Translate this page into:
Platelet-rich fibrin therapy in the management of nonhealing trophic ulcers due to underlying leprous neuropathy
*Corresponding author: Shekhar Neema, Department of Dermatology, Armed Forces Medical College, Pune, Maharashtra, India. shekharadvait@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Vendhan S, Neema S, Vasudevan B, Krishnan L, Gera V. Platelet-rich fibrin therapy in the management of nonhealing trophic ulcers due to underlying leprous neuropathy. J Cutan Aesthet Surg. 2024;17:262-5. doi: 10.4103/JCAS.JCAS_192_22
Abstract
Autologous platelet-rich fibrin (PRF) therapy is beneficial in the treatment of nonhealing ulcers. We present a case series of nonhealing, trophic ulcers with underlying leprous neuropathy, treated successfully with PRF therapy. It was a prospective study, conducted in a tertiary care hospital in the western Maharashtra, India between April 2021 and March 2022. A total of 11 patients with 18 nonhealing trophic ulcers were included in the study and consisted of 8 men and 3 women. The patient’s median age was 41 years (range, 33–68), the median size of the ulcers was 4 cm2 (range: 1–12 cm2), the median duration of ulcers was 20 weeks (16–30 weeks), and time to heal after starting treatment was 4 weeks (range: 1–8 weeks). PRF is an easy-to-use, simple, safe, effective, and economical treatment for the management of trophic ulcers.
Keywords
Hansen disease
Leprosy
Nonhealing ulcer
Platelet rich fibrin
PRF
Treatment
Trophic ulcer
INTRODUCTION
Nonhealing ulcers are described as spontaneous or traumatic lesions that do not improve even after 3 months of consistent treatment or that persist despite receiving the necessary care and do not progress toward healing within a specified time frame.1 Nonhealing ulcers have diverse etiologies such as venous, arterial, traumatic, and neuropathic or trophic ulcers. Other uncommon causes are hematological conditions and infectious diseases. Leprosy can result in trophic ulcers even after complete treatment due to the persistence of sensory neuropathy. These ulcers cause significant disability, affect the activity of daily living, reduce earning potential, and have a negative impact on the quality of life.2 Autologous platelet-rich fibrin (PRF) therapy is beneficial in the treatment of nonhealing ulcers.3 Here, we present data on a group of 11 patients who underwent PRF treatment for the trophic ulcers associated with leprous neuropathy.
MATERIALS AND METHODS
This prospective study was conducted in a tertiary care dermatology center during the study period from April 2021 to March 2022, after obtaining clearance from the institutional ethical committee. Patients suffering from leprosy presenting with trophic ulcers of more than 12 weeks duration were included in the study. Patients less than 18 years, pregnant and lactating women, anticoagulant and antiplatelet therapy, and concomitant illness causing nonhealing ulcers such as diabetes mellitus were excluded from the study. Each patient underwent a thorough history, examination, and relevant investigations including a radiograph of the affected area to rule out osteomyelitis and a surface swab and culture for infection. Appropriate antibiotics were prescribed before the initiation of PRF treatment. The ulcer’s length, breadth, and depth were measured and documented with tracing paper and photographs. In accordance with the size of the ulcer, ten to twenty milliliters of venous blood were collected in an anticoagulant-free vacutainer and promptly centrifuged for eight minutes at a speed of 3000 rpm under stringent aseptic conditions. Following centrifugation, three layers were obtained: upper platelet-poor plasma, middle PRF, and lower red blood cells (RBCs). The ulcer was cleaned and debrided, if necessary. The PRF was separated and placed on a piece of sterile gauze, the RBC tail was removed using a sterile blade and PRF was placed over the ulcer bed. Three-layered bandaging was done and the process was repeated every week till complete healing. Off-loading of the affected limb was advised to all the patients. The ulcer outline was marked on the transparent sheet and the area was calculated at each visit using a graph paper overlying the transparent sheet. Serial images of the ulcer were captured.
RESULTS
The study included 11 patients (8 men and 3 women) with 18 nonhealing ulcers; the median age of the patients was 41 years (range, 33–68) and the median duration of the ulcer was 20 weeks (range, 16–30 weeks). The median size of the ulcers was 4 cm2 (range: 1–12 cm2), and the median time for ulcer to heal was 4 weeks (range: 2–8 weeks) [Figures 1 and 2]. The site and size of each ulcer is mentioned in Table 1. Two patients received antibiotics due to positive culture on the surface swab. There was no adverse effect noticed with PRF treatment. During the 6-month follow-up period, none of our patients had ulcer recurrence.

- Trophic ulcer on left great toe shows complete healing after six platelet-rich fibrin (PRF) dressing done weekly.
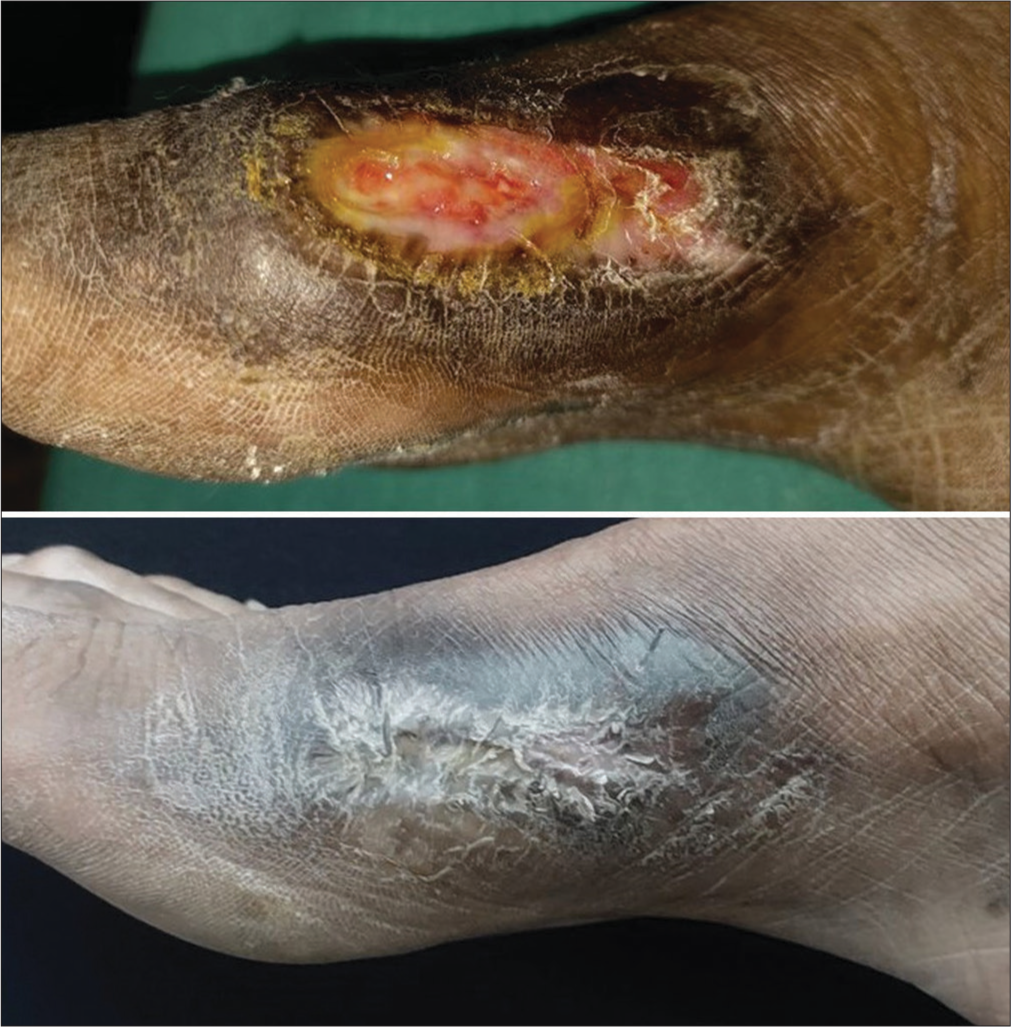
- Trophic ulcer over medial aspect of right foot shows complete healing after four platelet-rich fibrin (PRF) dressing done weekly.
| Sr. no. | Age (in years) | Gender | Site of ulcer | Size of the ulcer at first visit cm2 | Time to heal (weeks) |
|---|---|---|---|---|---|
| 1 | 37 | M | Dorsum of foot | 3.14 | 6 |
| 2 | 34 | F | Sole of foot | 2 | 6 |
| 3 | 39 | M | Sole of foot | 6 | 8 |
| 4 | 43 | M | Sole of foot | 12 | 5 |
| 5 | 54 | M | Sole of foot | 3 | 4 |
| 6 | 62 | M | Lateral malleolus | 1 | 1 |
| 7 | 41 | M | Sole of foot | 4 | 4 |
| 8 | 33 | F | Hand | 12 | 5 |
| 9 | 68 | M | Sole of foot | 4 | 6 |
| 10 | 64 | M | Sole of foot | 4 | 4 |
| 11 | 38 | F | Hand | 4 | 6 |
M: Male, F: Female
DISCUSSION
Wound healing is a complex process and consists of three stages such as inflammation, proliferation, and maturation.4 Chronic wounds exhibit decreased levels of epidermal growth factor, fibroblast growth factor, transforming growth factor-beta, platelet-derived growth factor, and vascular endothelial growth factor. The exact treatment of nonhealing ulcers depends on etiology and various treatments are used for their treatment such as different kinds of dressing, debridement, growth factors, negative pressure wound therapy, electromagnetic stimulation, or hyperbaric oxygen therapy to name a few. Nonhealing trophic ulcers frequently do not respond well to the traditional ulcer care techniques of dressing and debridement.
Platelet-rich plasma (PRP) is an autologous blood product that contains high concentration of platelets and a supraphysiological amount of growth factors, that has been utilized for the management of nonhealing ulcers. The PRP has to be injected into the wound and release growth factors on activation after coming in contact with the tissue.5 Suthar et al.6 used PRP in 24 patients with chronic nonhealing ulcers; the ulcers healed in median duration of 8.2 weeks. Although PRP is beneficial in chronic nonhealing ulcers, it has certain disadvantages. This paved the way for the development of PRF, a second- generation platelet concentrate that does not require injection and releases growth factors slowly. This slow release of growth factors over a period of 10 days and three-dimensional fibrin scaffold supports cell migration and stimulates tissue regeneration effectively. The preparation of PRF is an easy, one-step process and does not require anticoagulants, as compared to PRP.
Nagaraju et al.7 used weekly PRF in seven patients with nonhealing trophic ulcers with underlying leprous neuropathy and noticed complete healing by 5 weeks in all patients. Another study by Dorjay et al.8 used PRF for nonhealing ulcers of various etiology and found the mean time to heal was 5 weeks (range, 3–9). Dohan Ehrenfest et al.9 found that PRF was more effective than PRP in treating nonhealing ulcers.
A variety of growth factors, including platelet-derived growth factor, transforming growth factor beta1, vascular endothelial growth factor, and insulin-like growth factors, are released by PRF. In addition, PRF contains several cytokines and matrix glycoproteins such as thrombospondin 1, fibronectin, and vitronectin. PRF can be used as a tissue graft for cutaneous wounds since it functions like living tissue. The high concentration of leukocytes in PRF increases effectiveness by reducing the risk of infections.10 PRF is a safe, effective, and economical treatment for the management of trophic ulcers.
Authors’ contributions
All the authors contributed to the research study. Senkadhir Vendhan: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review. Shekhar Neema: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review. Biju Vasudevan: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review. Lekshmipriya Krishnan: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review. Vinay Gera: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Efficacy and safety of autologous platelet rich plasma for the treatment of vascular ulcers in primary care: Phase III study. BMC Fam Pract. 2014;15:211.
- [CrossRef] [PubMed] [Google Scholar]
- Selection of appropriate wound dressing for various wounds. Front Bioeng Biotechnol. 2020;8:182.
- [CrossRef] [PubMed] [Google Scholar]
- Cascade® autologous system platelet-rich fibrin matrix in the treatment of chronic leg ulcers. Adv Wound Care (New Rochelle). 2012;1:52-5.
- [CrossRef] [PubMed] [Google Scholar]
- Inflammation. 2: Its role in the healing of chronic wounds. J Wound Care. 2002;11:245-9.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of concentrated autologous platelet-derived growth factors in chronic lower-extremity wounds. J Am Podiatr Med Assoc. 2006;96:482-8.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of chronic nonhealing ulcers using autologous platelet rich plasma: A case series. J Biomed Sci. 2017;24:16.
- [CrossRef] [PubMed] [Google Scholar]
- Autologous platelet-rich fibrin matrix in nonhealing trophic ulcers in patients with Hansen's disease. J Cutan Aesthet Surg. 2017;10:3-7.
- [CrossRef] [PubMed] [Google Scholar]
- Platelet-rich fibrin in nonhealing leg ulcers: A simple and effective therapeutic option. J Cutan Aesthet Surg. 2021;14:160-5.
- [CrossRef] [PubMed] [Google Scholar]
- Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part II: Platelet-related biologic features. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e45-50.
- [CrossRef] [PubMed] [Google Scholar]
- The role of leukocytes from L-PRP/L-PRF in wound healing and immune defense: Newperspectives. Curr Pharm Biotechnol. 2012;13:1153-62.
- [CrossRef] [PubMed] [Google Scholar]






