Translate this page into:
Should high BMI of transmasculine patients prevent them from masculinizing their chest walls?
*Corresponding author: Lakshmi Venkata Simhachalam Kutikuppala, Department of General Surgery, Dr NTR University of Health Sciences, Vijayawada, Andhra Pradesh, India. simhachalam.kutikuppala@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kutikuppala LVS, Kuchana SK, Chintala JS, Boppana SH. Should high BMI of transmasculine patients prevent them from masculinizing their chest walls? J Cutan Aesthet Surg. 2025;18:131-2. doi: 10.4103/JCAS.JCAS_194_22
Dear Editor,
Chest wall masculinization is one of the familiar procedures used to serve the transition from female to male (FtM). Transmasculine patients typically have excess skin thickness, larger breast volumes, and presence of chest ptosis.1 Patients with high BMI have heavier and large breasts, making them more difficult to survive as a man. Many of these people have used breast binding to hide their breasts. Nevertheless, this can escalate the skin elasticity, necessitating excess skin excision during future chest masculinization. Because a large fraction of FtM individuals is obese, the early surgical access during their transition of gender affirmation can help with satisfaction and cosmesis. High body mass index (BMI) is regarded as a connection to the poor outcomes following the chest masculinization surgery.2 In spite, there is no proper evidence to support, people with a BMI greater than 30 kg/m2 have been denied this surgical procedure historically. When compared to other weight classifications, patients with a higher BMI had a higher incidence of wound dehiscence. The known relation between chest scarring and larger breast size is understandably the most concerning aspect of the chest masculinization among the obese individuals.3
Access to proper medical care for transgender people must be greatly simplified and the weight need not be a barrier for having the surgical approach to chest masculinization. Mastectomy could be performed securely in obese FtM patients for chest wall masculinization, while the interconnection between breast volume and obesity raises concerns about increased scarring and poor esthetic outcomes making the rates of acute or sudden complications comparable [Figure 1].2,4,5 The “hockey stick” incision comprising of free nipple grafts (FNGs) may dampen gender dysphoria in transgender men by reconstructing a cis- masculine appearing chest. “Hockey stick” incision is made up of two incisions horizontally, one at the infra- mamillary fold (horizontalized medially) and one at the overlapping of the horizontal incision line superiorly above the upper limit of the nipple-areolar complex. Findings of a study by Junn et al. indicated that this approach is an effective and safe technique for chest masculinization, specifically in patients with ptotic and moderate to large breast tissue and high BMI who achieve gender congruence with cis-masculine models.6 Furthermore, the “hockey stick” technique provides comparable better clinical outcomes and patient satisfaction to types of periareolar incision and FNGs.6
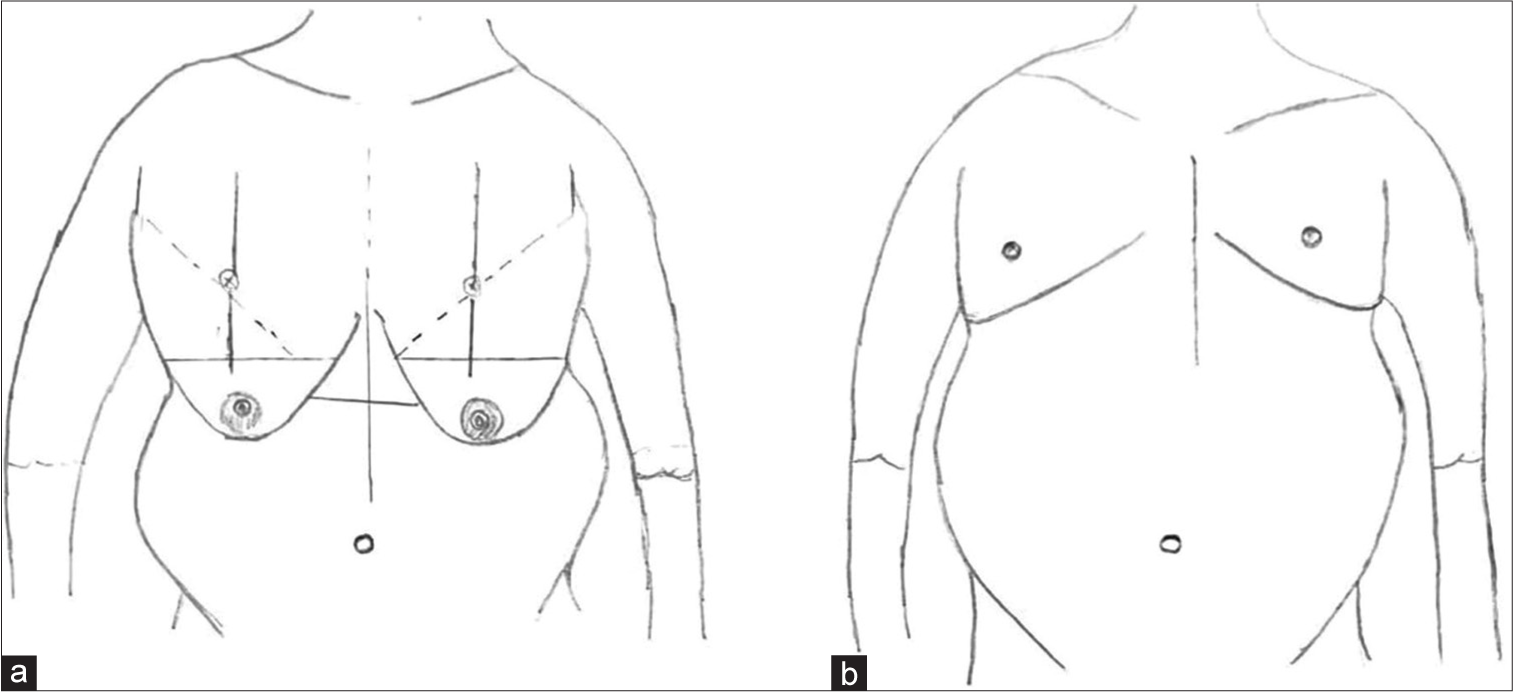
- Mastectomy of an obese female to male (FtM) transgender patient performed with a transverse incision and free nipple-areolar complex grafts: (a) Preoperative planning and (b) postoperative result.
Authors’ contributions
All the authors contributed to the research study. Lakshmi Venkata Simhachalam Kutikuppala: Concepts, design, definition of intellectual content, literature search, manuscript preparation, manuscript editing, and manuscript review. Sai Kiran Kuchana: Concepts, design, definition of intellectual content, literature search, manuscript preparation, manuscript editing, and manuscript review. Jyothi Swaroop Chintala: Concepts, design, definition of intellectual content, literature search, manuscript preparation, manuscript editing, and manuscript review. Sri Harsha Boppana: Concepts, design, definition of intellectual content, literature search, manuscript preparation, manuscript editing, and manuscript review.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Incidence of complications in chest wall masculinization for the obese female-to-male transgender population: A case series. World J Plast Surg. 2021;10:14-24.
- [CrossRef] [PubMed] [Google Scholar]
- Chest-wall contouring surgery in female-to-male transgender patients: A one-center retrospective analysis of applied surgical techniques and results. Scand J Surg. 2017;106:74-9.
- [CrossRef] [PubMed] [Google Scholar]
- Chest surgery in female to male transgender individuals. Ann Plast Surg. 2017;78:249-53.
- [CrossRef] [PubMed] [Google Scholar]
- Gender-affirming surgery for transgender individuals: Perceived satisfaction and barriers to care. Plast Surg (Oakv). 2018;26:263-8.
- [CrossRef] [PubMed] [Google Scholar]
- Female-to-male gender-affirming chest reconstruction surgery. Aesthet Surg J. 2019;39:150-63.
- [CrossRef] [PubMed] [Google Scholar]
- Hockey stick incision: A modified technique for chest wall masculinization. Ann Transl Med. 2021;9:600.
- [CrossRef] [PubMed] [Google Scholar]





