Translate this page into:
Nose Reconstruction Using Local and Regional Flaps: The Challenges and Advantages
Address for correspondence: Dr. Manjunath K N, Ramaiah Medical College, M. S. Ramaiah Nagar, MSRIT Post, Bengaluru 560054, Karnataka, India. E-mail: drknmanjunath@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
Nose is a central structure in midface. It has an important function in maintaining the aesthesis of the face. The three-dimensional (3D) structure of the nose is challenging to reconstruct. However, the availability of abundant vascularity and surrounding tissue is advantageous for the reconstruction of the soft tissue. Hence, this study was carried out to assess the cosmetic outcome and acceptability of patients undergoing nasal soft tissue reconstruction using local and regional flaps.
Materials and Methods:
Patients undergoing nasal soft tissue reconstruction using local or regional flaps, between January 2017 and December 2018, were studied. Patients requiring free flaps or skin grafts for reconstruction were excluded from the study. All the patients during follow-up at 3–6 months were asked to rate cosmetic acceptability and donor site cosmesis as bad, good, and very good.
Results:
In this study, 15 cases of nasal soft tissue reconstruction were studied. Among the 15 cases, 9 (60%) were male and 6 (40%) were female; the age range of patients was 7–65 years. Majority of the patients (5, 33.3%) had trauma as major cause of deformity. Post malignancy excision defect was the next major cause. All patients were happy with the results, only patient with composite graft complained regarding hyperpigmentation.
Conclusion:
Nose is an important structure in the midface. Apart from olfaction and respiration, maintaining adequate cosmesis is also an important function of the nose. Any deformity of the nose can be devastating to the patient. But, the 3D structure with varied structures makes reconstruction challenging to recreate. However, the availability of adequate donor tissue in local and surrounding region makes it advantageous. If principles of reconstruction are followed strictly, the outcome is good. Tissue expansion can be used whenever soft tissue requirement is more.
Keywords
Columella reconstruction
forehead flap
local and regional flaps
nasal reconstruction
nasal tip
INTRODUCTION
Nose is a central structure of the face. Olfaction and respiration are the primary functions of the nose. However, maintaining the structural integrity in itself is a major function. Any deformity of the nose is an aesthetic disaster. Nose is a three-dimensional (3D) structure, which projects beyond the plane of face. Any disfigurement is evident and has a huge impact on individual’s psychological health. Reconstructive options are skin grafts, local flaps, regional flaps, and free flaps.[1] All the reconstructive options have advantages and disadvantages. However, in the Indian subcontinent, the skin is less elastic and the scars are evident. Reconstruction with local or regional flaps is best suited for nasal soft tissue reconstruction. This study highlights the advantages of local and regional flaps and their outcome and acceptability in the patients.
MATERIALS AND METHODS
Between January 2017 and December 2018, all patients undergoing soft tissue reconstruction of the nose were included in the study. Patients requiring bony reconstruction or free flaps for soft tissue reconstruction were excluded from the study. Reconstruction was planned according to subunit principle. Donor flap was selected depending on the recipient site (defect) size and location. All patients were followed up at 3 and 6 months after wound healing. Patients are requested to rate the cosmetic outcome as very good (if the patient continued his/her routine without any concern such as scars), good (if the patient continued his/her routine with minor concerns such as scars), and bad (if patients had to change his/her routine and consulted for corrective surgery).
RESULTS
In this study, 15 cases of nasal soft tissue reconstruction were studied. Among the 15 cases, 9 (60%) were male and 6 (40%) were female; patients’ age range was 7–65 years. Majority of the patients (5, 33.3%) had trauma as the cause of deformity. Post malignancy excision defect was the next major cause [Table 1]. Depending on the size and location of the defect and following the subunit principles, local or regional flaps were planned. In one patient, composite graft was used for alar reconstruction, and rest all were reconstructed with local or regional flaps. In two patients, dorsal nasal flaps and bilobed flaps were used. In three patients, nasolabial flaps were used. Among the remaining seven patients, six were reconstructed using forehead flap and one using expanded forehead flap [Figure 1]. Of the 15 patients, 14 rated their cosmetic outcome as very good. One patient, who was reconstructed with composite graft, rated outcome as good, as parents were concerned with hyperpigmentation. All the patients were happy with results.
| Sl. no. | Age | Sex | Defect size (cm) | Etiology | Site |
|---|---|---|---|---|---|
| Composite graft | |||||
| 1 | 7 years | Female | 2 × 1 | Trauma | Ala |
| Dorsal nasal | |||||
| 2 | 45 years | Male | 2 × 2 | Trauma (bite injury) | Tip |
| 3 | 10 years | Female | 3 × 2 | Nevus | Tip |
| Nasolabial | |||||
| 4 | 70 years | Male | 3 × 2 | Basal cell carcinoma (BCC) excision | Ala |
| 5 | 65 years | Female | 1 × 2 | Trauma | Ala |
| Bilobed | |||||
| 6 | 26 years | Male | 1 × 1 | Nevus | Lateral |
| 7 | 35 years | Female | 2 × 1 | basal cell carcinoma | Lateral |
| 8 | 20 years | Female | 1 × 1 | Nevus | Lateral |
| Forehead | |||||
| 9 | 30 years | Male | 4 × 5 | Post burn | Tip/ala/dorsum |
| 10 | 20 years | Male | 4 × 3 | Arterio-venous Malformation | Tip/columella/ala |
| 11 | 26 years | Male | 5 × 3 | Trauma | Tip/dorsum |
| 12 | 65 years | Female | 3 × 3 | Carcinoma in situ | Dorsum |
| 13 | 65 years | Male | 4 × 5 | Melanoma | Dorsum |
| 14 | 30 years | Female | 4 × 4 | Trauma | Dorsum/tip |
| Expanded forehead | |||||
| 15 | 23 years | Male | 7 × 5 | Congenital nevus | Dorsum/nevus |
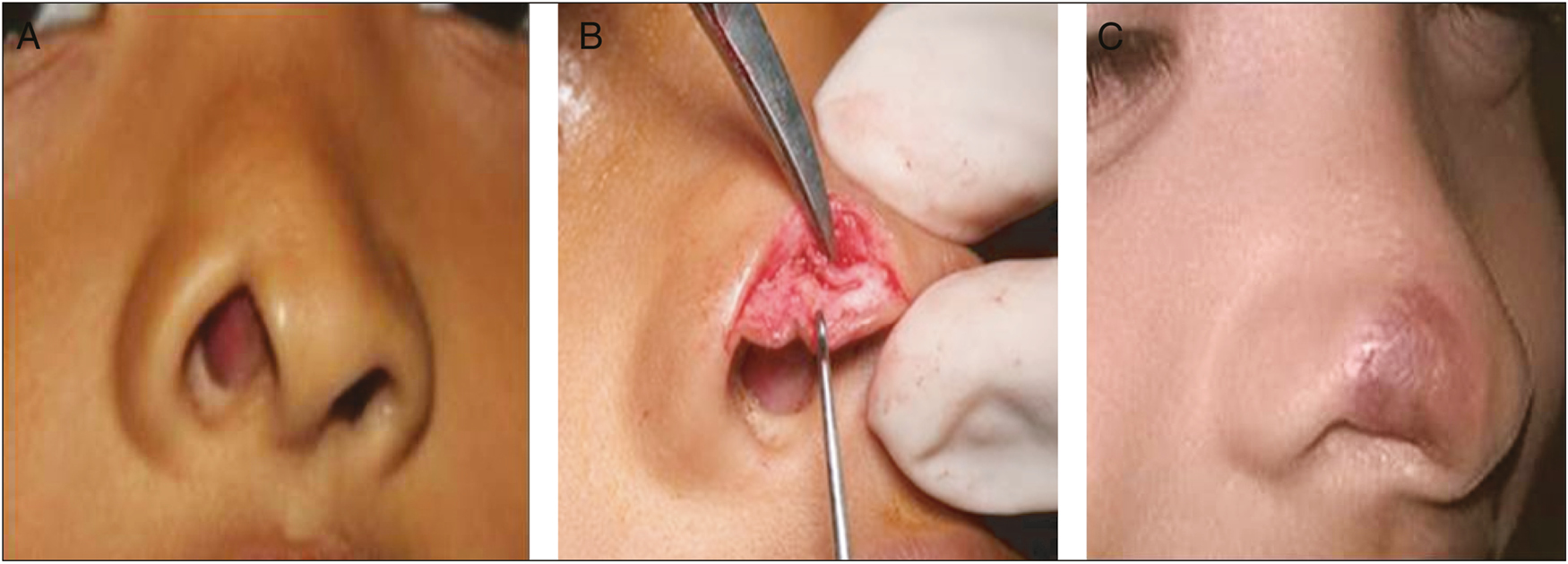
- (A) Post-cicatral alar defect. (B) Mucosa reconstructed by turndown flap. (C) After reconstruction with ear composite graft
DISCUSSION
Nose, being at the center of the face, has an important role in communication.[2] Reconstruction of mutilated nose is a challenging task as the nose is a 3D structure and projects from the plane of the face.[34] Structure of the nose is unique, as it has osteocartilaginous framework with mucosa[5] lining inside and skin lining outside. In any other structure, reconstruction would mean “simply to fill the defect,” however in case of the nose, filling the defect alone may lead to less optimal outcome. Nasal reconstruction needs meticulous planning. The two-dimensional defect sizes will not be the accurate measurement.[6] Subunits of the nose were described by Millard. He showed that wound closure at the junction of two subunits reduced scar.[78] However the principles of subunits reconstruction have evolved recently and modern techniques aim at building these subunits.[9] Margin of error is limited in these cases, as redoing or reconstructing a failed reconstruction is a herculean task.[5] Hence, choosing a best suited reconstructive option is of prime importance.
Composite grafts
Composite grafts are not a good choice for reconstruction as the uptake of the graft is very unpredictable. In Indian patients, the pigmentation, which develops post-graft uptake, is also disturbing. Also donor tissue available is less, and hence composite grafts can be used for very small defects. But it has advantages too, especially for an area where the cartilage is lost. In one case of a 7-year-old girl with post-traumatic full-thickness defect of the nose, including the mucosa, we used composite graft. In this case, mucosa was reconstructed using the turndown flap from the existing skin, and ala with cartilage was reconstructed with the composite graft harvested from the ear. The uptake was good and reconstruction healed well. But the patient was not happy with the cosmetic appearance. The skin had hyperpigmentation, which appeared like a scar. The patient had no problem with the donor site. Hence, she rated reconstruction as good [Figure 1A–C].
Dorsal nasal flap
Dorsal nasal flap by design is a rotation flap, which recruits excess of skin from the glabella and distally.[10] If it is performed for the proximal dorsal nasal region, it is called the glabellar flap, which rotates the glabellar skin. This flap can reach up to mid-nasal level.[11] These flaps should be elevated from the periosteum of the dorsum [Figure 2E] so that sufficient movement is achieved. The high vascularity of the base of the flap makes it a dependable flap for rotation.[12] However, the defects it covers are limited, as very less excess skin is available on the dorsum. The reach of the flap is till the tip of the nose. The lateral defects cannot be covered with these flaps. In our study, two patients had deformity of the tip, and recreating tip, which is convex in shape, was challenging. In both cases, tip was reconstructed recruiting the dorsal nasal skin. After healing, the end result was excellent, and the patients had a very good cosmetic acceptability. Donor-site scar was minimum and hardly visible in the front view [Figure 2A–D].
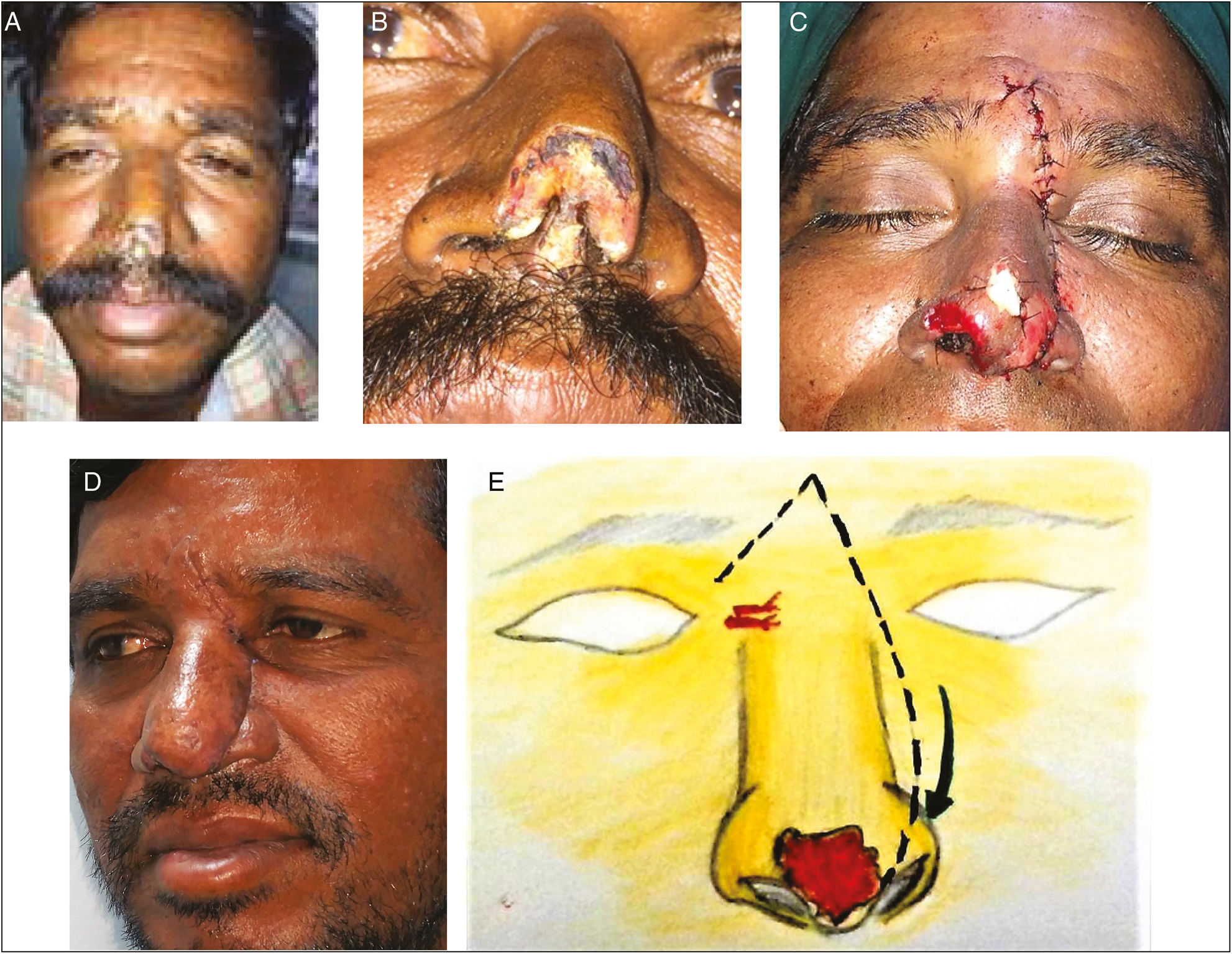
- (A) Post bite tip defect (far view). (B) Post bite tip defect (near view). (C) After immediate reconstruction with dorsal nasal flap. (D) Late picture after reconstruction. (E) Dorsal skin rotated to the tip
Bilobed flaps
Bilobed flaps are usually used for the defects on the lateral side of the nose. Geometrically, these flaps are double transposition, which are transposed on an axis at 45°C–50°C.[1314] The flaps are transferred such that the first flap covers the defect and the second flap covers the first flap donor site, and the donor site of the second flap is closed primarily using the laxity of the skin [Figure 3D]. Although the design can be used in any site, movement of the skin over the dorsum is an uphill task. So it can be used on defects on the lateral side.[151617] This flap is known for its best cosmetic results, but the donor site is limited and hence used for small defects only.[1819] In our study, the lateral defects of two patients were covered using bilobed flaps, both of them had excellent cosmetic results and minimal or no donor-site morbidity [Figure 3A–C]. Largest diameter of the defect was 2 cm, which was concurrent with other studies. Even other studies have opined that bilobed flaps are best for small defects. The greatest advantage of this flap is that the donor-site scar is on the lateral side and less conspicuous.
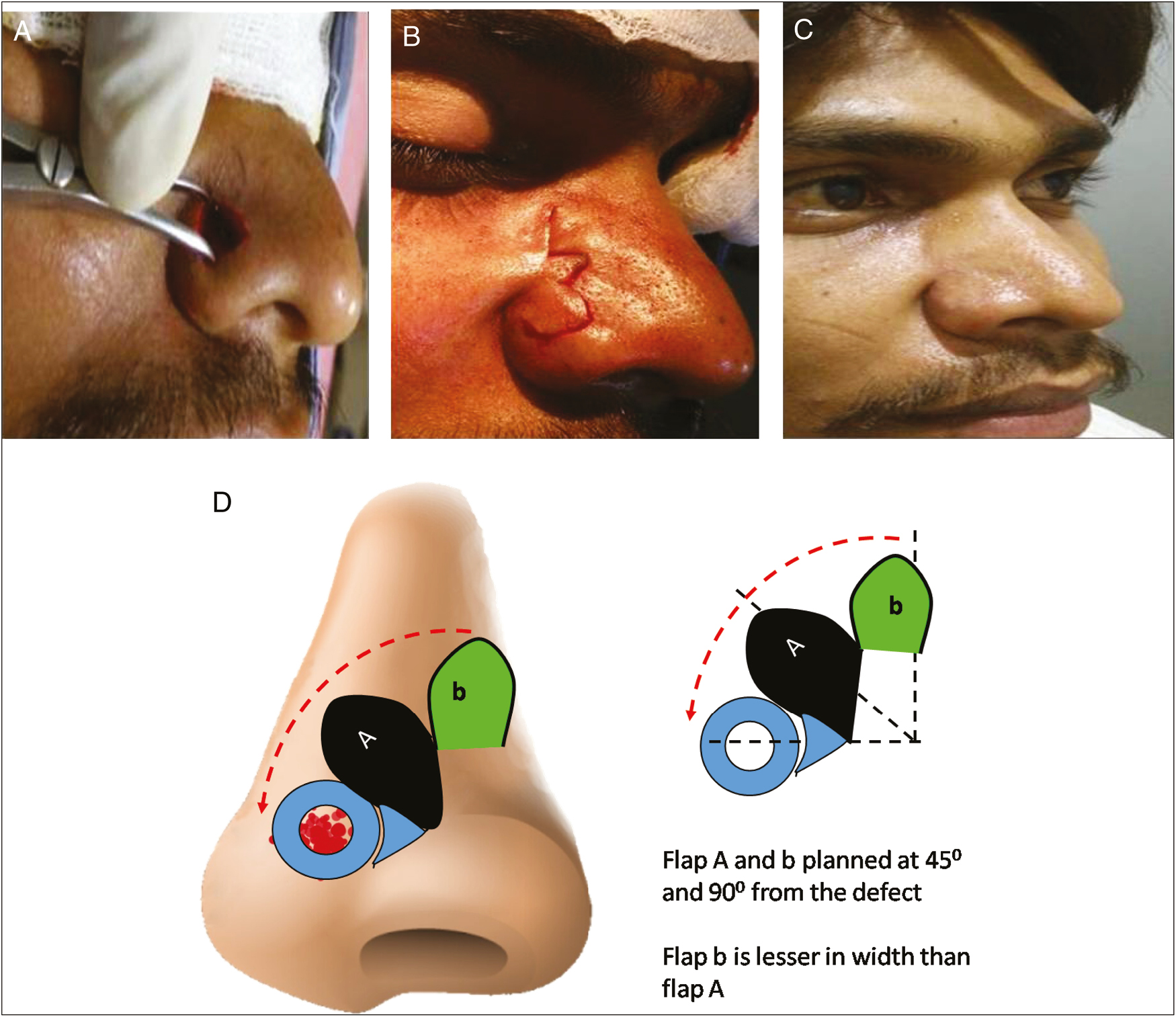
- (A) Post nevus excision defect over lateral side of the nose. (B) Bilobed flap planned. (C) After reconstruction. (D) Planning of bilobed flap
Nasolabial flaps
Nasolabial flap is an axial pattern flap based on the branches of facial artery, which can be elevated based on both cephalic and caudal branches of facial artery. These flaps can be designed as hatchet-Y advancement or as pedicled flaps.[120212223] The location and the reach of these flaps make them ideal for lower one-third of the nose. Ala of the nose has a round contour and is lined both from the outside and inside by skin. The skin is thick and has no subcutaneous tissue. The nasolabial skin matches all the requirements for ala or lower lateral nose reconstruction. After the transfer, the skin and the fat in the nasolabial region contracts resulting in rounded contour of the ala.[1924] Hence, it is best suited for the alar reconstruction. The donor site of the flap can be closed primarily leaving thin scar. Both our patients were old aged, hence the donor-site scar was minimum, and the reformed ala matched native nose very well [Figure 4A–D].
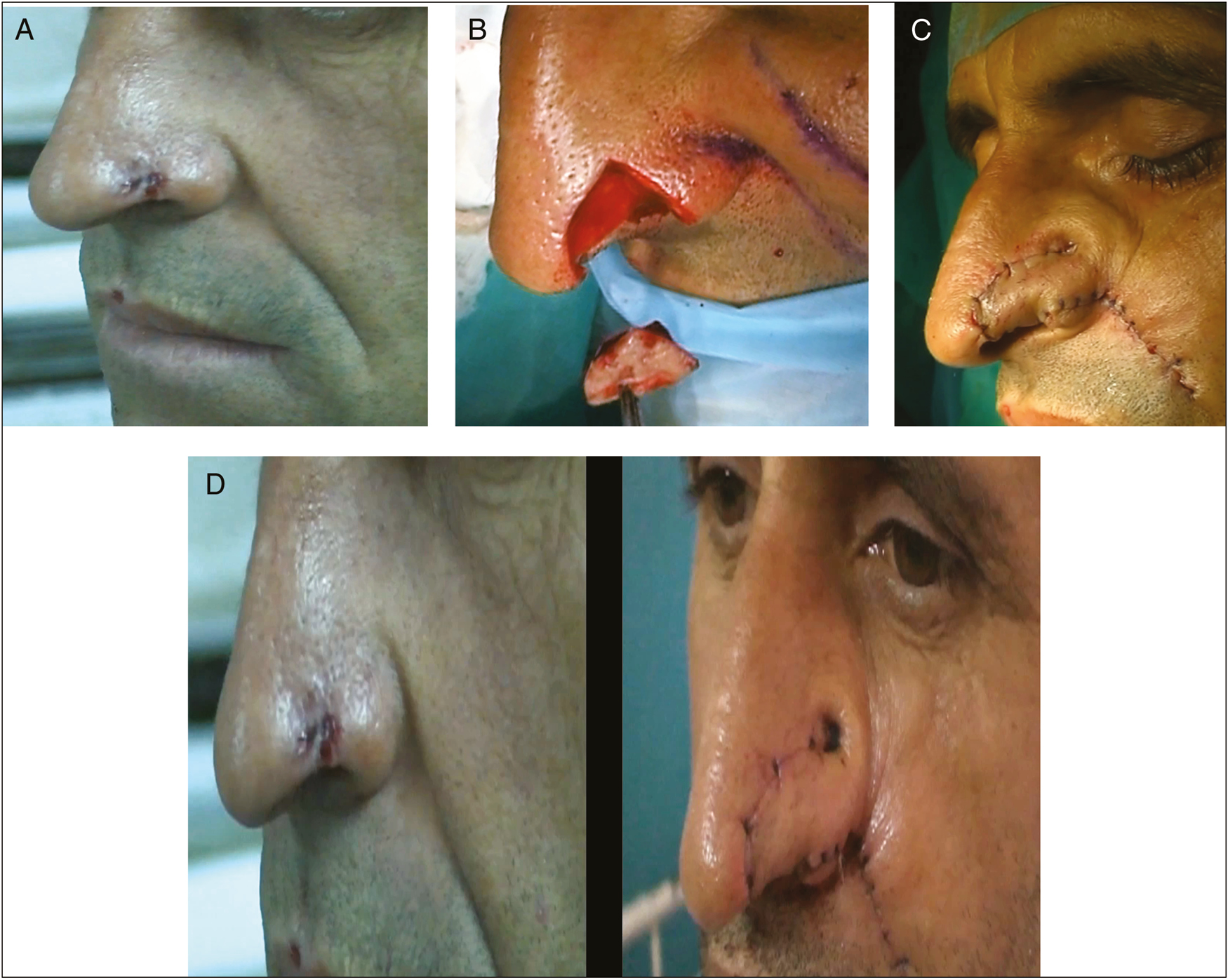
- (A) Basal cell carcinoma (BCC) of the ala. (B) Defect after the excision. (C) After immediate reconstruction with nasolabial flap. (D) Before and after reconstruction
Forehead flap
Whenever more than one subunit of the nose is lost, then donor site in the surrounding region is inadequate. Then the tissue from the forehead provides an excellent donor site. Forehead flap is an axial flap. This can be designed as oblique forehead (based on supratrochlear artery) or transverse flap (frontal branch of temporal artery). Skin of the forehead matches exactly to the skin of nose in color and texture.[2526] As the donor site is more, it can be used to cover the defects of the dorsum and the tip. By folding the distal end of the flap, it can be used to recreate the mucosal lining.[27] In conditions, where the osteocartilaginous frame needs to be reconstructed, prefabrication[28] of the flap along with the ear cartilage can be carried out. The disadvantage is the donor-site scar, which is visible on the forehead. Whenever the flap raised is more than 4 cm, skin graft is needed for closure. Majority of the times, it needs two stages to complete reconstruction. Majority of our patients required more than two subunit reconstruction. In all our patients, the donor site was closed primarily. Whenever more subunits are lost and requirement of the flap is more, then tissue expansion is used to cover both donor and recipient site effectively. One of our patients had congenital nevus over the nose and had discontinued college due to cosmetic embarrassment. We used tissue expansion [Figure 5A–D], to harvest large forehead flap. After reconstruction, the end result was very good and had huge impact on the psychology of the individual.
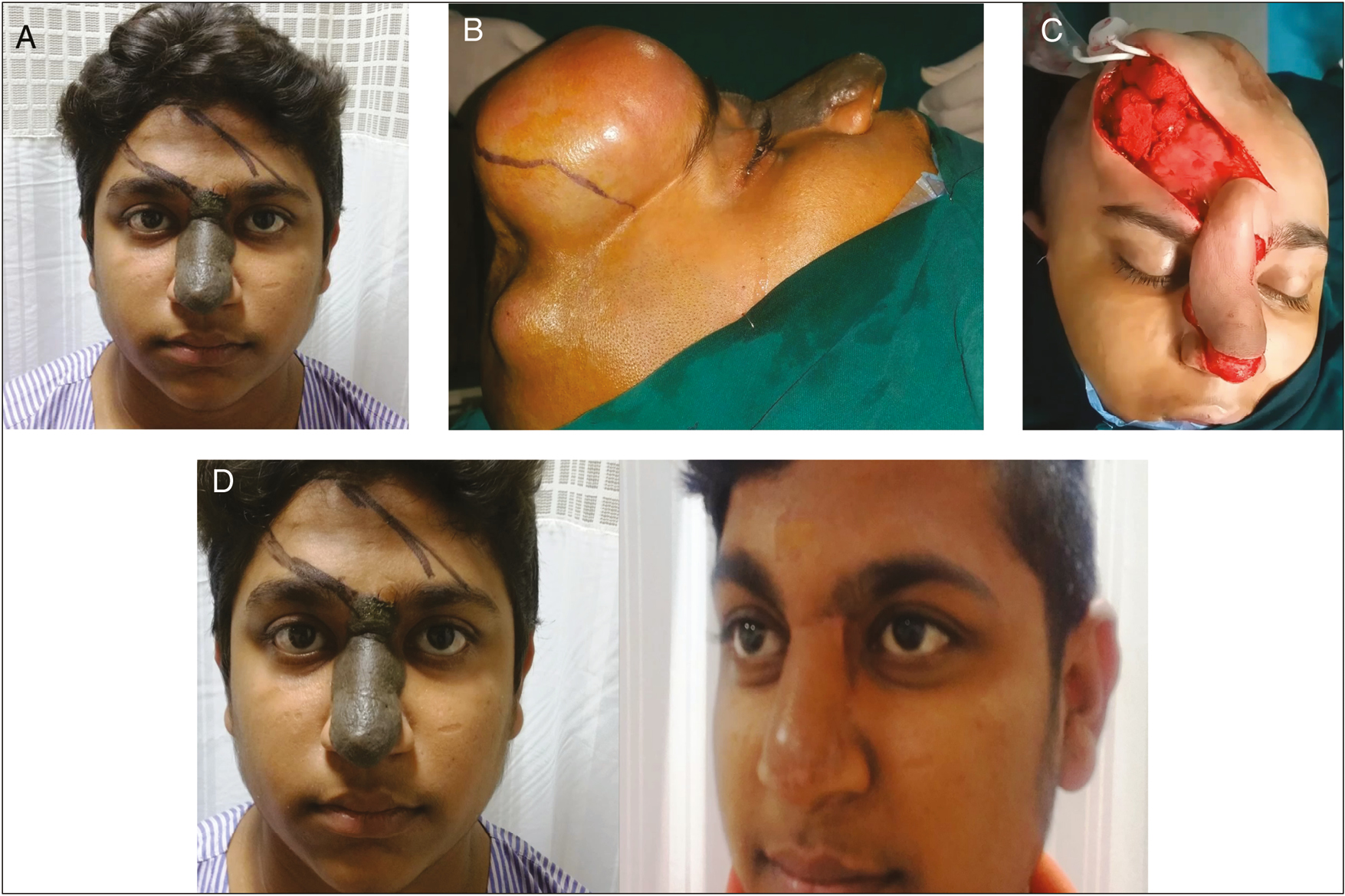
- (A) Hairy nevus involving whole nose. (B) Patient with fully expanded tissue expander in forehead. (C) Forehead flap elevated after expander removal. (D) Before and after reconstruction with expanded forehead flap
CONCLUSION
Nose plays an important role in an individual’s aesthesis. Reconstruction of the nose is a challenging task because of the 3D structure. Availability of highly vascular local and regional flaps is the biggest advantage. Tissue expansion is a useful tool whenever the flap requirement is more. If a principle of subunits is followed, the reconstruction can be gratifying both to the surgeons and the patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Nasal reconstruction: a simplified approach based on 419 operated cases. Aesthetic Plast Surg. 2015;39:91-9.
- [Google Scholar]
- Nasolabial flaps for nasal reconstruction: pros and cons. Turk J Plast Surg. 2018;26:151-5.
- [Google Scholar]
- Nasal reconstruction using the inferior turbinate mucosal flap. Arch Facial Plast Surg. 1999;1:97-100.
- [Google Scholar]
- The full-thickness forehead flap for complex nasal defects: a preliminary study. Otolaryngol Head Neck Surg. 2005;132:381-6.
- [Google Scholar]
- Nasal reconstruction: extending the limits. Plast Reconstr Surg Glob Open. 2016;4:e804.
- [Google Scholar]
- Defects of the nose, lip, and cheek: rebuilding the composite defect. Plast Reconstr Surg. 2007;120:887-98.
- [Google Scholar]
- Basal cell carcinoma in young women: an evaluation of the association of tanning bed use and smoking. J Am Acad Dermatol. 2002;46:706-9.
- [Google Scholar]
- The subunit principle in nasal reconstruction. Plast Reconstr Surg. 1985;76:239-47.
- [Google Scholar]
- Nonmelanoma skin cancer of the head and neck II: surgical treatment and reconstruction. Am J Otolaryngol. 2009;30:181-92.
- [Google Scholar]
- Reconstruction with dorsal nasal flap after excision of basal cell carcinoma of the nose. J Cutan Aesthet Surg. 2017;10:54-5.
- [Google Scholar]
- Nasal dorsal flaps. In: Baker SR, Swanson NA, eds. Local flaps in facial reconstruction (Chapter 14). St. Louis, MO: Mosby; 1995. p. :225-46.
- [Google Scholar]
- Nasal reconstruction with local flaps: a simple algorithm for management of small defects. Plast Reconstr Surg. 2008;122:130e-9e.
- [Google Scholar]
- StatPearls. Treasure Island, Florida: StatPearls Publishing; 2020. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470355/
- Reconstruction of nasal skin cancer defects with local flaps. J Skin Cancer 2011:181093. doi:10.1155/2011/181093, article ID
- [Google Scholar]
- Reconstruction of a surgical defect in the popliteal fossa: a case report. Int j Surg Case Rep. 2018;53:228-30.
- [Google Scholar]
- Use of local flaps for soft-tissue closure in diabetic foot wounds: a systematic review. Foot Ankle Spec. 2019;12:286-93.
- [Google Scholar]
- The differential use of bilobed and trilobed transposition flaps in cutaneous nasal reconstructive surgery. Plast Reconstr Surg. 2018;142:511-19.
- [Google Scholar]
- [The bilobed flap: a very efficient method in aesthetic reconstruction of small skin defects at the alar and tip regions of the nose] Ann Chir Plast Esthet. 2003;48:211-5.
- [Google Scholar]
- Modification of the Zitelli bilobed flap: a comparison of flap dynamics in human cadavers. Arch Facial Plast Surg. 2006;8:404-9.
- [Google Scholar]
- Superiorly based nasolabial interpolation flap for repair of complex nasal tip defects. Dermatol Surg. 2000;26:19-24.
- [Google Scholar]
- Nasolabial hinge flap with simultaneous cartilage graft in nasal alar and tip reconstruction. Dermatol Surg. 2007;33:476-83.
- [Google Scholar]
- Nasolabial flap for nasal tip reconstruction. Plast Reconstr Surg. 2008;122:775-81.
- [Google Scholar]
- Reconstruction of lower half defects of the nose with the lateral nasal artery pedicle nasolabial island flap. Plast Reconstr Surg. 2007;119:1767-72.
- [Google Scholar]
- Local flap in facial reconstruction (2nd ed). St. Louis, MO: Mosby; 2007.
- Three-dimensional nasal reconstruction using a prefabricated forehead flap: case report. Aesthetic Plast Surg. 2008;32:166-71.
- [Google Scholar]
- A modified bilobed flap design for nasal tip defects. Plast Aesthetic Res. 2014;1:16-20.
- [Google Scholar]
- Total nasal reconstruction: utility of the free radial forearm fascial flap. Arch Facial Plast Surg. 2003;5:159-63.
- [Google Scholar]






