Translate this page into:
Tertiary Health Care-Based Randomized Controlled Study to Compare Autologous, Non-cultured, Non-trypsinized Epidermal Cell Transplant (Jodhpur Technique) with Split-Thickness Skin Grafting (STSG) in Stable Vitiligo
Address for correspondence: Dr. Dilip Kachhawa, Shastri Nagar, Jodhpur, Rajasthan, India. E-mail: kachawahadrdilip@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
Surgical treatment of vitiligo is reserved for stable recalcitrant vitiligo patches. Split-thickness skin grafting (STSG) is an important established modality for the surgical treatment of vitiligo, whereas autologous, non-cultured, non-trypsinized epidermal cell transplant, also known as Jodhpur technique (JT), is an unconventional innovative surgical modality for the treatment of stable vitiligo.
Aims:
To compare the two techniques, JT and STSG, with regards to the extent and pattern of repigmentation achieved, color matching of the repigmented area, patient satisfaction (Dermatology Life Quality Index [DLQI] questionnaire and patient global assessment), and adverse events (if any) in patients with stable vitiligo.
Materials and Methods:
It was a randomized comparative study. We randomized 32 patients with 180 stable vitiligo lesions into two groups. Patients in group 1 were treated with JT, and those in group 2 with STSG. They were subjectively evaluated 20 weeks post-surgery for the extent of repigmentation, color match, change in DLQI score, and patient satisfaction. The categorical data were presented as number (percent) and were compared among groups using Chi-square test. Mean and standard deviation were calculated for demographic data, and they were also compared by using student t-test. Probability P value < 0.001 was considered statistically significant.
Results:
The extent of repigmentation was excellent (90%–100% repigmentation) in 72.5% of lesions in the JT group and in 40% of lesions in the STSG group (P < 0.001). Seventy-five percent repigmentation (good repigmentation) was observed in 95% of lesions in the JT group and in 83.75% of lesions in the STSG group (P = 0.040). There was a highly significant decline in DLQI score. Post-procedure DLQI (0.79 ± 1.13) and pre-procedure DLQI (15.39 ± 4.76) in the JT group were compared with post-procedure DLQI (3.85 ± 2.89) and pre-procedure DLQI (16.19 ± 4.56) in the STSG group. The mean decline among groups differed significantly (P < 0.001). Adverse events were significantly higher in the STSG group at the recipient site.
Conclusions:
JT is found to be significantly better than STSG with regard to the degree of repigmentation.
Keywords
Grafting
non-trypsinized
STSG
surgery
vitiligo
INTRODUCTION
Vitiligo is an acquired disorder of depigmentation. Histopathologically, loss of functional melanocytes manifests clinically as depigmented patches. Medical management is the initial modality of treatment for most vitiligo cases. However, in cases not responding to medical management, surgical modalities must be used. Disease stability, defined as no occurrence of new vitiligo lesions or an extension of preexisting lesions for a specific period, is a prerequisite for surgical management. The latest Vitiligo Global Issues Consensus Conference guidelines recommend a minimum of one-year period of stability for surgical intervention.[1]
Among the surgical modalities, punch grafts, suction blister grafts,[2] epidermal cellular grafts,[3] melanocyte culture and grafting,[4] and autologous, non-cultured melanocyte grafting[5] are well-known treatment options. JT[6] is a recent surgical modality for the management of vitiligo. This comparative study is planned to compare the outcome of two surgical modalities, namely STSG and autologous, non-cultured, non-trypsinized, melanocytes plus keratinocytes grafting (JT), in patients with stable vitiligo.
Aims and objectives
The primary outcome was to compare the effectiveness of two surgical methods in the treatment of stable vitiligo patches using parameters such as the extent and pattern of repigmentation, color matching of repigmented area.
The secondary outcome was to compare patient satisfaction (DLQI questionnaire and patient global assessment) and adverse events, if any, in both techniques.
Null hypothesis: There was no significant difference in the extent of pigmentation induced by JT vs. STSG as a surgical modality for the treatment of stable vitiligo.
MATERIALS AND METHODS
This interventional, randomized comparative study was conducted at a tertiary health center in Western Rajasthan. Patients were selected randomly from those presenting to our outpatient Department of Dermatology. A total of 160 stable vitiligo patches from 32 patients were included by applying the following inclusion and exclusion criteria.
Inclusion criteria
Subjects with a clinical diagnosis of vitiligo that has been stable for a minimum of one year and not responding to medical treatment.
Exclusion criteria
Age younger than 10 years and older than 50 years
Patient with actively spreading vitiligo
Pregnancy and lactation
History of hypertrophic scars or keloidal tendency
Bleeding disorders
Patients with unrealistic expectations
Patients with connective tissue disorders
After obtaining institutional ethical committee approval and patients’ written informed consent, patients were subjected to vitiligo surgery. Patients were asked to fill the DLQI Questionnaire, which was designed by Dr. Finlay.[7] Anxiolytics were given in the night before the surgery and in the morning on the day of the surgery. Vitiligo patches were randomly divided into two groups by using the chit-in-box method: Group 1 and Group 2. Group 1 comprised 80 stable vitiligo patches treated by JT; group 2 comprised 80 stable vitiligo patches treated by STSG.
Technique of transplantation
Procedure at donor site
The lateral area of the thigh was selected as the donor area in all the cases. The donor area needed for collecting grafting material was approximately one-fourth of the recipient area in JT and equal to or slightly larger in STSG.
In JT, the graft was obtained by dermabrasion at a slow rpm and the superficial epidermal layers were removed by just rolling the fraise twice or thrice over the donor site. An antibiotic ointment (2% mupirocin) was applied over the donor site. The ointment helps to entangle the epidermal particles that are separated during the process of epidermal dermabrasion. Dermabrasion was continued till the area appeared whitish (i.e., upper dermis). At this junction, dermabrasion was stopped and the epidermal material entangled in ointment was collected with the help of a spatula or graft spreader. A paste-like material was obtained. This paste-like ointment containing melanocytes and keratinocytes was spread over the recipient site.
In STSG, the donor area was shaved using aseptic precautions; the graft was taken with the help of a shaving blade held firmly by a straight artery forceps and transferred under aseptic conditions to a container with normal saline.
Procedure at recipient site
The recipient site was prepared similar to the donor site.
Dermabrasion was done until tiny pinpoint bleeding spots were seen.
In STSG, the graft was placed over the denuded area, taking care to ensure that the dermal surface was facing down.
In cellular grafting, the paste-like material containing melanocytes and keratinocytes was spread over the recipient site.
Dressing with antibiotic-soaked gauge was done over the donor and recipient sites.
Suitable antibiotics and analgesics were prescribed. The dressing was removed after seven and 14 days from the recipient site and donor site, respectively.
Follow-up
Patients were asked to follow up on day 8; week 4, 6, 10, 14, and 20 after the procedure.
After seven days when the dressing was removed, at the recipient site of JT a blackish graft was seen that fell off on its own in the next three to five days. Topical psoralen with sunlight (PUVASOL) was started after 14–21 days in the form of methoxsalen 0.75% w/v. It was applied on the recipient area during the night and morning as well, followed by exposure to sunlight for 10 min (twice a week). PUVASOL was given in both techniques.
Repigmentation was assessed subjectively by an unbiased observer, based on a comparison of the digital photographs [Table 1]. It included extent, grading, type, and color matching of repigmentation. Also, the change in DLQI[7] and patient satisfaction questionnaire (PSQ) scores[8] were compared between the two groups. Patient’s global assessment with the help of a PSQ was used, including three questions—“grade the change in pigmentation in the transplanted area,” “are you satisfied with the treatment?” and “do you find the treatment worthwhile?” Patients were asked to answer in terms of scoring from 0 to 10.
| Percent repigmentation | Grading |
|---|---|
| <50% | Poor repigmentation |
| 50%–74% | Fair repigmentation |
| 75%–89% | Good repigmentation |
| 90%–100% | Excellent repigmentation |
The repigmentation patterns were noted as “diffuse,” “perifollicular” or “dotted,” and marginal. A note was also made of the color matching of the repigmented skin as “somewhat lighter than,” “same as,” or “somewhat darker than” normal skin.
Statistical analysis was performed with the PRIMER and SPSS, Tril version 20 for Windows statistical software package (SPSS Inc, Chicago, IL, USA). The categorical data were presented as number (percent) and were compared among groups using Chi-square test. Mean and standard deviation were calculated for demographic data, and they were also compared by using student t-test. Probability P value < 0.001 was considered statistically significant.
RESULTS
Thirty-two patients with a clinical diagnosis of stable vitiligo, and a total of 160 lesions were included in the study. Final analysis was done at 20 weeks. Eighteen were females, and 14 were males. Totally, 22 patients (68.75%) were same in both the groups. Among the remaining 10 patients, five (15.62%) patients were treated with JT and five (15.62%) were treated with STSG.
The mean duration of vitiligo patches was 22.63 ± 6.344 years, and the mean period of stability of patches was 3.89 ± 3.89 years [Table 2].
| No. | % | |
|---|---|---|
| Total patients | 32 | |
| Patients treated by JT | 5/32 | 15.625 |
| Patients treated by STSG | 5/32 | 15.625 |
| Patients treated by both JT and STSG | 22/32 | 68.75 |
| Total vitiligo patches | 160 | |
| Patches treated by STSG | 80 | 50 |
| Patches treated by JT | 80 | 50 |
| Female | 18 | 56.25 |
| Male | 14 | 43.75 |
| Leukotrichia | No | |
| Absent | 23 | 71.88 |
| Present | 9 | 28.13 |
Results were comparable between two groups on the basis of vitiligo type and the mean size of the treated area [Table 3, Figure 1].
| Parameters | JT group | STSG group | P value |
|---|---|---|---|
| Vitiligo type (G/F/S) | 65/13/2 | 61/14/5 | 0.48 |
| Size (mean) | 6.59 ± 10.39 | 5.47 ± 5.84 | 0.40 |
F = focal, G = generalized, S = segmental
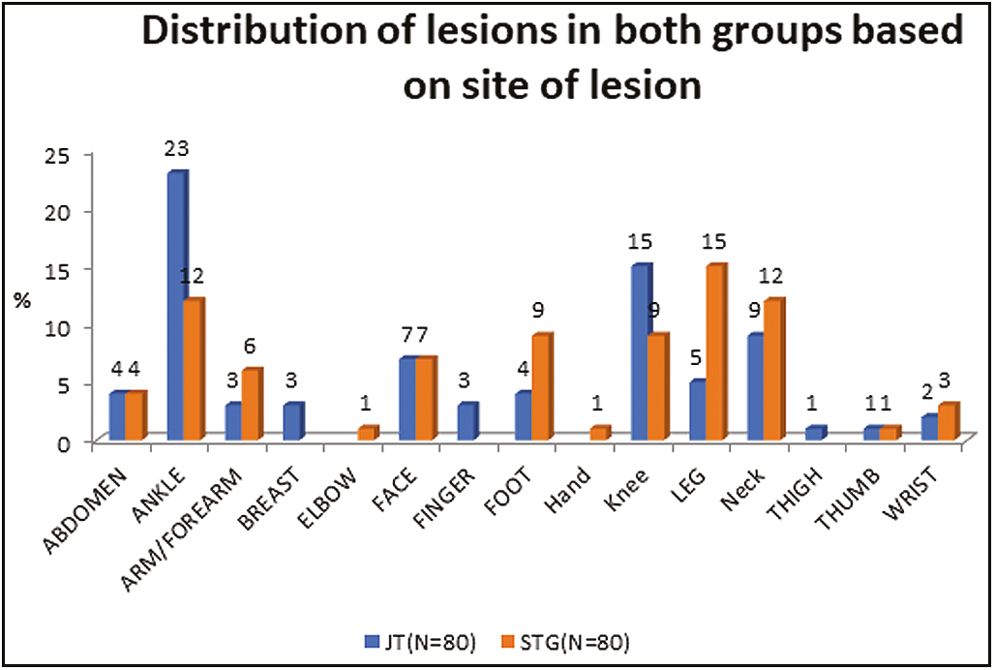
- Distribution of lesions in both groups based on the site of lesions
At six weeks, there was <75% of repigmentation in all patches of the JT group whereas there was 75%–90% of repigmentation in four patches of the STSG group. At 10 weeks, 32 out of 80 (40%) lesions in the STSG group showed ≥75% extent of repigmentation whereas only one out of 80 patients in the JT group showed this much extent of repigmentation at this state (P < 0.001). However, over a period of the next four weeks (at 14 weeks) of follow-up, 57 out of 80 (71.25%) lesions in the JT group and 59 out of 80 (73.75%) lesions in the STSG group showed ≥75% extent of repigmentation but this was statistically nonsignificant (P = 0.859). Twenty-eight out of 80 lesions (35%) in the STSG group showed >90% extent of repigmentation at the 14 weeks of follow-up, whereas none in the JT group (P < 0.001) showed repigmentation. This value was highly significant. Repigmentation ≥75% at week 20 was achieved in 76 out of the 80 (95%) lesions in the JT group compared with 67 out of the 80 (83.75%) lesions in the STSG group (P = 0.040). Also, 58 out of 80 lesions (72.5%) in the JT group and only 32 out of 80 lesions (40%) in the STSG group showed >90% extent of repigmentation (P < 0.001). Repigmentation started four weeks earlier in the STSG group than the JT group [Table 4, Figure 2].
| Grade of repigmentation | Extent of repigmentation (%) | JT (N = 80) | STSG (N = 80) | Total | Chi-square test | ||
|---|---|---|---|---|---|---|---|
| P value LS | |||||||
| FU 6 | |||||||
| 0 | No. | 0 | 1 | 1 | <0.001S | ||
| 1 | Poor | 67 | 83.75 | 35 | 102 | ||
| 2 | Fair | 13 | 16.25 | 40 | 53 | ||
| 3 | Good | 0 | 4 | 4 | |||
| 4 | Excellent | 0 | 0 | ||||
| FU 10 | |||||||
| 0 | No. | 0 | 0 | 0 | 0 | 0 | <0.001S |
| 1 | Poor | 23 | 28.75 | 8 | 10 | 31 | |
| 2 | Fair | 56 | 70 | 40 | 50 | 96 | |
| 3 | Good | 1 | 1.25 | 32 | 40 | 33 | |
| FU 14 | |||||||
| 0 | No. | 0 | 0 | 0 | 0 | 0 | <0.001S |
| 1 | Poor | 4 | 5 | 3 | 3.75 | 7 | |
| 2 | Fair | 19 | 23.75 | 18 | 22.5 | 37 | |
| 3 | Good | 57 | 71.25 | 31 | 38.75 | 88 | |
| 4 | Excellent | 0 | 28 | 35 | 28 | ||
| FU 20 | |||||||
| 0 | No. | 0 | 0 | 0 | 0 | 0 | |
| 1 | Poor | 0 | 2 | 2.5 | 2 | <0.001S | |
| 2 | Fair | 4 | 5 | 11 | 13.75 | 15 | |
| 3 | Good | 18 | 22.5 | 35 | 43.75 | 53 | |
| 4 | Excellent | 58 | 72.5 | 32 | 40 | 90 | |
LS = level of significance
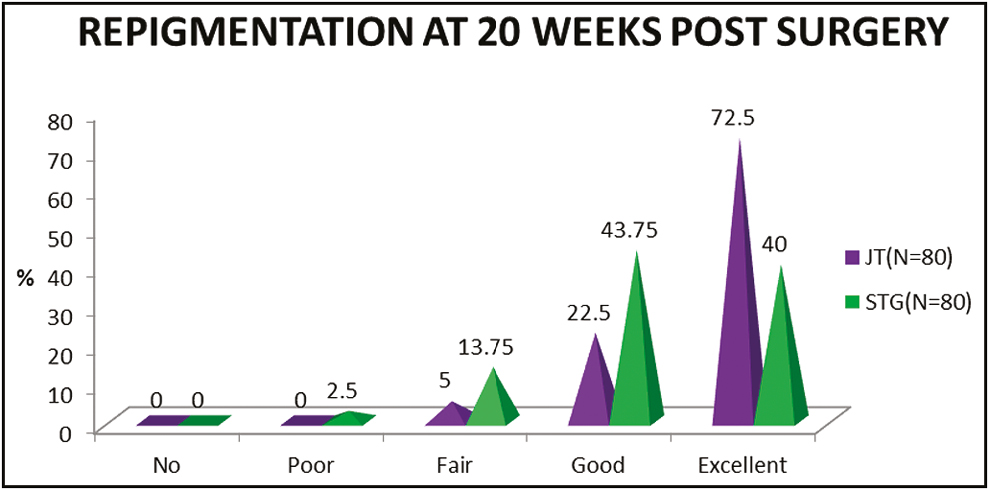
- Extent of repigmentation at 20 weeks post-surgery
At 20 weeks of follow-up, for 78 out of 80 lesions in the JT group (97.5%) and 16 out of 80 lesions in the STSG group (20%), the color of the repigmented area matched excellently with the normal surrounding skin [Table 5, Figure 3].
| Color match with surrounding skin | JT (N = 80) | STSG (N = 80) | Total | Chi-square test | ||
|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | P value LS | |
| FU 6 | ||||||
| Darker than surrounding skin | 7 | 8.75 | 75 | 93.75 | 82 | <0.001S |
| Same with surrounding skin | 73 | 91.25 | 5 | 6.25 | 78 | |
| FU 10 | ||||||
| Darker than surrounding skin | 6 | 7.5 | 72 | 90 | 78 | <0.001S |
| Same with surrounding skin | 74 | 92.5 | 8 | 10 | 82 | |
| FU 14 | ||||||
| Darker than surrounding skin | 6 | 7.5 | 64 | 80 | 78 | <0.001S |
| Same with surrounding skin | 74 | 92.5 | 16 | 20 | 82 | |
| FU 20 | ||||||
| Darker than surrounding skin | 2 | 2.5 | 64 | 80 | 66 | <0.001S |
| Same with surrounding skin | 78 | 97.5 | 16 | 20 | 94 | |
LS = level of significance
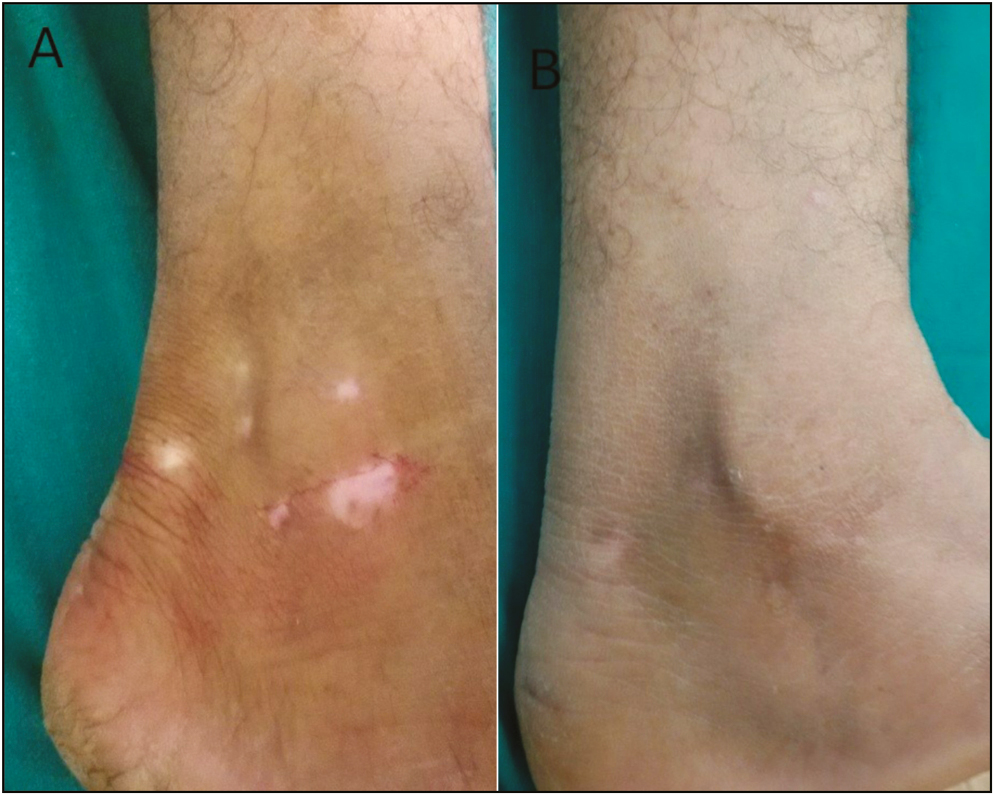
- Jodhpur technique in vitiligo patch on malleoli: (A) Pretreatment and (B) posttreatment at 20 weeks
Diffuse repigmentation was the most common pattern of repigmentation observed in 85% of lesions overall (75% of lesions in the JT group and 95% of lesions in the STSG group) [Table 6].
| Pattern of repigmentation | JT (N = 73) | STSG (N = 73) | Total | ||
|---|---|---|---|---|---|
| No. | % | No. | % | No. | |
| DF | 60 | 75 | 76 | 95 | 136 |
| M | 18 | 22.5 | 9 | 11.25 | 27 |
| DD | 8 | 10 | 0 | 7 | |
| PF | 4 | 5 | 0 | 4 | |
DD = dotted, DF = diffuse, M = marginal, PF = perifollicular. Chi-square = 16.753 with three degrees of freedom; P < 0.001S
Comparing the mean change in pre and post-surgery (20 weeks) DLQI, we observed a highly significant (P < 0.001) decline in DLQI in both the groups [Table 7]. The mean reduction in DLQI was found to be significantly greater in the JT group compared with the STSG group (P < 0.001).
| Pre | Post | P value (paired t test) | |
|---|---|---|---|
| Group JT | 15.39 ± 4.75 | 0.79 ± 1.13 | <0.001 |
| Group STSG | 16.19 ± 4.56 | 3.85 ± 2.89 | <0.001 |
| P value (independent-sample t-test) | 0.279 | <0.001 |
According to paired t test statistics, DLQI pre and post in JT and STSG was significant. Post-DLQI was significantly lower in both the groups. There was a highly significant decline in DLQI score. Post-procedure DLQI (0.79 ± 1.13) and pre-procedure DLQI (15.39 ± 4.76) in the JT group could be compared with post-procedure DLQI (3.85 ± 2.89) and pre-procedure DLQI (16.19 ± 4.56). Therefore, the mean decline in DLQI among the groups differed significantly.
Also, the difference between the mean of all three PSQs was statistically significant (P < 0.001). So, patients were significantly more satisfied in the JT group compared with the STSG group [Table 8].
| Group JT | Group STSG | P value (independent sample t test) | |
|---|---|---|---|
| PSQ1 | 9.35 ± 1.03 | 7.38 ± 1.76 | <0.001 |
| PSQ2 | 9.05 ± 1.23 | 6.83 ± 1.80 | <0.001 |
| PSQ3 | 9.20 ± 1.18 | 6.84 ± 1.79 | <0.001 |
Adverse events were significantly higher in the STSG group at the recipient site (P < 0.001). Graft hypertrophy and rejection were significantly higher in the STSG group (P < 0.001 and P = 0.006, respectively) [Table 9, Figure 4].
| Recipient site | JT (N = 80) | STSG (N = 80) | Total | Chi-square test | ||
|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | P value LS | |
| No complication | 40 | 50 | 14 | 17.5 | 54 | <0.001S |
| Milia | 0 | 0 | 1 | 1.25 | 1 | 1.0NS |
| Hypertrophy of graft | 0 | 0 | 25 | 31.25 | 25 | <0.001S |
| Rejection of graft | 0 | 0 | 9 | 11.25 | 9 | 0.006S |
LS = level of significance, NS = no significance. Chi-square = 60.262 with four degrees of freedom; P = 0.000
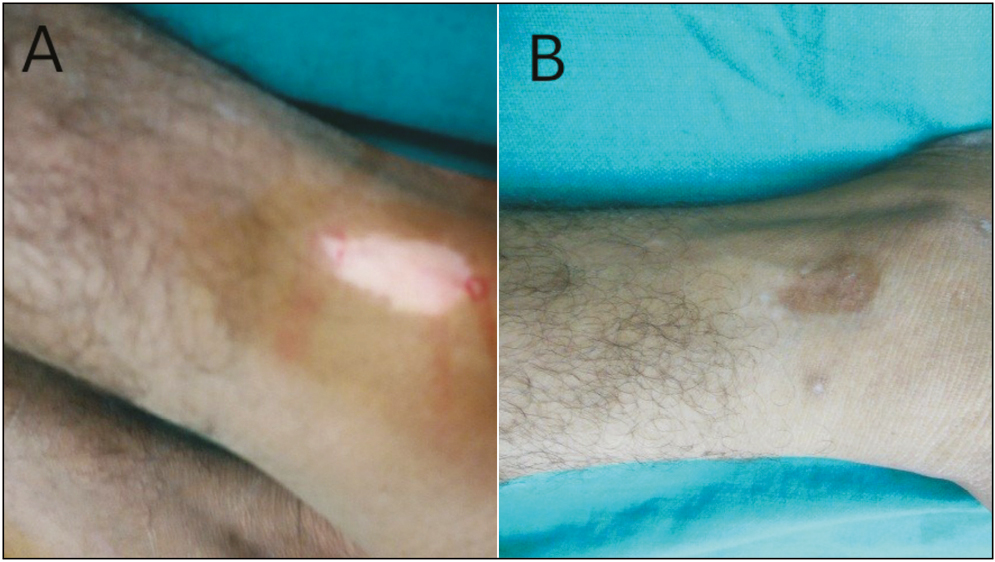
- STSG in vitiligo patch on malleoli: (A) Pretreatment and (B) posttreatment at 20 weeks
DISCUSSION
Despite the limitations and some side effects, surgical modalities appear to be the method of choice in recalcitrant stable vitiligo.
The STSG is a simple and easy-to-follow surgical technique for the treatment of stable vitiligo. However, achromic fissure, perigraft halo, color mismatch with surrounding skin, and hypertrophy of graft are some common and cosmetically significant problems that are commonly encountered after STSG.[9]
The introduction of epithelial grafting is considered a promising tool in those resistant cases; however, failures are still possible outcomes.[9] The cultured autologous melanocytes technique and its modifications are excellent methods of producing enormous amounts of melanocytes for transplanting a large area of vitiligo but it needs well-trained, skilled staff and also, the laboratory setup is expensive.
Autologous, non-cultured, non-trypsinized, melanocytes plus keratinocye grafting (JT) is a simple and new method of melanocytes transfer in stable vitiligo. However, it has not been standardized and is still in an early phase of development.
Some systematic review studies have been carried out between tissue and cellular transplant methods. Njoo et al.[10] collected 39 studies, comprising minigrafting, split-thickness grafting, grafting of epidermal blisters, grafting of cultured melanocytes, and grafting of non-cultured epidermal suspension. The highest success rates were achieved with split-thickness grafting (87% [95% CI, 82%–91%]) and epidermal blister grafting (87% [95% CI, 83%–90%]). The lowest success rate was reported with grafting of non-cultured epidermal suspension (31% [95%CI, 11%–59%]).
The reason behind this outcome can be explained by the fact that patients in the non-cultured epidermal suspension group were too few to draw a firm conclusion and this study was carried out in the year 1998, when the non-cultured epidermal cell suspension (NCES) method was still in its early stage of development.
In our study, we could not get repigmentation at the fingers and elbow with either of the methods, similar to a retrospective study carried out by Olsson and Juhlin.[11]
We observed more than 90% (excellent) repigmentation in 72.5% of lesions in the JT group and 40% of lesions in the STSG group. The extent of repigmentation of ≥75% (good) was seen in 95% of lesions in the JT group compared with 83.75% in the STSG group. So, JT for vitiligo surgery was found to be significantly superior to the STSG technique in terms of the degree of repigmentation.
The significantly better results in terms of excellent repigmentation (90%–100%) obtained with JT over STSG can be explained by the hypothesis suggested by Budania et al.[12] as in epidermal grafts, there is some resistance to pigment spread in vitiligo patch and they also have a tendency to roll, split, and displace from the recipient site with slight movement, resulting in a lesser extent of repigmentation. No such problems are encountered with JT.
Van Geel et al.,[13] utilizing the modified procedure, reported 70% repigmentation in 62% of the 40 patients at the last follow-up visit.
We observed excellent repigmentation (90%–100%) in 40% patients that was poorer than the study by Kahn and Cohen,[14] who observed excellent repigmentation in 83.33% patients; however, in terms of good to excellent repigmentation (>75%), our results (83.75%) were slightly better than the comparative study done by Khandpur et al. (83.33%).[15]
We found that ≥75% repigmentation was seen in 32 out of 80 lesions in the STSG group and one out of 80 lesions in the JT group at 10 weeks. This is an important difference between the tissue and cellular transfer techniques, as described earlier. However, at 14 and 20 weeks of follow-up, 57 and 76 out of 80 lesions, respectively, in the JT group and 59 and 67 lesions out of 80 lesions, respectively, in the STSG group reached ≥75% repigmentation.
The reason for faster repigmentation in the STSG group can be explained by the hypothesis suggested by Budania et al.[12] According to that, in tissue graft, the epidermis has a higher melanocyte concentration and this higher concentration of melanocytes helps in faster early repigmentation. However, on the other hand, there was little spread of repigmentation achieved in early time because of some resistance to pigment spread in epidermal grafts and the repigmentation was limited to the area where the graft was applied.
In JT, the concentration of melanocytes in suspension is lower than a tissue graft. So, the initial speed of repigmentation was slow. However, as the melanocytes repopulate the recipient site evenly, the final outcome was better in terms of the extent of repigmentation. Keratinocytes were also transferred along with melanocytes in JT, which helped in the growth and survival of melanocytes.
The adverse effects were minor in our study. None of our patients showed scarring or infection. A few patients exhibited postoperative hyper-pigmentation at the donor site, which vanished over time. Complications at the recipient site were statistically and significantly more in the STSG group (P < 0.001). At the recipient site, 50% lesions showed persistent depigmentation in the JT group whereas 66.25% lesions showed persistent depigmentation in the STSG group. Persistent depigmentation was central and perilesional (halo phenomenon) in the JT and STSG group, respectively. Though not significant, halo phenomena can be due to some difficulty in pigment spread in the STSG technique.
The most commonly observed pattern of pigmentation was diffuse. This signifies that the repigmentation was due to transplanted melanocytes by JT and STSG. Perifollicular or marginal repigmentation is mainly induced by the melanocytes reserve in the hair follicle, which is stimulated by dermabrasion or phototherapy.
We observed a significant reduction in DLQI after surgery, similar to the study of van Geel et al. and Budania et al.[1213] The reduction in DLQI was significantly better in the JT group compared with the STSG group. Apart from DLQI, PSQ scores were significantly higher in the JT group than in the STSG group. One particular problem faced by every patient in the STSG group was that they were very anxious about the ugly look of graft (stuck on appearance) after the removal of dressing. No such problem was faced by any of the patients in the JT group. That is why patients in the JT group were significantly much more satisfied than those in the STSG group.
Our study is the first of its kind in the literature to compare a new cellular transplantation technique (JT) with a well-established tissue transplantation technique (STSG). Cellular transplantation techniques have been found to be sophisticated, costly, require a laboratory, and are somewhat difficult to be performed at the clinic. However, we used a very cheaper technique of JT without any melanocyte culture media, trypsin inhibitor, hyaluronic acid, or phosphate buffer saline. We did not use any sophisticated or costly apparatus.
We took into consideration patient satisfaction and improvement in DLQI, which are important parameters to consider in a psychologically disabling disease such as vitiligo, especially since it has been reported that the extent of repigmentation may not correlate directly with patient satisfaction and improvement in the quality of life.
So, in the light of the facts mentioned earlier, we compared two simplified techniques of vitiligo surgery. Our study indicates that both JT and STSG are safe and effective techniques in terms of good repigmentation (≥75% extent of repigmentation) but JT is superior to STSG in terms of excellent repigmentation (90%–100% extent of repigmentation), color match, side effects, patient satisfaction, and DLQI reduction. However, further molecular-level research still needs to elaborate the factors impeding pigment spread in STSG and the factors provided by keratinocytes for the growth and survival of melanocytes in JT.
Limitations
Assessment for repigmentation in both groups was subjective, based on digital photography.
Test for normality of data was not done.
Age of the patients and comorbidities such as diabetes were not matched in the two groups.
CONCLUSION
This is the first study to compare a new cellular transplantation technique with an established tissue transplantation technique. We found that JT was significantly better than STSG in terms of the extent of repigmentation and patient satisfaction. Another benefit of JT is that it can cover a larger body surface area with smaller grafts. Repigmentation was seen earlier in the STSG group. The STSG is time-consuming as compared with JT, and also adverse effects are more in STSG. Our study suggests that JT has an edge over STSG in patients with stable vitiligo.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Revised classification/nomenclature of vitiligo and related issues: The vitiligo global issues consensus conference. Pigment Cell Melanoma Res. 2012;25:E1-13.
- [Google Scholar]
- Efficacy of suction blister epidermal graft without phototherapy for locally stable and resistant vitiligo. Indian J Dermatol. 2012;57:282-4.
- [Google Scholar]
- Surgical treatment of vitiligo: Why, when and how. J Eur Acad Dermatol Venereol. 2003;17:518-20.
- [Google Scholar]
- A study of autologous melanocyte transfer in treatment of stable vitiligo. Indian J Dermatol Venereol Leprol. 2005;71:393-7.
- [Google Scholar]
- Autologous grafting with noncultured melanocytes: A simplified method for treatment of depigmented lesions. J Am Acad Dermatol. 1992;26:191-4.
- [Google Scholar]
- Simplified non-cultured non-trypsinised epidermal cell graft technique followed by psoralen and ultraviolet A light therapy for stable vitiligo. J Cutan Aesthet Surg. 2017;10:81-5.
- [Google Scholar]
- Dermatology life quality index (DLQI)—A simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19:210-6.
- [Google Scholar]
- Validation of a patient satisfaction questionnaire in primary health care. Public Health. 2012;126:710-8.
- [Google Scholar]
- Grafting in vitiligo: How to get better results and how to avoid complications. J Cutan Aesthet Surg. 2013;6:83-9.
- [Google Scholar]
- A systematic review of autologous transplantation methods in vitiligo. Arch Dermatol. 1998;134:1543-9.
- [Google Scholar]
- Long-term follow-up of leucoderma patients treated with transplants of autologous cultured melanocytes, ultrathin epidermal sheets and basal cell layer suspension. Br J Dermatol. 2002;147:893-904.
- [Google Scholar]
- Comparison between autologous noncultured epidermal cell suspension and suction blister epidermal grafting in stable vitiligo: A randomized study. Br J Dermatol. 2012;167:1295-301.
- [Google Scholar]
- Modified technique of autologous noncultured epidermal cell transplantation for repigmenting vitiligo: A pilot study. Dermatol Surg. 2001;27:873-6.
- [Google Scholar]
- Repigmentation in vitiligo patients. Melanocyte transfer via ultra-thin grafts. Dermatol Surg. 1998;24:365-7.
- [Google Scholar]
- Comparison of minipunch grafting versus split-skin grafting in chronic stable vitiligo. Dermatol Surg. 2005;31:436-41.
- [Google Scholar]






