUT1, whereas the second half along IN and OUT2. Once the thread is inserted following the general techniques along the paths described above, the two ends are drawn up, whereas the other hand drapes and repositions the superficial compartments toward the lateral part of the cheek where anchoring occurs. Once the correct repositioning of tissues is achieved, the excess threads are cut with the rest seen disappearing into the skin. |
| Oval reshaping-vertical (OR-V) technique |
| Purpose: |
| • For reshaping the facial frame in order to make the face appear oval [Figure 6] |
| • For lifting the mid- and lower-face superficial fat compartments of the cheek |
| • Indicated in Asian patients type 2, 3, and 4 and in Caucasian patients type 3 and 4 |
| • Generally indicated in a patient with large and round face |
| Thread: |
| • Double-needle 23-cm threads |
| • Smaller faces may require only 12-cm long threads |
| Technique: |
| • IN is located close to the sideburn in the upper preauricular zone. It is important to create the entry hole slightly cranial to the inferior border of the zygomatic process to assure that the first anchoring point is placed correctly above the lateral part of zygomatic ligament. M is located 2–3 cm medially from IN, still cranial to the inferior border of zygomatic arch to ensure that the thread between IN and M bounds the zygomatic ligament superior to the McGregor patch for anchoring. |
| • The two OUTs are located close the jawline: OUT1 above IJF and OUT2 approximately 1 or 2 cm medial to the mandibular angle. For a more effective repositioning of the SJF, OUT1 could be moved close to this fat compartment. The positions of these OUTs can vary based on the specific features of each patient. |
| • The first needle is inserted through the entry hole created by an 18-G needle and pulled out at M. The thread is inserted till the central part without barbs reaches the middle point between IN and M. Afterward, the first needle is introduced through the intermediate hole and inserted into the subcutaneous fat tissue until the needle tip reaches OUT1. At this point, the needle can be pulled out through the skin with the entire first portion of the thread inserted. The second needle is then inserted through the entry hole and drawn out at OUT2. |
| • The fatty tissue of cheek (mainly the MCF, SJF, and IJF) are raised upward along the vertical vectors while gently drawing both the threads downward with the other hand, carefully repositioning the cheek soft tissues toward the zygomatic arch. Once the correct repositioning of tissues is achieved, the excess threads are cut with the rest seen disappearing into the skin. |
| Oval vertical-H (OV-H) technique |
| Purpose: |
| • Vertically reshapes the frame of the face |
| • Indicated in Asian patients type 2, 3, and 4 and in Caucasian patients type 3 and 4 |
| • Generally indicated in patient with large and round face |
| Thread: |
| • Double-needle 12-cm threads (creates an H shape upon insertion––hence, the name OV-H) |
| Technique: |
| • This technique is characterized by the positioning of anchoring part of threads in the temple region, beyond the SL1 that lies between the upper margin of the tragus and the external eye canthus. The insertion of the needle in the temporal area is done taking care to insert in the correct anatomical plane: The subcutaneous fat tissue above the superficial temporal fascia. IMPORTANT: Inside this fascia lies the frontal branch of superficial temporal artery and underneath of it the frontal branches of facial nerve. Avoid damage to these structures by identifying the correct plane. |
| • IN of the first thread is marked along the zygomatic arch, cranial to its inferior border and anterior to the sideburn. OUT1 is in the temporal region close to hair line. The OUT2 point is located close to the jawline. The RL1 connects the IN to OUT1 and the RL2 the IN and OUT2. Insert the needle as previously described but this time, parallel to the skin inside the subcutaneous fat until the needle tip reaches OUT1. The skin is pierced, and needle pulled out to insert the first half of thread. The J stitch is done at the level of OUT1. Afterward, the second needle is introduced through the entry point and, once the correct insertion layer is achieved, it is kept parallel to the skin along the RL2 into the subcutaneous tissue. The skin is pierced at OUT2 and the needle extracted. The second thread is inserted in the same way: using the same insertion path that lies parallel to the previous thread in a more medial position. |
| • With a hand placed flat on the skin of the cheek, the soft superficial tissues are displaced cranially toward the zygomatic arch, whereas the other hand draws the ends of the threads in the other direction. Finally, stabilize and increase the strength of anchoring parts by pulling the two external threads of the J stitches. Once the correct repositioning of tissues is achieved, the excess threads are cut with the rest seen disappearing into the skin. |
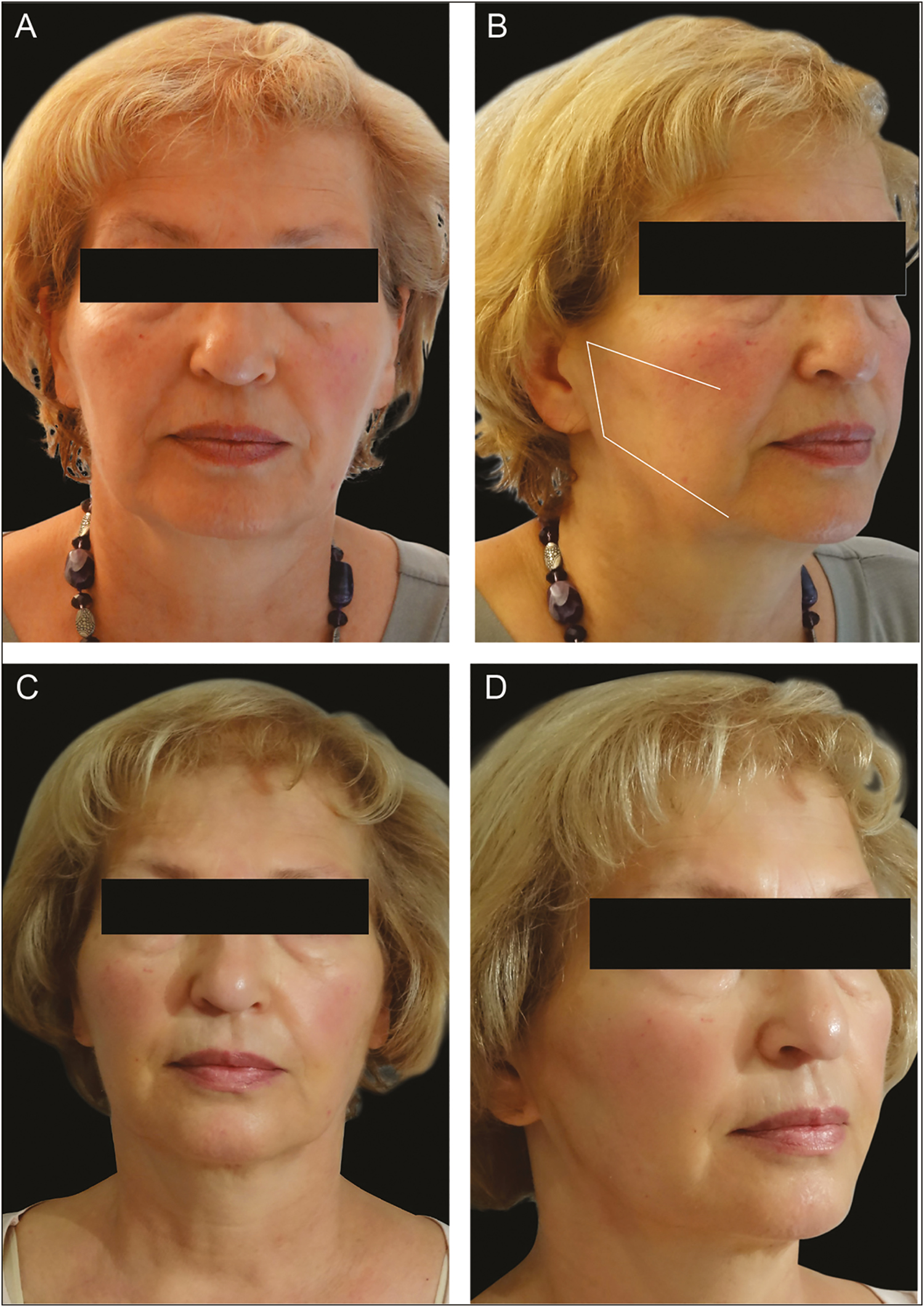
- Before and after: The lateral reshaping (LR) technique
- The patient has been treated with two 23-cm double-needle threads on each side using the LR technique; preprocedure right oblique and frontal views (A and B); follow-up after 1 month (C and D)
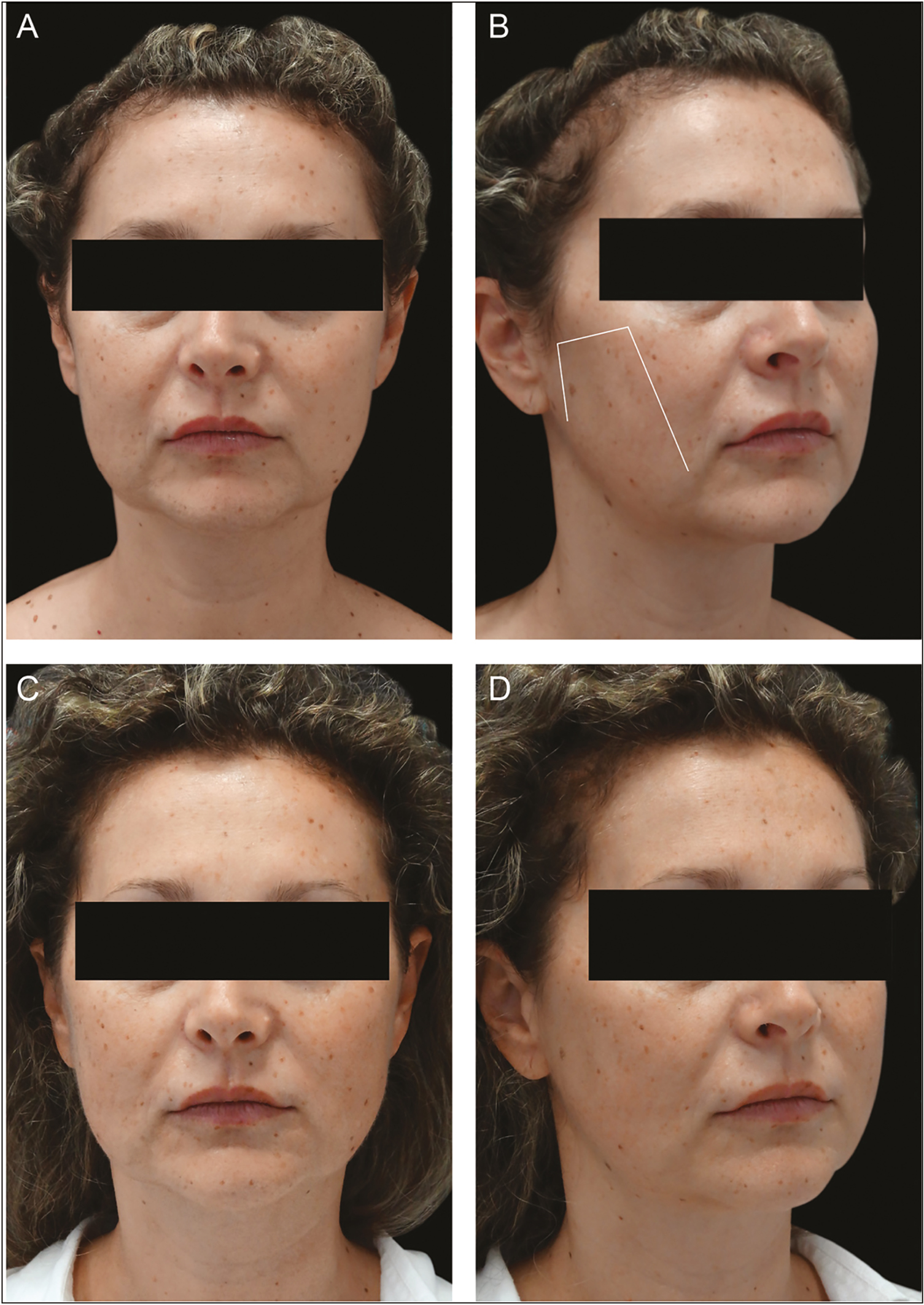
- Before and after: The oval reshaping-vertical (OR-V) technique
- The patient has been treated with two 23-cm double-needle threads on each side using the OR-V technique. Preprocedure right oblique and frontal views (A and B). Follow-up after 1 month (C and D)
Insertion planning
The first step is outlining of the insertion path on the skin with a dermatograph pencil. The marks include the entry point (IN), the two exit points (OUTs), and depending on the technique used, an intermediate point (M) and the reshaping lines (RLs). The RLs represent the path of the thread once inserted. Two safety lines (SLs) are also drawn: the first, from the upper margin of the tragus to the external eye canthus (SL1), and the second, from the internal canthus to the modiolus (SL2). Vital anatomical structures outside the two SLs, like big vessels or nerve branches, should be avoided. Because the soft tissues that cover them are thinner, these structures are often more superficial. Any insertion beyond these lines requires a higher level of skill and attention.
Local anesthesia and surgical field preparation
After drawing, surgical field preparation and local anesthetic injection with lidocaine and epinephrine 1:100.000 are done at the IN and OUT points and optionally, along RLs between the IN and OUT. It is important to set up a minimal yet adequate surgical field before executing the procedure with the threads. All materials and instruments (i.e., gauze, scissors, needle, and single-use surgical drape) must be sterile. After cleaning, an accurate skin disinfection of all the face and of the hairline with chlorhexidine 20% is mandatory. A sterile surgical drape fitted with an adequate central hole is put on one-half of the face. Performing the local anesthesia first followed by surgical tray preparation is preferred to give time for vasoconstriction.
Thread insertion
At the IN point, an 18-G needle is used to vertically perforate the entire thickness of the skin. The perpendicularity of the entry hole relative to the skin is an important aspect of the insertion because it facilitates the correct introduction of the needle and the barbed thread. Through this hole, the tip of one of the two needles is vertically placed. Correct insertion reduces the risk of skin dimpling due to traction.
The tip of the needle is introduced below the dermal layer and, once it reaches the subcutaneous layer, it should be rotated and kept parallel to the skin and introduced into the subcutaneous layer above the SMAS plane along the planned RL. During insertion, the same depth should be kept for the entire length of the RL. Once the tip of the needle reaches the OUT point, the skin should be pierced with the needle to create an exit point. The needle should exit throughout the OUT perpendicularly with respect to the skin layer to reduce intradermal passage at the exit point.
While pulling out the needle from the OUT, be aware that the central part without barbs should reach the entry hole at IN. At this point, the second needle should be inserted into the same entry hole, taking care to insert it through the same path created by the 18-G needle. The introduction technique for the second needle is the same as the first. The second needle is inserted parallel to the skin layer following the second RL, until the second OUT, where the exit point was created. The second part of the thread is completely inserted and the central tract without barbs is introduced completely below the dermal layer through the entry hole. Finally, the two needles are carefully cut, and the two external parts of the thread are pulled, whereas the superficial soft tissues are carefully “draped” along the thread closer toward the entry point.
Some techniques (LR, OR-V, JR) require an intermediate point (M), a pivot point where the needle exits the skin and then back in again before its final exit at an OUT point. The M point is intended to create a sharp change in direction of thread path and to create a strong anchoring point through the so-called J stitch. To avoid skin dimpling, it is important to reinsert the needle exactly through M, so the barbs slip through the hole without grasping the dermis.
The “J stitch” is a means to reinforce suspension at the anchoring point to allow a stable and effective tissue repositioning. It is performed only in JR and OR-H and is done by reintroducing the needle into the cranial exit hole while being rotated at a 20° to 30° angle with respect to the inserted thread. On insertion for approximately 2 cm, the needle is taken out through the skin. At this point, the needle is completely pulled out and the thread is drawn until it completely penetrates the dermis. The acute angle between the two tracts of thread and the orientation of the barbs in opposite directions considerably increase the holding force and the resistance to slipping of the thread. This effect is due to the compression on the tissues located between the two arms of the angle helping secure the barbs on to the connective tissue fibers.
Aftercare
At the end of the procedure, an ice pack may be applied especially when bleeding at entry and exit points or when a hematoma is noted. It is important to provide a full list of instructions regarding aftercare to avoid untoward events and to help yield optimal results. It is not recommended to apply ice at home because it is difficult to advise regarding the correct pressure and duration of application. After the procedure small adhesive dressings are applied. It is recommended to maintain the dressing and clean only once daily with antiseptic for approximately 3–5 days or longer if needed.[15]
Applying makeup should be postponed up to 24h after the procedure. Vigorous washing or any sort of manipulation of the face may dislodge the thread. Washing or shaving or make-up removal should be done as carefully as possible without massaging or rubbing the affected areas of the face.[15]
Patients should be advised not to engage in strenuous activities for 2 weeks and are required to stop smoking and drinking alcoholic beverages. Exposure to direct sunlight or use of tanning beds is to be avoided for approximately 2 weeks. Also, they are advised to sleep with the face upright for at most 3 nights and to avoid prolonged opening of the jaw (i.e., dental procedures) for approximately 3 weeks. Other aesthetic procedures of the face and neck are also to be avoided for at least 3 weeks.
Mild analgesics, specifically oral acetaminophen, can be taken to control pain. Advise against the use of anti-inflammatory drugs as this may lead to bruising. Short-term antibiotic therapy may be beneficial (e.g., amoxicillin or clarithromycin for 5 days). A routine follow-up should be scheduled from days 3 to 5 after the procedure, and then a few weeks after to fully document treatment subjective (e.g., pain assessment) and objective outcomes (e.g., photographic documentation).[15]
Prevention and management of complications
Mild bruising, neural pain or paresthesia, edema, inflammation, dimpling, and irregularities/asymmetry may occur. These are often temporary, that is, ≤7–10 days, and often fully recover with supportive therapy.
Bruising and edema may be avoided with accurate, slow, and careful thread insertion. The injection of lidocaine with epinephrine along the insertion lines may help reduce the risk of these events. Applying an ice pack for 20–30 min immediately after the procedure can help in reducing swelling and inflammation.[45]
Gentle traction of the thread to avoid overcorrecting is vital in preventing nerve injury, pain, dimpling, and irregularities. The asymmetric repositioning of soft tissues on the two sides of the face is normal immediately after the insertion and often disappears after a few days. If needed, adjustments can be done before cutting the extremities of the threads.[45]
Hemorrhage and hematoma can be a result of damage to one of the main vessels at the deep planes. Awareness of the space between the dermis and the SMAS plane is important. In the event of profuse bleeding, manual compression is advised together with application of an ice pack for 30 min. For the next 2 days, an ice pack wrapped in a towel may be used for 10–15 min three to four times a day may be done with supervision. After 48h, a warm washcloth may be applied on the hematoma for 10 min for two to three times a day to facilitate the absorption of the hematoma. Arnica or vitamin K-based creams may be considered where available. In rare severe cases of hematoma, a surgical drain may be used.[45]
Insufficient traction of the thread on one side, thread rupture, or unhooking barbs may cause asymmetry. Repeating the procedure or correcting the undertreated side may resolve.[45]
Visibility and palpability of the thread can be prevented by avoiding superficial insertion. A vigorous massage along the thread course is rarely effective and removal of the thread may be necessary. When obviously displaced or extruded but without the signs of infection, the thread may simply be cut after adequate disinfection. Infection may be controlled by oral antibiotics and a topical antibiotic cream. If it persists, complete and urgent thread extraction will have to be done. In some cases, a formal face lift may be considered after removal of the threads.[4546]
A sialocele may arise as a result of the iatrogenic trauma of the parotid gland parenchyma. This is treated with conservative approaches such as repeated aspiration and the use of compression dressings.[45] Botulinum toxin A injection (i.e., 30–50 U) has been documented to be effective and safe for use as treatment for parotid sialocele after fluid aspiration.[47] In the event of a parotid duct rupture, specialist referral should be immediately arranged for possible emergency duct stenting and repair.[46]
As barbed suspension threads have become recognized as an essential tool for repositioning and tightening of facial tissue, clinicians should be aware of these outcomes. These threads have great versatility for use in Asian and Caucasian facial types and can be used to achieve nonsurgical lift to a certain extent.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors of the article have received honoraria from A. Menarini Asia Pacific, Pte Ltd for their participation in the meeting.
Acknowledgement
The authors would like to acknowledge Dr. Dennis Malvin H. Malgapo of MIMS Pte Ltd Medical Communications for medical writing support.
REFERENCES
- Expert consensus on absorbable advanced suspension technology for facial tissue repositioning and volume enhancement. J Drugs Dermatol. 2017;16:661-6.
- [Google Scholar]
- The convergence of medicine and neurotoxins: A focus on botulinum toxin type A and its application in aesthetic medicine––a global, evidence-based botulinum toxin consensus education initiative: Part I: Botulinum toxin in clinical and cosmetic practice. Dermatol Surg. 2013;39:493-509.
- [Google Scholar]
- Facial thread lifting with suture suspension. Braz J Otorhinolaryngol. 2017;83:712-9.
- [Google Scholar]
- Thread lift : Classification, technique, and how to approach to the patient. Int J Medical, Heal Biomed Bioeng Pharm Eng. 2016;10:547-55.
- [Google Scholar]
- Thread lift with absorbable monofilamentthreads. J Japan Soc Aesthetic Plast Surg. 2013;35:1-12.
- [Google Scholar]
- APTOS suture lifting methods: 10 years of experience. Clin Plast Surg. 2009;36:281-306, viii.
- [Google Scholar]
- Medical textiles: Application of an absorbable barbed bi-directional surgical suture. J Text Apparel, Technol Manag. 2002;2:1-5.
- [Google Scholar]
- Suture with resorbable cones: Histology and physico-mechanical features. Aesthet Surg J. 2016;36:NP122-7.
- [Google Scholar]
- Preparation of biodegradable and elastic poly(ε-caprolactone-co-lactide) copolymers and evaluation as a localized and sustained drug delivery carrier. Int J Mol Sci. 2017;18:671.
- [Google Scholar]
- Outcomes in thread lift for facial rejuvenation: A study performed with happy lift™ revitalizing. Dermatol Ther (Heidelb). 2014;4:103-14.
- [Google Scholar]
- Outcomes of polydioxanone knotless thread lifting for facial rejuvenation. Dermatol Surg. 2015;41:720-5.
- [Google Scholar]
- Histologic evaluation of a biorevitalisation treatment with PDO wires. Aesthetic Surg J. 2015;1:111-7.
- [Google Scholar]
- Use of barbed threads in facial rejuvenation. Indian J Plast Surg. 2008;41:S93-S100.
- [Google Scholar]
- The fat compartments of the face: Anatomy and clinical implications for cosmetic surgery. Plast Reconstr Surg. 2007;119:2219-27; discussion 2228-31.
- [Google Scholar]
- The retaining system of the face: Histologic evaluation of the septal boundaries of the subcutaneous fat compartments. Plast Reconstr Surg. 2008;121:1804-9.
- [Google Scholar]
- Vascularized membranes determine the anatomical boundaries of the subcutaneous fat compartments. Plast Reconstr Surg. 2009;123:695-700.
- [Google Scholar]
- The superficial musculo-aponeurotic system (SMAS) in the parotid and cheek area. Plast Reconstr Surg. 1976;58:80-8.
- [Google Scholar]
- Mechanical properties and microstructure of the superficial musculoaponeurotic system. Plast Reconstr Surg. 1996;98:59-70; discussion 71-3.
- [Google Scholar]
- The youthful cheek and the deep medial fat compartment. Plast Reconstr Surg. 2008;121:2107-12.
- [Google Scholar]
- The mandibular septum: Anatomical observations of the jowls in aging-implications for facial rejuvenation. Plast Reconstr Surg. 2008;121:1414-20.
- [Google Scholar]
- The extended minimal incision approach to midface rejuvenation. Facial Plast Surg Clin North Am. 2005;13:411-9.
- [Google Scholar]
- Some anatomical observations on midface aging and long-term results of surgical treatment. Plast Reconstr Surg. 2008;121:258-68.
- [Google Scholar]
- Update on treatment rationale and options for the ageing face. Curr Opin Otolaryngol Head Neck Surg. 2011;19:269-75.
- [Google Scholar]
- The science and theory behind facial aging. Plast Reconstr Surg Glob Open. 2013;1:e8-e15.
- [Google Scholar]
- Aging changes of the midfacial fat compartments: A computed tomographic study. Plast Reconstr Surg. 2012;129:263-73.
- [Google Scholar]
- The relationship of the superficial and deep facial fascias: Relevance to rhytidectomy and aging. Plast Reconstr Surg. 1992;89:441-9; discussion 450-1.
- [Google Scholar]
- Surgical anatomy of the lower face: The premasseter space, the jowl, and the labiomandibular fold. Aesthetic Plast Surg. 2008;32:185-95.
- [Google Scholar]
- Anatomicohistologic study of the retaining ligaments of the face and use in face lift: Retaining ligament correction and SMAS plication. Plast Reconstr Surg. 2002;110:1134-47; discussion 1148-9.
- [Google Scholar]
- SMAS fixation to the facial skeleton: Rationale and results. Plast Reconstr Surg. 1997;100:1834-42; discussion 1843-5.
- [Google Scholar]
- Surgical anatomy of the midcheek and malar mounds. Plast Reconstr Surg. 2002;110:885-96; discussion 897-911.
- [Google Scholar]
- Innovative minimal invasive techniques in facial reshaping using barb suspension thread surgery IMCAS Academy [Internet]. c2018. Available from: https://www.imcas.com/en/academy/blog/415/innovative-minimal-inv
- Management of patients with risk factors. GMS Curr Top Otorhinolaryngol Head Neck Surg. 2013;12:Doc02.
- [Google Scholar]
- Consensus on changing trends, attitudes, and concepts of Asian beauty. Aesthetic Plast Surg. 2016;40:193-201.
- [Google Scholar]
- Management of the aging face in the Asian patient. Facial Plast Surg Clin North Am. 2007;15:353-60, vi-vii.
- [Google Scholar]
- Consensus on current injectable treatment strategies in the Asian face. Aesthetic Plast Surg. 2016;40:202-14.
- [Google Scholar]
- Comparison of age-related changes in facial wrinkles and sagging in the skin of Japanese, Chinese and Thai women. J Dermatol Sci. 2007;47:19-28.
- [Google Scholar]
- Comparison of age-related changes in wrinkling and sagging of the skin in Caucasian females and in japanese females. J Cosmet Sci. 2004;55:351-71.
- [Google Scholar]
- Reshaping with barbed threads (2020th ed). Torino, Italy: Edizioni Minerva Medica; 2020.
- Stensen duct rupture (sialocele) and other complications of the aptos thread technique. Plast Reconstr Surg. 2006;118:1468-71.
- [Google Scholar]
- A pilot study evaluating the treatment of postparotidectomy sialoceles with botulinum toxin type A. Arch Otolaryngol Head Neck Surg. 2000;126:421-4.
- [Google Scholar]





