Translate this page into:
Post sclerotherapy lower lip reconstruction with dermofat graft and labial advancement flap
*Corresponding author: Taruna Singh, Department of General Surgery, All India Institutes of Medical Sciences, Rishikesh, Uttarakhand, India. taruna1209@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Vathulya M, Singh T, Behl R, Pasricha A. Post sclerotherapy lower lip reconstruction with dermofat graft and labial advancement flap. J Cutan Aesthet Surg. 2025;18:23-6. doi: 10.25259/jcas_162_23
Abstract
Sclerotherapy has been commonly used for the treatment of arteriovenous (AV) malformation as a stand-alone technique or with surgical excision of the nidus. However, it can cause surrounding tissue necrosis and scarring. The lip is one of the most uncommon sites for AV malformation. Lip esthesis is of paramount importance. Hence, its reconstruction becomes a difficult task due to its specialized nature. In our technique, we have combined a labial mucosal advancement flap to reconstruct a scarred lip with dermofat grafting to provide an acceptable contour. Therefore, we have combined the principles of reconstruction of the lip with the aesthetic domain in a single stage to replicate a pinkish-red, smooth, and pliable lip with a pout.
Keywords
Arteriovenous malformation
Buccal mucosa advancement flap
Dermofat graft
Lip
Sclerotherapy
PROBLEM STATEMENT
Sclerotherapy is one of the management protocols for arteriovenous (AV) malformation.1 It has been used as a stand-alone technique or in combination with surgical excision to completely eradicate the nidus of AV malformations. It is indicated in lesions that are increasing in size, causing cosmetic disfigurement and dental malalignment. Although this management results in a decrease in the size of the lesion, in some cases, it can lead to severe cosmetic disfigurement and scarring due to necrosis, which is seldom addressed.2
Lips are specialized muscular tissues covered with a smooth, pinkish-red mucosa. Their function includes competence and articulation. Lip esthesis is of paramount importance, and the ultimate goal is lip deformity correction and reconstruction resulting in a pliable smooth pinkish-red lip with a pout.
In this case, we address one such post-sclerotherapy lower lip sequelae surgically managed with dermofat graft and buccal advancement flaps with a satisfactory outcome.
RECOMMENDED SOLUTION
A 15-year-old presented with a severely scarred lower lip following sclerotherapy for lower lip malformation. She had swelling over the lower lip region since childhood which caused disfigurement of the lower lip. She had undergone four sessions of foam sclerotherapy with sodium tetradecyl sulfate. After that, she developed scarring on her lower lip with an uneven texture [Figure 1]. She underwent a scar excision at a local hospital but was unsatisfied with the results. Her main concern was the flattening of the lower lip with pitted and scarred lower lip mucosa. Pre-operative ultrasound ruled out the recurrence of arteriovenous malformation. Under general anesthesia, the scar involving the vermilion border was removed, preserving the orbicularis oris muscle. The excision was done according to the extent of the deep scar. Some fibrotic bands traversing the orbicularis oris were also released to give the lip more pliability. This technique involved raising labial mucosal flap advancement from the free border (posterior border of the excised scar defect) of the labial advancement flap was made and the redundancy of the labial mucosa near its junction with gingiva was used to advance it to resurface the defect [Figure 2a and b]. Resurfacing was done intraoperatively by covering the mucosal raw area of the excised scar region with a buccal advancement flap along with a sandwiched dermofat graft underneath to cover the entire thickness of the vermilion of the lower lip [Figure 2b]. The new dry lip vermillion border was sutured to the skin border using proline 5–0 [Figure 3]. Dermofat graft harvested from the groin [Figure 4] was threaded into a tunnel below the mucosal advancement flap and remnant muscular fibers using a suction steel introduction metal tip after the mucosal flap had been sutured in place [Figure 5]. The result was a smooth, pink-colored lower lip with a natural pout. The following photograph is 6 months post-operative [Figure 6]. The patient followed up after nearly two years of surgery, which shows a well-healed lip. We can also see the underlying muscle tone with a smooth contour of the lip and the luster of the lip regained as compared to the previous lusterless scarred lip [Figure 7]. A photograph of the patient taken after two and a half years of surgery shows good results [Figure 8].

- Pre-operative photo.
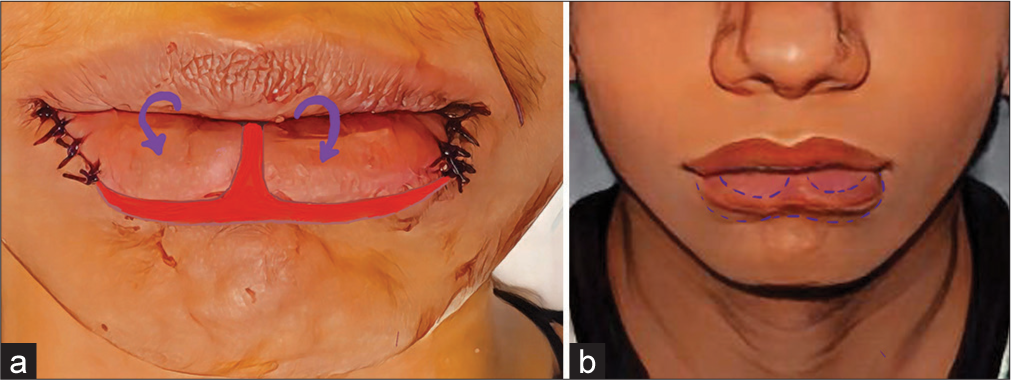
- (a) Arrow points to the advancement of labial mucosal flap (b) shows the out turning of the mucosal flap advanced into the defect.

- Excision of scar and suturing to skin border.

- Dermofat graft.

- Dermofat threaded into the tunnel under mucosal advancement flap

- Clinical photograph after 6 months post-operatively.

- Post-operative lower lip (after two-year follow-up).

- Clinical photographs after two and a half years of surgery.
Discussion
The lip is a rare site for AV malformation. Treatment modalities include sclerotherapy, pre-operative embolization, and surgical resection.3 However, these managements can have complications and cause disfigurement of facial landmarks and hemorrhage, which makes their management difficult. The lip is a specialized tissue comprised of keratinized stratified squamous epithelium that overlies a highly vascular bed of tissue that gives the lips their rosy hue.4 The end goal of reconstruction is a cosmetically appealing lip. Lip augmentation has been described earlier by autologous fat grafting to reconstruct.5 In our case, we have combined reconstructive and esthetic domains in a single stage to give a natural and esthetically pleasing lip [Figure 6].
Conclusion
We, the authors, propose this single-staged technique of buccal mucosal advancement flap resurfacing along with dermofat grafting for such complex lip deformities to produce a satisfactory lip esthesis. One can see that this technique has combined both the reconstructive and esthetic domains of plastic surgery.
Authors’ contributions
All the Authors have contributed to the research study. They have contributed in data collection, consent and picture collection, drafting of manuscript, editing of manuscript and follow up of the patient.
Ethical approval
The research/study approved by the Institutional Review Board AIIMS/IEC/24/305, 21st June 2024.
Declaration of patients consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Incidence of major complications from embolosclerotherapy of head and neck vascular malformations in a single specialist centre. Vascular. 2022;30:952-9.
- [CrossRef] [PubMed] [Google Scholar]
- Arterio-venous malformation: How much do we know? Phlebology. 2009;24:193-200.
- [CrossRef] [PubMed] [Google Scholar]
- Arteriovenous malformation of the oral cavity. Case Rep Dent. 2014;2014:353580.
- [CrossRef] [PubMed] [Google Scholar]
- Arteriovenous malformation of the lip: A rare case report. Cureus. 2020;12:e8979.
- [CrossRef] [Google Scholar]
- Permanent lip augmentation with serial fat grafting. Ann Plast Surg. 1999;42:376-80.
- [CrossRef] [PubMed] [Google Scholar]







