Translate this page into:
Successful management of an unusual hypopigmented scar after surgical repair of a unilateral Tessier 7 cleft
Address for correspondence: Dr. Kriti Jain, Department of Oral and Maxillofacial Surgery, Faculty of Dental Sciences, SGT University, Chandu-Budhera, Gurugram-Badli Road, Gurugram 122505, Haryana, India. E-mail: jain.kriti@gmail.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Tessier No. 7 cleft is the most common atypical craniofacial cleft with an incidence of 1:3000–5642 births. This clinical report describes the successful management of a delayed, unusually hypopigmented postoperative facial scar following the surgical closure of a Tessier 7 cleft using the Pfeiffer wave line incision. In the absence of any other associated systemic lesions, the scar was treated as a localized leucoderma. The scar coloration improved dramatically with the chosen line of conservative medical treatment, and a surgical revision was not required. This report highlights the need for continuous follow up despite seemingly good short-term results. The medical management of the hypopigmented scar will aid fellow practitioners who may face similar dilemmas.
Keywords
Hypopigmentation
leucoderma
macrostomia
pfeiffer incision
tessier 7
Hypopigmented scars that appear postoperatively can be quite disconcerting for both patients and clinicians alike; especially when they appear on the face. This report highlights the use of a non-invasive treatment that proved to be successful within a short span of time.

INTRODUCTION
Tessier No. 7 is the most common among the rare craniofacial clefts with an incidence between 1:3000 and 1:5642 births.[1] It is commonly associated with syndromes such as hemifacial microsomia and Treacher Collins syndrome. The spectrum of clinical presentation varies from a pre-auricular skin tag to a complete otomandibular dysostosis.[2] Usually, a wide oral aperture with loss of commissural anatomy is observed.[3]
Macrostomia has been treated using multiple techniques with three primary goals: myoplasty, commissuroplasty, and skin and buccal mucosal closure of the excised cleft. Skin closure techniques have employed straight-line closures, Pfeiffer incisions, Z-plasties, W-plasties, transposition flaps etc. Post-operative complications include hypertrophic, contracted, and hyper- or hypopigmented scars that may adversely affect aesthetic and functional outcomes; contractures with commissural migration that compromises oral competence; and inadequate orbicularis myoplasty that results in a ‘‘goldfish mouth deformity.’’[45]
This report describes the clinical course of a patient who underwent unilateral Tessier 7 cleft repair using the Pfeiffer wave line incision. The postoperative scar showed an unusual, delayed hypopigmented appearance and was managed conservatively.
CASE REPORT
A five-year-old girl was referred to the cleft unit for the evaluation of her facial cleft [Figure 1A]. Her family history was unremarkable for any craniofacial deformities. On local examination, a lateral facial cleft was observed on the left side. The full thickness defect extended into the skin of the cheek linearly, almost parallel to the ala-tragus line, terminating at about one third of its length. There were no other associated soft or hard tissue anomalies. All hematological investigations were within normal limits and no other systemic involvement was observed.

- (A) Preoperative view of the Lt Tessier 7 cleft (mouth open). (B) Wound dehiscence lateral to the neocommissure, 5 days postoperatively. (C) Appearance of the scar, 4 months postoperatively
Surgical repair was performed using the Pfeifer wave line incision. The incision was marked [Figure 1B] and the sterile zones were excised. The superior and inferior bellies of orbicularis oris were isolated by undermining the overlying skin and the underlying mucosa. Closure was performed from inside out starting with the mucosae. The surgical site was covered with a pressure dressing for stabilization. The patient was discharged the next day after an uneventful postoperative period.
Five days postoperatively, the patient reported to the hospital following an injury caused by a physical blow to her face by her younger sibling. A mild dehiscence was noted just lateral to the neocommissure without any signs of active bleeding [Figure 1B]. The dehiscence was not communicating with the oral cavity. She was prescribed an antiseptic ointment to encourage healing by secondary intention and ten days later, the sutures were removed. Six weeks postoperatively, no raw areas were observed and anti-cicatricial ointments were prescribed. Patient was advised to avoid direct sun exposure. Four months postoperatively, the scar looked healthy with a similar coloration to that of the surrounding skin [Figure 1C]. The texture was still mildly fibrotic, however, the neocommissure was well defined and her mouth opening was symmetrical. Thereafter, the patient was asked to report for annual follow-ups.
However, she reported after 6 months with a hypopigmented patch over the region that had previously dehisced [Figure 2A]. The rest of the scar was quite inconspicuous and its texture was soft and pliable. Following a dermatology consultation, it was decided to treat the scar per the treatment guidelines for leucoderma. The patient was prescribed a regimen that included the topical application of a psoralen compound (methoxysalen) followed by sun exposure on alternate days, tacrolimus ointment for bedtime application, and mometasone cream in the morning, for two weeks. Scar coloration improved rapidly over the next couple of weeks and after three months the leucodermic patch had resolved almost completely and no restriction in mouth opening was observed [Figure 2B].
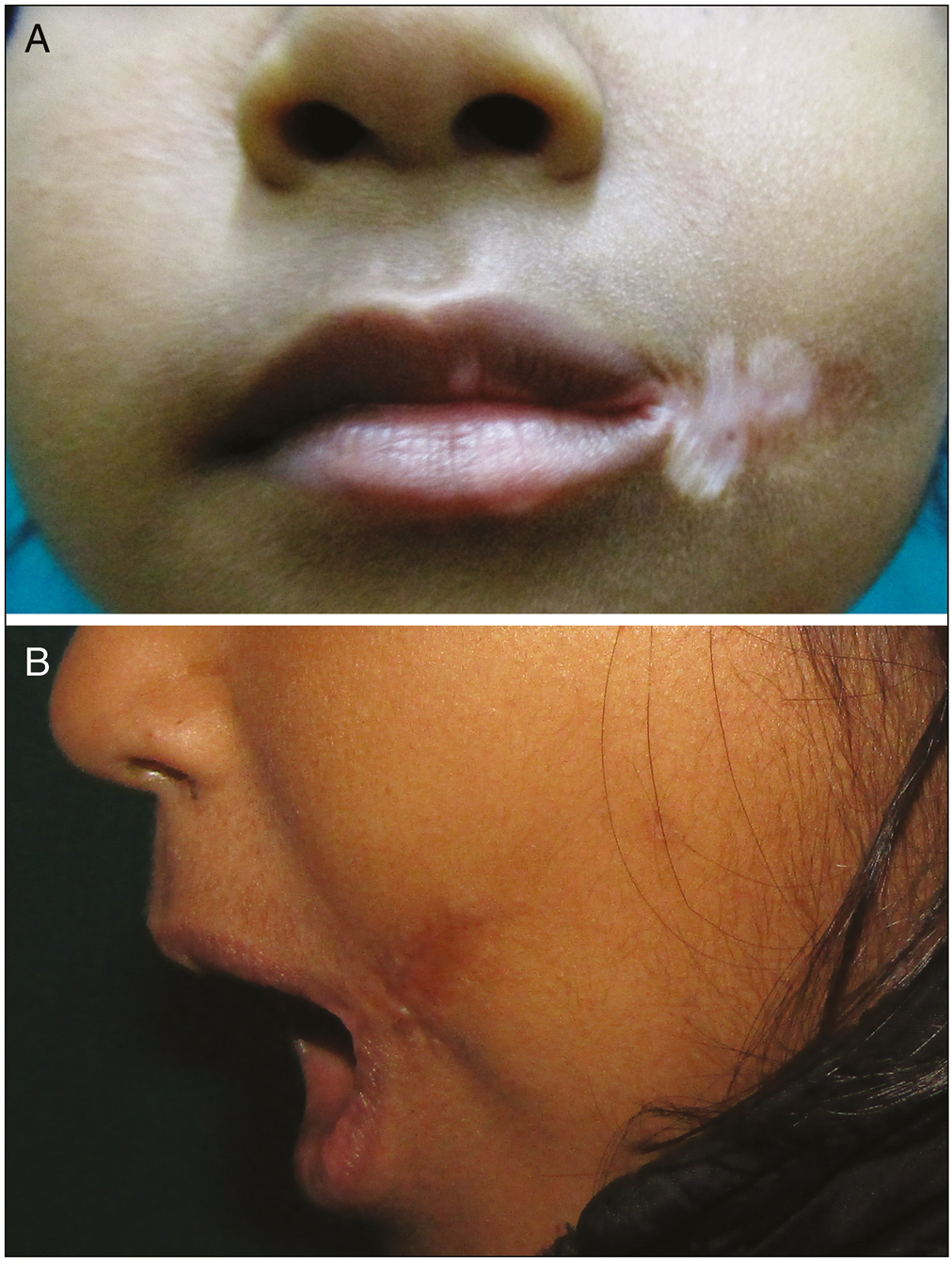
- (A) Hypopigmented patch over the previously dehisced area seen 11 months postoperatively. (B) Appearance of the scar 3 months following the prescribed treatment
DISCUSSION
Irrespective of the technique employed, the surgical goals for successful macrostomia repair have been outlined as: (1) restoration of symmetric lip length and height and contour; (2) creation of mobile and symmetric commissures; (3) myoplasty to restore labial function for speech, eating, and blowing; (4) skin closure with minimal visible scarring; and (5) mucosal repair with adequate vestibular space.[4,5,6] The Pfeiffer wave line incision[7] can be easily adapted to the form of the cleft and enables uniform distribution of the tissue without any angular scars.[8]
In the present case, a good surgical outcome was achieved in the short-term; however, the delayed appearance of a hypopigmented patch over the scar was undesirable. Abnormally pigmented scars present a challenge for clinicians due to the dearth of definitive treatments and can be highly distressing for patients. Furthermore, literature regarding the re-pigmentation of cutaneous scars is limited.
Sites with secondary intention healing can commonly have a hypopigmented, focally hypertrophic, or depressed cicatrix depending on their location. Concavities of the face, including the medial canthus and conchal bowl often heal imperceptibly. Conversely, convex surfaces such as the nasal tip and malar cheek can heal with depressed scars; while, flat areas of the cheeks, forehead, and chin may heal favorably.[9] Cosmetic tattooing, medium-depth chemical peels, carbon dioxide and erbium laser resurfacing, dermabrasion, skin grafting, cosmetic camouflage, and various forms of phototherapy and laser therapy have shown limited efficacy and variable safety profiles in the treatment of hypopigmentation.[10]
Although, initially a surgical revision was considered as a possible treatment; however, owing to the age of the patient, a conservative approach was adopted to avoid another surgical intervention. Table 1 outlines the features of the prescribed agents that have previously been used successfully for the treatment of pediatric leucoderma.
| Treatment modality | Mechanism | Features |
|---|---|---|
| Topical corticosteroids (TC) | Immunomodulatory effects | First line of treatment; local and systemic adverse effects with long-term use (tachyphylaxis, suppression of hypothalamic-pituitary adrenal axis, and growth retardation) |
| Psoralen and solar exposure (PUVAsol) | Direct stimulation of melanocytes from the hair follicles or the adjacent dark skin and reactivation of existing melanocytes in recently developed leucodermic area | Effective in both localized and generalized leucoderma |
| Tacrolimus | Topical calcineurin inhibitors (TCI); inhibit the expression of cytokines | Improved benefit-toxicity ratio. Proven success in re-pigmentation in pediatric cases |
Combination therapies have reported a better success rate, and are recommended for the pediatric population. Although, surgical excision completely removes the affected area and minimizes the new scarring created to close the defect; however, many areas of abnormal pigmentation may be too large for the same.
This report highlights the need for continuous follow-up despite seemingly good short-term results and outlines an effective medical management for hypopigmented scars that will aid fellow practitioners. It is recommended that a conservative approach be employed as the first line of treatment in children before opting for the seemingly obvious surgical revision.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Not applicable.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Tessier number 7 cleft with oblique clefts of bilateral soft palates and rare symmetric structure of zygomatic arch. J Plast Reconstr Aesthet Surg. 2008;61:447-50.
- [Google Scholar]
- Craniofacial cleft: A case of tessier no. 3, 7 and 11 cleft. J Plast Reconstr Aesthet Surg. 2006;59:1388-90.
- [Google Scholar]
- Macrostomia: A practical guide for plastic and reconstructive surgeons. J Craniofac Surg. 2016;27:118-23.
- [Google Scholar]
- Lippenkorrekturen nach friiheren Spalten- Operationen mit dem wellenschnittverfahren. Dtsch Zahnärztl. 1970;25:569.
- [Google Scholar]
- Fractional resurfacing for the treatment of hypopigmented scars: A pilot study. Dermatol Surg. 2007;33:289-94; discussion 293-4.
- [Google Scholar]





