Translate this page into:
Innovative post-traumatic ectropion repair – A case report
*Corresponding author: Ritu Gujarati Vishwanath, Department of Dermatology Venereology and Leprology, RiVa Skin and Plastic Surgery Clinic, Hanamkonda, Telangana, India. drrituvarun@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Vishwanath V, Vishwanath RG, Vishwanath R. Innovative post-traumatic ectropion repair – A case report. J Cutan Aesthet Surg. doi: 10.25259/jcas_66_24
Abstract
Eyelid ectropion is the outward turning of the eyelid away from the globe of the eye. Trauma is one of the acquired causes of ectropion. The scar can pull the eyelid and lead to cicatricial ectropion. It causes dryness of the eye, watering, exposure to keratitis, and a great psychological impact on the patient. Correction is needed to protect the eye and improve esthetic appearance. Many treatment modalities, such as regional flaps and transconjunctival flaps, were described earlier which are complex. We present an innovative approach to post-traumatic ectropion repair with simple scar revision and threads.
Keywords
Traumatic ectropion
Scar excision
Threads
INTRODUCTION
Eyelid ectropion is an anatomic malposition in which the eyelid is turned away from the globe of the eye. Beyond esthetic consequences, it may lead to pain, dryness, irritation, foreign body sensation, tearing, erythema, conjunctivitis, corneal ulcers, and scarring. Acquired eyelid ectropion can be involutional, cicatricial, paralytic, or mechanical. The cicatricial type is typically caused by scarring of the lower eyelid caused by trauma and burns.1 Scars are a natural and normal part of healing following an injury to the integumentary system, predominantly the reticular dermis.2 Cicatricial ectropion causes a great psychological impact on the patient. Correction is important to protect the eye, improve esthetic appearance, and boost social confidence. We present a case of post-traumatic ectropion repair with simple scar revision and threads.
CASE REPORT
A 26-year-old male presented with the left lid retraction for 1 year. There was associated dryness of eyes and dripping of tears. There was a history of a road traffic accident 1 year back. The patient underwent multiple treatments for the same like silicon gels, sheet but no good response. The general condition of the patient was normal. Cutaneous examination revealed ectropion 5 mm from the pupil when compared to the normal eyelid. There was a linear hypertrophic scar pulling the lid outward due to contracture extending on the left cheek diagonally down, causing an ectropion [Figure 1]. Scar revision was planned. The surgical profile was normal. The complete scar was excised [Figure 2], margins were undermined, and sutured with simple sutures using round-bodied 5.0 vicryl with complete lid reconstruction [Figure 3]. After a month, 70% of ectropion was corrected [Figure 4]. There remained a 2 mm pull on the lid. This was corrected by inserting two cogged monofilament threads with a builtin cannula from the temporal area to the left cheek just below the eyelid in the subcutaneous plane. Local anesthesia was given only at the entry point. Threads were pulled tight to adjust the remaining ectropion and cut [Figure 5]. The patient was asked to continue using moisturizer and silicone gel on the scar twice daily. There was a very good response in 3 months [Figure 6]. A sustained response was seen after 6 months [Figure 7]. The patient is still in follow-up.

- Traumatic ectropion with a scar on the cheek.

- Excision of the scar.

- Lid reconstruction.

- Mild ectropion remaining 1-month post-scar excision.
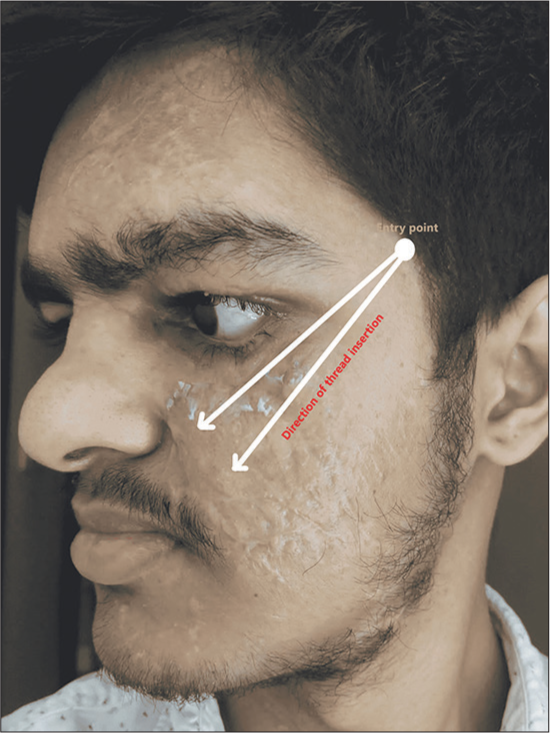
- The figure shows the entry point and the direction of threads.

- Good recovery post-polydioxanone threads.

- A sustained response was seen after 6 months.
DISCUSSION
A patient seeks scar revision for various reasons such as pain, itch, cosmetic appearance, and social stigma. It is important to note that scars take about 12–18 months to mature. Immature scars lead to poor results after a revision.2 Various modalities of ectropion correction are described earlier. Sharma and Georgolios mentioned Z-plasty as a common technique for distributing tension forces along a different axis that leads to the improvement of skin contractures and increased mobility of affected tissue. Two flaps are transposed along an axis, often using an angle of 60°, which results in a 75% gain in length and a 90° change in scar direction. The potential gain in scar length, the trapdoor effect, and bulging are a few disadvantages. Regional flaps such as rhomboid flap, bilobed rotational flap, paramedian forehead flap, and V to Y flap are also considered3 but are very complicated for everyone to do. The surgical management of cicatricial ectropion involving lengthening of the anterior lamella with transposition flaps and full-thickness free skin grafts (FTSG) taken from the preauricular area was suggested by Sidana and Kadam4. Chen et al. presented a novel surgical technique. The upper edge of the lower eyelid and associated scar tissue were excised. A modified Hughes flap was mobilized and secured above the posterior lamellar remnant. A full-thickness skin graft was placed over the flap. The flap was divided 4–5 weeks later.5 Transverse tarsotomy combined with a tarsoconjunctival flap is another modality effective for those who have failed surgery with traditional posterior lamellar spacer grafts, according to Cho.6 Baek et al. suggested the management of ectropion due to various reasons through medial and lateral canthopexy.7 Mitchell et al. described the use of hyaluronic acid (HA) injections for ectropion correction. Two injections of 0.2 mL and 0.3 mL of HA were injected subcutaneously below the ciliary margin above the orbicularis muscular plane into the lateral and medial lower left eyelid 1 week apart.1 However, this may not be useful in cicatricial cases. All the above techniques are complex, require great skills, and may lead to complications. Usage of threads may be helpful in such patients after simple excision to provide an upward pull avoiding major surgery and flaps. Thread lifting with polydioxanone (PDO) sutures is a cosmetic procedure where lax tissue is lifted and repositioned. The threads are absorbable and come in different shapes and lengths. The rate of complications and the downtime of the procedure are low, which is something patients are looking for. It is an addition to the armamentarium of plastic surgeons and dermatologists who can offer this option to their patients with improved outcomes.8 PDO threads are commonly used to lift facial skin that shows signs of aging, such as wrinkles and sagging, and to slim down the jawline, chronic facial palsy,9, and hair growth.10 Its usage in ectropion repair is not commonly reported. We introduce a novel and simple technique of scar excision and enhancing the result with PDO threads. This avoided the use of flaps or FTSG and resulted in improvement in lagophthalmos, exposure keratopathy, and very good esthetic appearance with eyelid ectropion correction and almost 80% improvement in the scar on the cheek.
Limitations
This method is used only in a single patient. Case series or studies are required to know the consistent use of threads in such ectropion patients.
CONCLUSION
Scar excision, along with PDO threads, could be an effective treatment modality for cicatricial ectropion, resulting in a better esthetic appearance and improving the quality of life of the patient, avoiding complicated flaps or full-thickness skin grafting.
Authors’ contributions
Varun Vishwanath: Concept, design, definition of intellectual content, literature search, clinical studies, data acquisition, data analysis, manuscript preparation, manuscript editing, manuscript review, guarantor. Ritu Vishwanath: Concept, design, literature search, data acquisition, manuscript preparation, manuscript editing, manuscript review, guarantor. Ramesh Vishwanath: Literature search, manuscript editing, manuscript review, guarantor
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Correction of cicatricial and involutional lower eyelid ectropion with hyaluronic acid. JAAD Case Rep. 2018;4:628-30.
- [CrossRef] [Google Scholar]
- Medial canthal reconstruction-scar restricting vision in only seeing eye of a 75-year-old female. World J Plast Surg. 2023;12:75-9.
- [CrossRef] [Google Scholar]
- Cicatricial ectropion of lower eyelid: A report of two cases. J Cutan Aesthet Surg. 2021;14:233-7.
- [CrossRef] [Google Scholar]
- A modified hughes flap for correction of refractory cicatricial lower lid retraction with concomitant ectropion. Ophthalmic Plast Reconstr Surg. 2020;36:503-7.
- [CrossRef] [Google Scholar]
- Correction of recalcitrant cicatricial lower lid retraction and entropion with transverse tarsotomy and tarsoconjunctival flap. Ophthalmic Plast Reconstr Surg. 2019;35:91-4.
- [CrossRef] [Google Scholar]
- Algorithm for the management of ectropion through medial and lateral canthopexy. Arch Plast Surg. 2018;45:525-33.
- [CrossRef] [Google Scholar]
- Use of polydioxanone threads as an alternative in nonsurgical procedures in facial rejuvenation. Facial Plast Surg. 2020;36:447-52.
- [CrossRef] [Google Scholar]
- F. Safety and efficacy of restoring facial symmetry using polydioxanone thread face lift technique in patients with facial palsy. J Clin Aesthet Dermatol. 2022;15:26-9.
- [Google Scholar]
- Monofilament threads in treatment of female hair loss. J Dermatolog Treat. 2021;32:521-5.
- [CrossRef] [Google Scholar]






