Translate this page into:
Piercing Ear Keloid: Excision Using Loupe Magnification and Topical Liquid Silicone Gel as Adjuvant
Address for correspondence: Dr. Bellam Alagirisamy Ramesh, 2/F2, Eighth Street, Shanthi Nagar, Adambakkam, Chennai 600088, Tamil Nadu, India. E-mail: ramesh.ba@srimachandra.edu.in
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Keloid is an abnormal growth of scar at the site of skin injury, which usually does not regress. It proliferates beyond the original scar. The ear keloid usually develops after piercing injury to wear ornaments. A patient usually asks for removal of keloid, as it is aesthetically unpleasant. Patient may sometimes complain of itching and pain.
Aim:
The study was conducted to analyze results following excision of keloid with its tract and topical silicone gel as the postsurgical adjuvant.
Materials and Methods:
Ear keloids measuring less than 0.5cm or more than 5cm in maximum dimension were excluded from the study. Nonpiercing causes such as burns, trauma, and recurrent keloid were excluded from the study. The study was carried out on 22 patients who had keloid because of piercing injury, including 4 cases with both ear keloids. Of 26 ear keloids, 19 had the tract or connecting tissue. The lesion was excised under anesthesia using magnification. For all the operated cases, topical liquid silicone gel was used as postsurgical adjuvant therapy. The method of application of topical silicone gel was taught to each patient and was considered significant.
Result:
The magnification helped in identification of tract in 73% of the cases in this study. Twenty patients had successfully responded to proposed treatment, and two patients developed recurrence while using topical silicone gel as the adjuvant. These two patients were managed with conventional triamcinolone injection.
Conclusion:
The topical silicone gel as postsurgical adjuvant therapy avoided the use of painful postsurgical injection or radiotherapy for the 1–3cm primary ear keloids. The advantages of magnification were better clearance of keloid tissue, easier identification of tract and removal of keloid pseudopods, meticulous suturing, and comfortable elevation of a small local flap.
Keywords
Auricular keloid
local flap
loupe
needle injury
silicone
tract
INTRODUCTION
Keloid develops because of abnormal wound healing. The risk of development of keloid is higher in pigmented population.[1] The proposed etiology of keloid are genetic, hormonal, poor wound healing due to skin tension, inflammation, and infection.[2] The recent studies show peripheral region of keloid to be more active than the center.[3] The perilesional fibroblast is more active than intralesional fibroblast. These stimulate surrounding normal fibroblast to become keloidal fibroblast by its paracrine-secreting substances.[4] The study was based on this concept to excise keloid entirely from the margin. The aim was to remove all abnormal fibrous tissue with minimal loss of healthy tissue. The excision was achieved using loupe magnification. Usually piercing injury leads to the formation of a tract in the subdermal region.[5] The tract can be removed by magnification. After surgery, patients were prescribed topical liquid silicone gel as the adjuvant to prevent recurrence.
MATERIALS AND METHODS
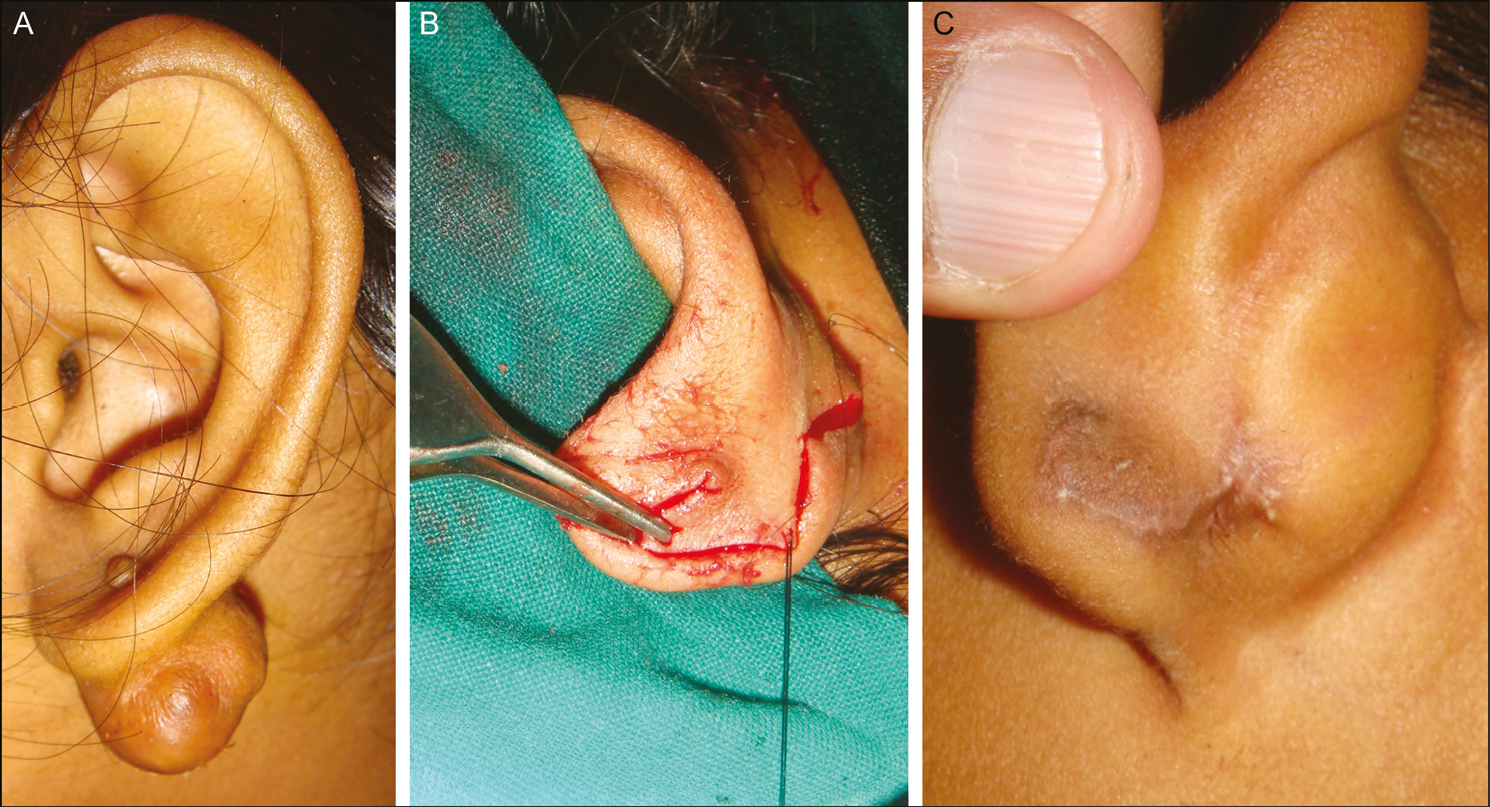
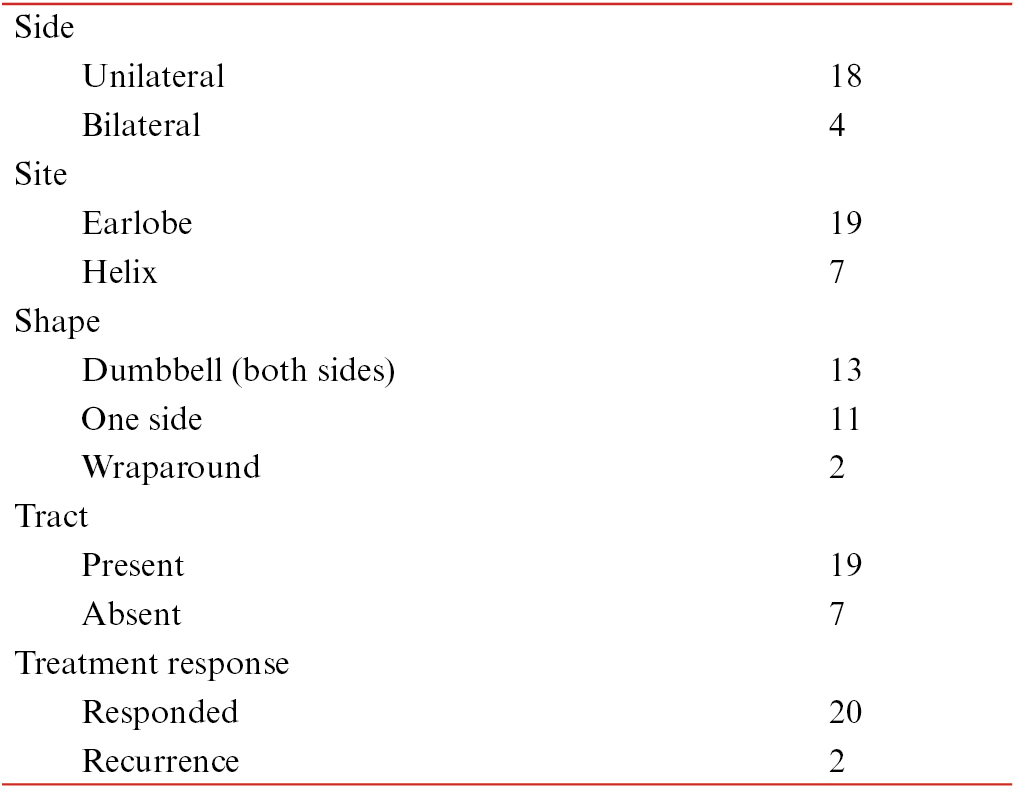
Only piercing primary ear keloid was included in the study. The large ear keloid (more than 5cm), recurrent keloid, and nonpiercing causes such as trauma and burns were not included in the study. The small ear keloids (less than 0.5cm) primarily treated with injection triamcinolone and silicone gel were not included in the study. Of 30 cases operated from January 2015 to June 2016, 22 cases available for follow-up were involved in the research [Table 1]. All the managed cases were females. The age of presentation was from 10 to 29 years in this study, except a patient who was 45 years old. The patient presented with a slow increase in the size of keloid, itching, and pain. The maximum size of anterior or posterior keloid in any of its plane without calculating interconnecting tract was recorded.
Surgical procedure
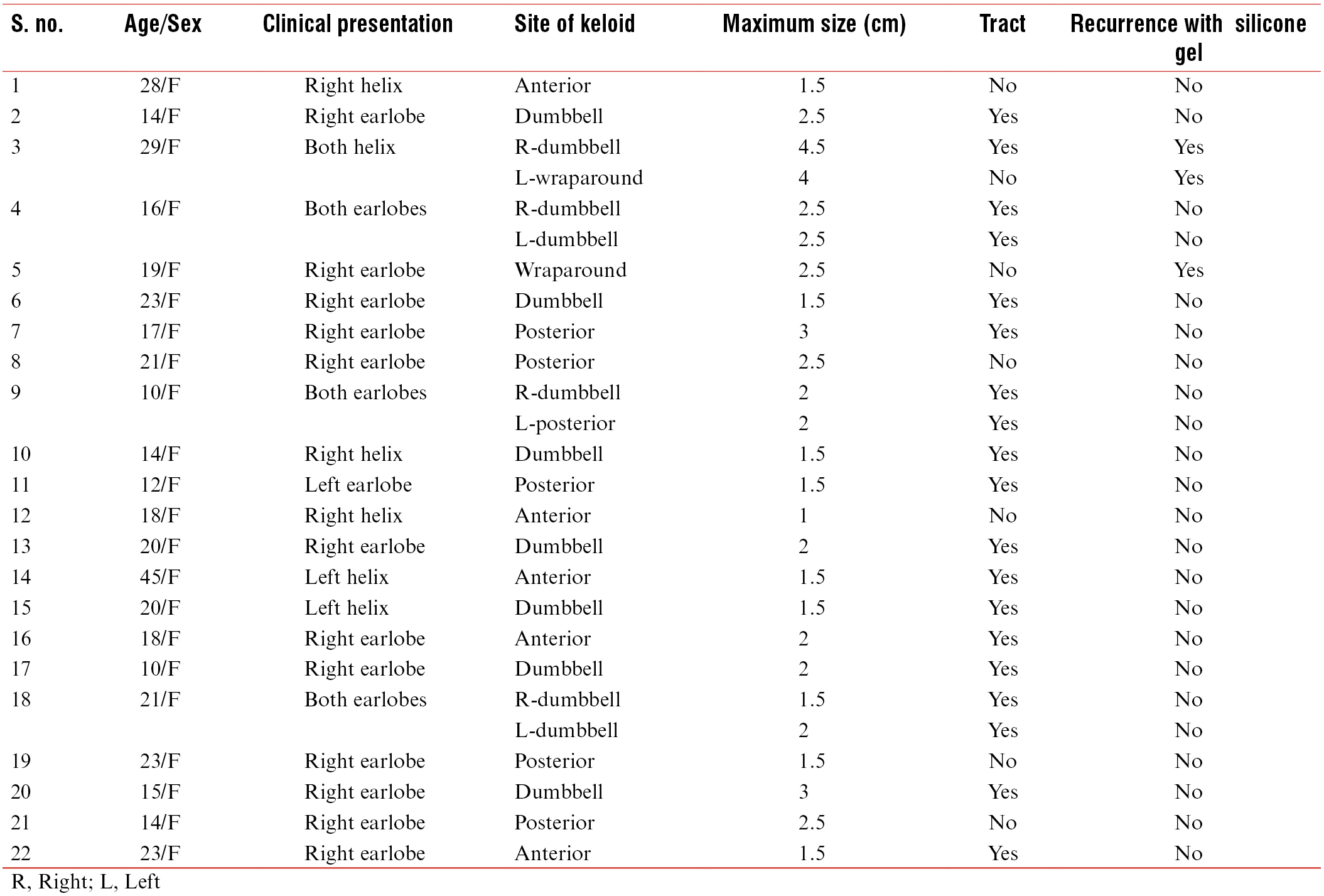
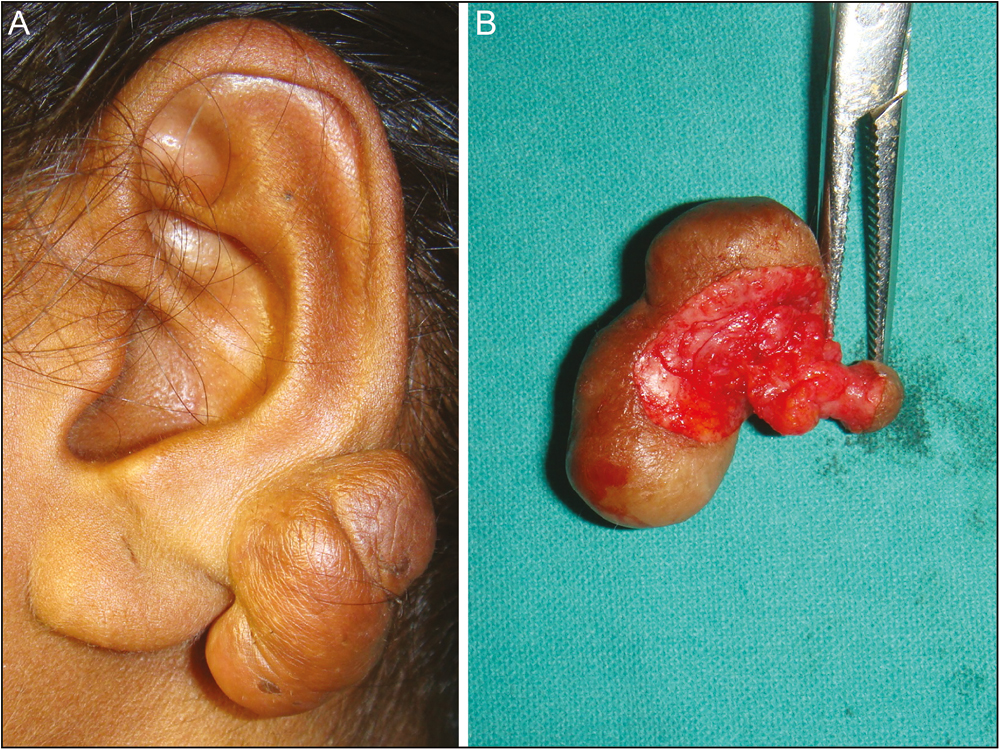
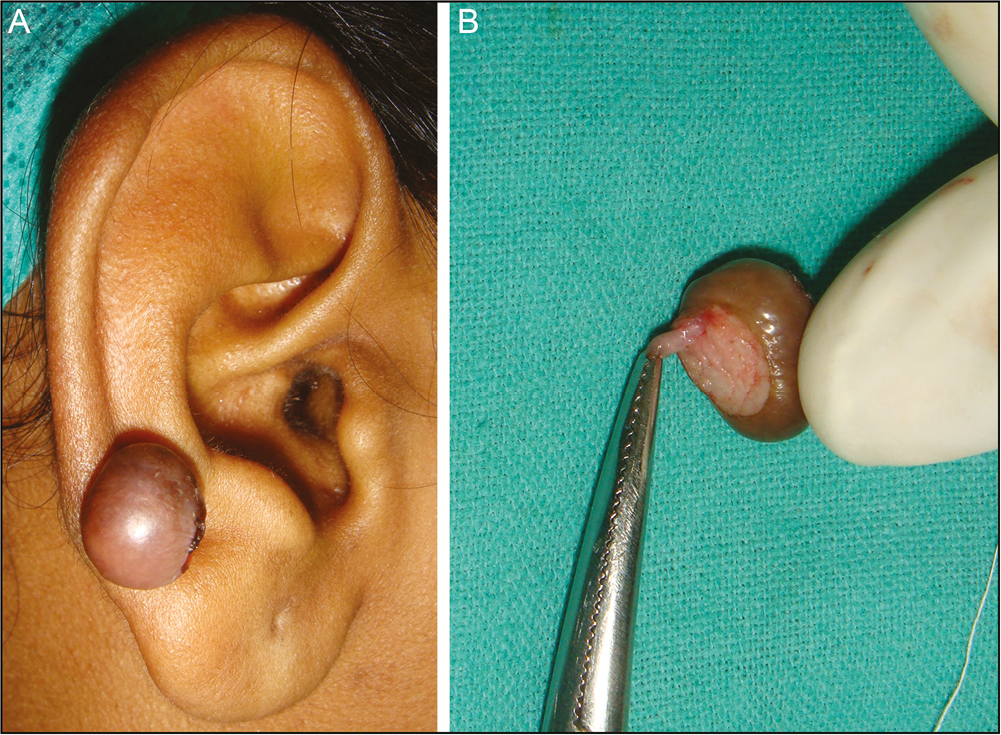
The ear was scrubbed with povidone-iodine, and local anesthetic 1% lignocaine was given at the appropriate site. The incision was made in the healthy tissue at the margin of the keloid. The dissection was carried out using 4× surgical loupe magnification, which identifies plane just outside the keloid. The dumbbell keloid with its connecting tissue (tract) was removed as a single entity [Figure 1A and B]. In anterior- or posterior-only ear keloid, the tract was identified by loupe magnification. The tract was either a conical mass from the base of keloid or a linear tissue emanating from the base of a keloid. The tract that was either fleshy or fibrous was removed [Figure 2A and B]. The use of magnification helped to remove any residual fingerlike processes of keloid tissue left on the wound. The removal of keloid with its tract on cartilaginous part of auricle sometimes needs coring of involved cartilage. Suturing was done with 5-0 monofilament nonabsorbable materials, without tension. If the initial approximation of wound edges produced suture line tension, local flap (commonly Limberg) was used to close the defect. The magnification further helps to do small local flaps better [Figures 3A–C and 4A–D].
- (A) Large dumbbell keloid. (B) Anterior and posterior keloid masses removed along with its connecting tissue (tract)
- (A) Ear keloid. (B) Fleshy tract completely removed using loupe magnification
- (A) Dumbbell keloid with large posterior mass. (B) Posterior defect covered with Limberg flap. (C) Ten months after surgery no recurrence
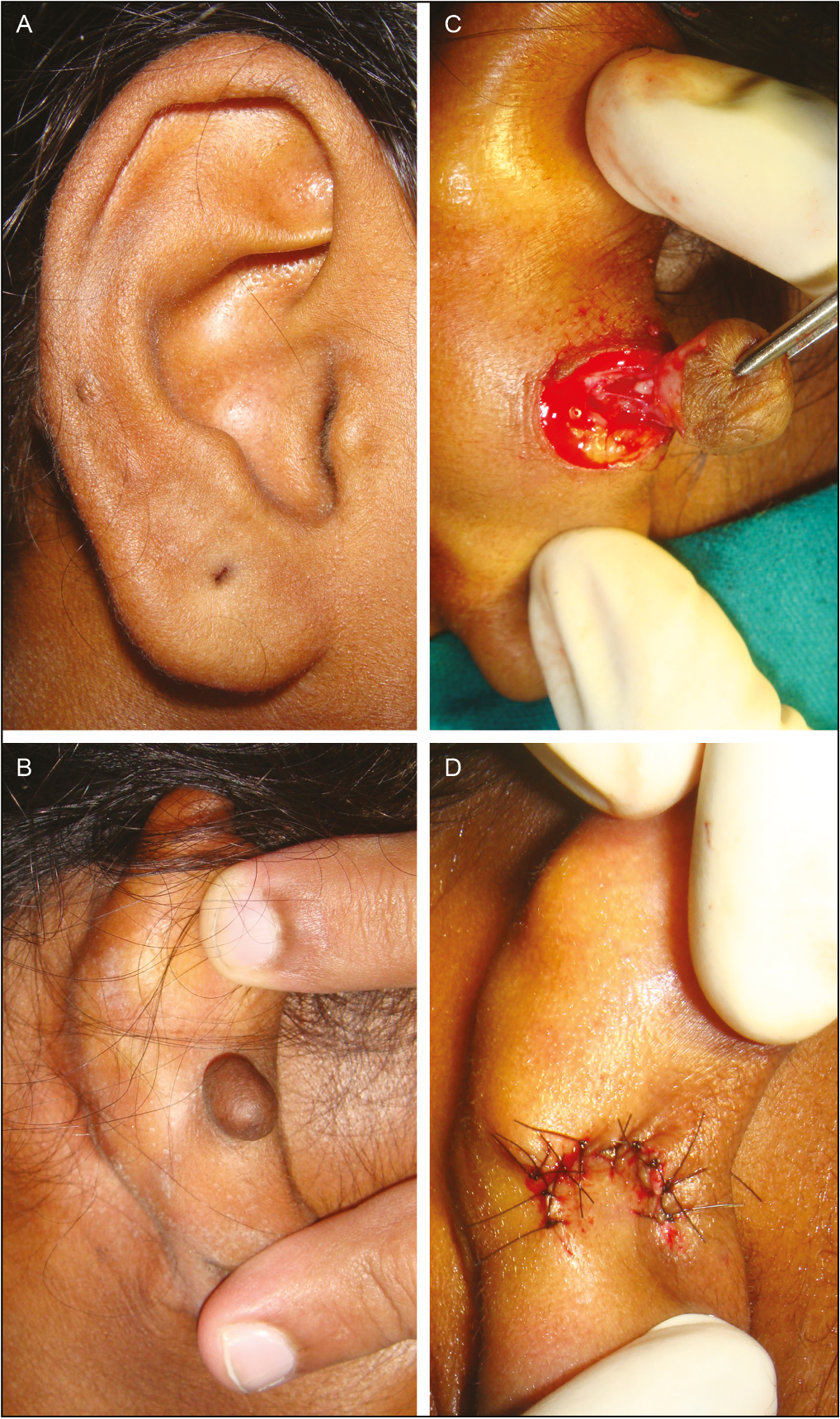
- (A) Anterior view piercing mark seen on helix. (B) Posterior view keloid ear helix. (C) Conical tract removed with keloid under magnification. (D) Defect covered with small Limberg flap to avoid notching deformity of helix
Patients were discharged after applying pressure dressing along with antibiotic and analgesic prescriptions. They were then advised the twice-daily application of antibiotic ointment to prevent infection for first 7 days. Sutures were removed on the 14th day of surgery. The postoperative adjuvant therapy was to use topical silicone gel twice daily from the third week after surgery and continued daily for 6 months. The method of application of topical silicone gel was taught to each patient. They were instructed to massage silicone gel on scar area for 5min twice daily. At the end of massage, excess silicone gel wiped off, so that thin film remains. During this treatment, if the keloid reappeared as nodularity, they were considered as nonresponsive to silicone gel. In nonresponsive cases, silicone gel treatment was stopped, and intralesional triamcinolone injection was started.[6] The injection triamcinolone 10mg/mL was given every 3 weeks for 6 cycles.
Patients were followed up every month for 6 months and then every third month for next 1 year. After 1.5 years of follow-up, if swelling reappeared, patient was asked to review. They are strictly advised to defer ear helix piercing forever. However, if patient insists to wear earrings on earlobe, the surgeon does the piercing after 1 year of surgery. Patients were also instructed to wear pure gold ornaments, as gold is the least reactive element.
RESULTS
Eighteen patients had single ear keloid. Four patients presented with both ear keloids. Hence, the total number of ear keloids operated was 26. Keloid was present in earlobe in 19 cases and in helical part of the ear in 7 cases. Nine instances presented as dumbbell keloid on one ear and two cases on both ears. Two cases had the wraparound keloid. The loupe magnification dissection identified the root or connecting tissue in 19 (73% of piercing ear keloid) of 26. The operated specimen was subjected to histopathological examination. The report was keloid in all the cases. The tract was said to contain granuloma in eight cases. Of 22 patients (90%), 20 responded to proposed treatment and did not develop recurrence at 1.5 years of follow-up. Two cases, including one patient with both ear keloids, did not respond to silicone gel [Tables 1 and 2]. The unresponsive cases in this study were wraparound keloids and keloid size of 4cm or more. These two patients had intralesional triamcinolone injection and did not develop recurrence. Patients were followed up every month for 6 months and then every third month for next 1 year. After 1.5 years of follow-up, they were suggested to review when swelling reappears.
DISCUSSION
Keloids are characterized by their continued growth following trauma and extension into healthy tissue. The keloid may grow up to 1 year after injury. It does not regress on its own. Simple surgical excision without adjuvant therapy causes recurrence.[7] The extralesional excision of keloid mass with its tract (active perilesional keloid fibroblast removed) may help to avoid recurrence.[6]
Earlobe keloids are classified as minor keloids according to the international clinical recommendation on scar management.[89] They cause cosmetic deformities, itching, pain, and psychological distress to the patient.[10] The typical age of presentation is between 10 and 30 years.[11] The common size of ear keloid when presented to surgeons is 1–3cm. The common cause of ear keloid is piercing injury.[12] The entity of ear piercing keloids is unique when compared with other reasons. The ear is usually pierced with a sharp instrument passed through earlobe or helix. Hence, there is an injury to the skin on one side with a penetrating subdermal fat or cartilage injury and injury to surface on opposite side. Scarring develops on both sides of the ear and in between soft tissue. The piercing effect tends to form keloid tissue on anterior, posterior, or both surfaces with a connecting tract. The dumbbell keloid is a classical presentation of piercing injury. The dumbbell keloid has a tract connecting anterior and posterior keloid masses. They are treated by complete excision of both keloid masses with its tract.[1314] If only anterior or posterior keloid is present, there is still a tract or root going inside soft tissue. It is either fibrous or fleshy. The use of magnification facilitates removal of root and surrounding keloid pseudopods with less removal of surrounding fat. Minimal removal of surrounding tissue helps in tension-free closure after keloid excision. If tension is still present, smaller flaps with less deformity to the ear can meticulously be done with magnification. The extraction without magnification may result in significant loss of healthy tissue, leading to higher chance of ear deformity after suturing, tension along suture line, or a larger flap to cover the defect.
Keloid formation is often considered to be the result of a persistent inflammation, prolonged proliferative phase of wound healing, and delayed remodeling phase of wound healing.[1516] Apart from ornaments, persistent inflammation might be because of foreign bodies such as dirt getting inside by piercing injury. The tiny foreign body can get deposited along the tract. The histopathology of tract shows granuloma in 8 of 19 cases in our study. The removal of tract helps in clearing persistent inflammatory cause of keloid because of a microscopic foreign body.
A healing wound can become an unsightly scar during the remodeling phase.[171819]
A keloid has normal epidermis, a tonguelike advancing edge, a horizontal fibrous band in the upper reticular dermis, prominent fascia like a band, and keloidal collagen.[20] The perilesional or peripheral region of keloid has abundant T-cell lymphocytes[21] and increased collagen production.[322] The collagen bundles are thicker in keloid than the hypertrophic scar or normal scar.[23] Silicone gel modifies the abnormal remodeling phase of wound healing in keloid. The proposed mechanisms of action of silicone gel are the reduction of wound-site tension,[24] hydration,[25] downregulating fibroblast, and altered fibrogenic cytokines.[2627] The study uses topical silicone gel as an adjuvant for preventing recurrence of the keloid.[28] The adjuvant prevented recurrence in 20 (90% of patients) of 22 patients operated in this study. The liquid silicone gel is a useful method to overcome the difficulties of applying silicone gel sheet on an irregular surface.[29] The prolonged application up to 6 months or 1 year is useful in keloid patients as their remodeling phase of wound healing is longer. The method of application of topical silicone gel is critical. Twice daily circular motion massaging is to be done for 5min on the ear keloid excised region. At the completion of massage, a thin film remains on the surface. Topical silicone gel is easy to apply and cosmetically acceptable.[3031] The cases that did not respond to silicone gel were either wraparound or more than 4-cm-sized keloids in this study. In our opinion, silicone gel avoids series of painful postoperative injection and hence provides better patient compliance. The various postsurgical adjuvant treatments may be reserved for cases not responding to topical liquid silicone gel. Excellent results by excision and postoperative radiotherapy are shown in multiple studies.[123233] The problem is the availability of radiation in all centers and management of its complications. Surgical removal combined with radiotherapy may be reserved as a last resort in the treatment of therapy-resistant keloids.[34]
CONCLUSION
Piercing earlobe keloids need to be considered differently from other keloids, as they have a tract. This study shows a good response after complete surgical excision and postsurgical topical liquid silicone gel as adjuvant therapy for 1- to 3-cm-sized earlobe keloid. Magnification ensures complete removal of pseudopods of keloid tissue and its tract. It also helps to do meticulous suturing. Tension-free closure of wound may require small local flaps. With the use of silicone gel, patient may not need radiotherapy or painful postsurgical intrascar injections. Adjuvant therapy is needed for cases not responding to silicone gel treatment in 1- to 3-cm-sized keloids, wraparound keloids, and more than 4-cm-sized keloids.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
REFERENCES
- Molecular dissection of abnormal wound healing processes resulting in keloid disease. Wound Repair Regen. 2010;18:139-53.
- [Google Scholar]
- Fibroblasts from the growing margin of keloid scars produce higher levels of collagen I and III compared with intralesional and extralesional sites: Clinical implications for lesional site-directed therapy. Br J Dermatol. 2011;164:83-96.
- [Google Scholar]
- Site-specific keloid fibroblasts alter the behaviour of normal skin and normal scar fibroblasts through paracrine signalling. PLoS One. 2013;8:e75600.
- [Google Scholar]
- The efficacy of complete surgical excision of keloid and piercing sinus tract on earlobe keloid. Ann Dermatol. 2013;25:370-3.
- [Google Scholar]
- Investigation of the influence of keloid-derived keratinocytes on fibroblast growth and proliferation in vitro. Plast Reconstr Surg. 2001;107:797-808.
- [Google Scholar]
- Hypertrophic scars and keloids: Etiology and management. Am J Clin Dermatol. 2003;4:235-43.
- [Google Scholar]
- International Advisory Panel on Scar Management. International clinical recommendations on scar management. Plast Reconstr Surg. 2002;110:560-71.
- [Google Scholar]
- International Advisory Panel on Scar Management. Updated international clinical recommendations on scar management: Part 2—algorithms for scar prevention and treatment. Dermatol Surg. 2014;40:825-31.
- [Google Scholar]
- Relationship between age of ear piercing and keloid formation. Pediatrics. 2005;115:1312-4.
- [Google Scholar]
- Analysis of the surgical treatments of 63 keloids on the cartilaginous part of the auricle: Effectiveness of the core excision method. Plast Reconstr Surg. 2015;135:868-75.
- [Google Scholar]
- Keloids of the earlobes: A surgical technique. J Dermatol Surg Oncol. 1983;9:552-6.
- [Google Scholar]
- Cutaneous tissue repair: Basic biologic considerations. I. J Am Acad Dermatol. 1985;13:701-25.
- [Google Scholar]
- Histopathological differential diagnosis of keloid and hypertrophic scar. Am J Dermatopathol. 2004;26:379-84.
- [Google Scholar]
- Biological differences between fibroblasts derived from peripheral and central areas of keloid tissues. Plast Reconstr Surg. 2007;120:625-30.
- [Google Scholar]
- Differences in collagen architecture between keloid, hypertrophic scar, normotrophic scar, and normal skin: An objective histopathological analysis. Wound Repair Regen. 2009;17:649-56.
- [Google Scholar]
- The tensile reduction effects of silicone gel sheeting. Plast Reconstr Surg. 2010;126:109e-11e.
- [Google Scholar]
- Hydration, not silicone, modulates the effects of keratinocytes on fibroblasts. J Surg Res. 1995;59:705-11.
- [Google Scholar]
- Silicone sheeting decreases fibroblast activity and downregulates TGFbeta2 in hypertrophic scar model. Int J Surg Investig. 2001;2:467-74.
- [Google Scholar]
- The effect of silicone gel on basic fibroblast growth factor levels in fibroblast cell culture. Arch Facial Plast Surg. 2004;6:88-93.
- [Google Scholar]
- Silicone gel sheeting for the prevention and management of evolving hypertrophic and keloid scars. Dermatol Surg. 1995;21:947-51.
- [Google Scholar]
- A useful method to overcome the difficulties of applying silicone gel sheet on irregular surfaces. Int Wound J. 2015;12:185-8.
- [Google Scholar]
- The efficacy of silicone gel for the treatment of hypertrophic scars and keloids. J Cutan Aesthet Surg. 2009;2:104-6.
- [Google Scholar]
- Prevention of postsurgical scars: Comparison of efficacy and convenience between silicone gel sheet and topical silicone gel. J Korean Med Sci. 2014;29:S249-53.
- [Google Scholar]
- Postoperative radiation protocol for keloids and hypertrophic scars: Statistical analysis of 370 sites followed for over 18 months. Ann Plast Surg. 2007;59:688-91.
- [Google Scholar]
- Combined surgical excision and radiation therapy for keloid treatment. J Craniofac Surg. 2007;18:1164-9.
- [Google Scholar]
- The results of surgical excision and adjuvant irradiation for therapy-resistant keloids: A prospective clinical outcome study. Plast Reconstr Surg. 2007;119:2248-54.
- [Google Scholar]






