Translate this page into:
Aesthetic reconstruction of the upper antihelix in external ear with banner pull-through flap
Address for correspondence: Dr. Ali Ebrahimi, PO Box 1994943636, Tehran, Iran. E-mail: ae_49341@yahoo.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
We can use pre auricular and post auricular skin as a pull through flap for upper antihelix defects reconstruction.
Patients and Methods:
This was a prospective case-series study, which was done in the Department of Plastic and Reconstructive Surgery Ward. In this study, 15 patients (3 women, 12 men), ranging from 45 to 72 years old (mean, 58 years) underwent operation with pull through banner flap for reconstruction of upper antihelix (7 cases) and triangular fossa with superior and inferior crura (5cases) caused by BCC or SCC excision. Reconstruction of upper antihelix defects up to 20 × 30 mm with post auricle pull through flap and reconstruction of triangular fossa up to 20 × 20 mm with pre auricle pull through flap were done.
Results:
Our study showed that pull through flap with superior pedicle from post auricular and preauricular area was an effective method for reconstruction of upper ear antihelix defects.
Conclusion:
We advocate that the pull through flap with superior pedicle from post auricle and pre auricle is an excellent choice for reconstruction of upper antihelix ear reconstruction in both crura and triangular fossa.
Keywords
Aesthetic
antihelix
flaps
pull-through
INTRODUCTION
The auricle is composed of tightly adherent skin over a cartilaginous framework. Between the skin envelope and underlying cartilage lies a layer of adipose tissue that is present on the posterior surface of the auricle but absent on the anterior surface, The position of the external ear predisposes it to both traumatic injury and malignancy.[1]
Reconstruction of nonmarginal defects of the upper part of the ear while maintaining ear shape and length is a challenging problem.[2] Defects of the auricle frequently occur within the context of congenital deformities, trauma, and in particular, the surgical excision of benign and malignant tumors.[3] Postauricular scalp-to-anterior auricle pull-through subcutaneous pedicle flap should be considered for defect of the scaphoid fossa and antihelix; it is performed as a one-stage procedure.[4]
PATIENTS AND METHODS
This was a prospective case-series study, which was conducted in the Department of Plastic and Reconstructive Surgery in our hospital in Tehran, Tehran Province, Iran between 2012 and 2014. All patients were referred by the dermatologist after incisional biopsy of antihelix lesions and confirmation of malignancy. The procedures of ear antihelix reconstruction was explained to the patients, the advantages and disadvantages of pull-through flap from postauricular and preauricular areas were described to all the patients, and all of them filled the consent form before operation. This study protocol was approved by the ethics committee in Baqiyatallah University of Medical Sciences (BMSU) University of Medical Sciences.
In these patients, excision of antihelix tumor with a safe margin of 4-6 mm was performed; also, in all patients underlying cartilage adjacent to the tumor was excised with the tumor.
In this study, 15 patients (3 women, 12 men), with an age range of 45-72 years (mean: 58 years) underwent operation with banner pull-through flap for reconstruction of the upper antihelix (7 cases) and triangular fossa with superior and inferior crura (5 cases) caused by basal cell carcinoma (BCC) or squamous cell carcinoma (SCC) excision [Table 1]. Reconstructions of the upper antihelix defects up to 20 × 30 mm with postauricular pull-through flap and reconstruction of triangular fossa up to 20. × 0 mm with preauricular pull-through flap were done.

We did not use any cartilage under the flap, The special operation result form was completed for all patients, and aesthetic and functional aspects were evaluated. Photography was taken before and after the operation of all patients.
Designing of flap
The postauricular flap with superior based pedicle was designed in the upper postauricular neck skin [Figure 1]. The base of the flap was deepithelialized superficially, only including the epidermis in that portion that had to be tunneled in the upper antihelix. The diameter of the tunnel was a little larger than the width of flap in the deepithelialized portion. Designing of flap in the preauricular portion was similar to the posterior one [Figure 2]; both flaps had a banner pattern and transposed through the tunnel for ear reconstruction. In posterior defects, postauriclular design is suitable and in anterior defects between the antihelix crura preauricular design was better. This is a single-stage operation. Donor site of flap in both areas closed primarily and it was hidden in the postauricular or preauricular area; the size of tunnel was a little larger than the width of flap in the base. The thickness of the flaps was similar to the thickness of the defects.
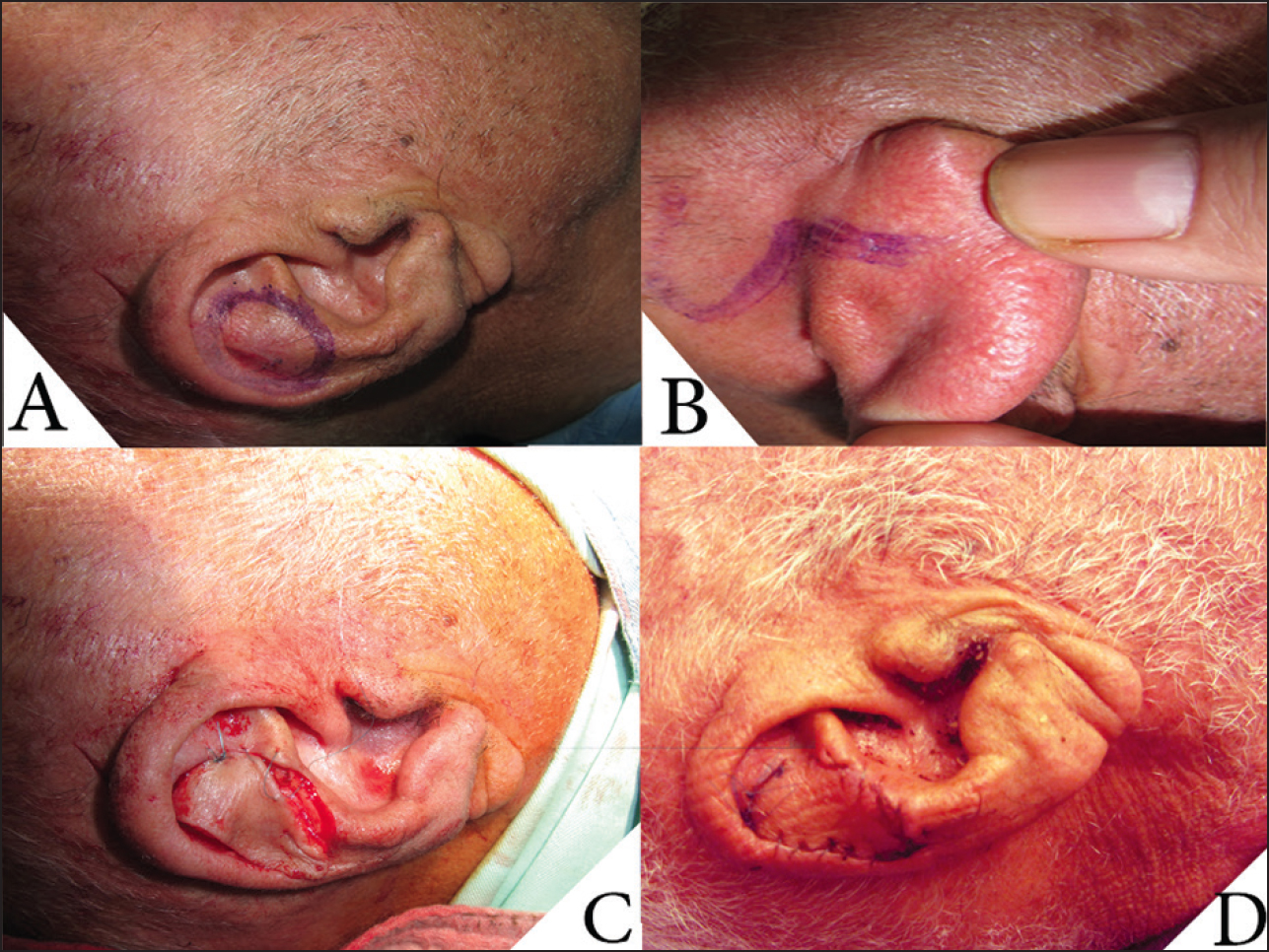
- (a and b) Designing of postauricular pull-through flap (c) Intraoperative view of flap (d) Postoperative view of flap

- (a) Before operation designing of preauricular pull-through flap (b and c) Intraoperative view of flap (d and e) 1-month postoperative view of flap. In this figure, the stages of flap designing and ear reconstruction are shown
RESULTS
Fifteen patients (3 women, 12 men), with an age range of 45-72 years (mean age: 58 years), were included in this survey [Table 1]. Our study showed that banner pull-through flap with superior pedicle from postauricular and preauricular areas was an effective method for reconstruction of upper ear antihelix defects (both crura and triangular fossa); if defect is in the posterior part, postauricular design is suitable [Figure 1] and in anterior defect between crura, preauricular design [Figure 2] is better. We used this flap without any complication in our patients. The technique leads to excellent correction of ear skin defects in these areas. All the patients were satisfied, and antihelix skin defects were corrected in all cases with good aesthetic and functional results. The donor site of flaps was closed primarily with good aesthetic result. There were no complications such as ischemia, infection, necrosis, or bulging of flap. Long-term results were good.
DISCUSSION
Postauricular area is an excellent donor source for full-thickness skin graft or skin flap to close the soft tissue defects in the face. The postauricular surface is mainly supplied by auricular branches of the postauricular artery.[56] The postauricular area is an ideal donor site for reconstruction of the anterior surface of the external ear because it is closer to defect, and therefore, color, texture, and thickness match the defect, and its scar is more inconspicuous.[7] Malignant lesions of the external ear account for approximately 6% of all head and neck skin cancers. These cancers usually occur in older men with history of excessive sun exposure. The auricle is especially susceptible to actinic injury because of its projection and exposure. The most common malignancies are basal cell cancer, squamous cell cancers, and rarely melanoma.[8]
The human ear is one of the most complex three-dimensional structures of the external body. Auricular defects can be classified according to anatomical location, whether affecting the conchal bowl, antihelix, antitragus, helical rim, or lobule. Additionally, the involved tissues need to be considered.[9] Several articles categorize the defects of the auricle to aid reconstruction based on anatomic location, extent, and depth of the defect.[1011]
Surgical reconstruction of an almost normal ear is a difficult challenge.[12] Local anesthesia block with epinephrine was the method of choice for resection and some reconstructions following ear cancer excision; except for large neglected tumors that need general anesthesia. There are several options for antihelix and concha reconstructions including primary repair, different local flaps, skin graft. Full-thickness skin grafts can harvested from the postauricular, preauricular, supraclavicular, or lateral neck regions.[8] Various chondrocutaneous reconstruction methods have been described for defects up to one-third of the auricle. These flaps are based on the redistribution of the ear elements to cover the defect and try to maintain ear size and shape.[8]
The retroauricular skin may well be considered a “flap bank” for ear reconstruction. The ingenious idea of passing a retroauricular flap through a tunnel in the cartilagineous framework to reach the anterior auricular surface has stimulated the interest in retroauricular skin for reconstruction of anterior defects of the ear.[13]
Similar to retroauricular skin, we can use preauricular skin as a pull-through flap with a superior base for the upper part of the antihelix and concha reconstruction after skin and cartilage excisions due to skin malignancy. This flap had a good shape, texture, and color and finally very good aesthetic results compared to skin graft. We must be careful about the thickness of the flap. The best thickness is similar to the thickness of the native skin and cartilage that have been excised.
CONCLUSIONS
We advocate that the banner pull-through flap with superior pedicle from postauricle and preauricle is an excellent choice for reconstruction of the upper antihelix ear reconstruction in both the crura and triangular fossa, especially after antihelix tumor excisions. This is a desirable method because its color, texture, and thickness match the defect functionally and aesthetically. In addition, the donor site of the flap in both the postauricle and preauricle has no visible scar.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Reconstruction of acquired auricular deformity. Operative Techniques in Otolaryngology-Head and Neck Surg. 2011;22:47-52.
- [Google Scholar]
- Superior pedicle retroauricular island flap for ear and temporal region reconstruction: Anatomic investigation and 52 cases series. Ann Plast Surg. 2008;60:652-7.
- [Google Scholar]
- Anteriorly pedicled retroauricular flap for repair of auricular defects. Aesthetic Plast Surg. 2012;36:623-7.
- [Google Scholar]
- Pull-through subcutaneous pedicle flap for an anterior auricular defect. Dermatol Surg. 2010;36:945-9.
- [Google Scholar]
- Anterior conchal reconstruction using a posteroauricular pull-through transpositional flap. Plast Reconstr Surg. 2004;113:2071-5.
- [Google Scholar]
- Reconstruction of congenital stenosis of external auditory canal with a post uricular chondrocutaneous flap. Plast Reconstr Surg. 1998;102:2320-4.
- [Google Scholar]
- Reconstruction of the anterior surface of the ear using a postauricular pull-through neurovascular island flap. Ann Plast Surg. 2006;56:609-13.
- [Google Scholar]
- Reconstruction of skin cancer defects of the auricle. J Oral Maxillofac Surg. 2004;l62:1457-71.
- [Google Scholar]
- Use of the earlobe in auricular reconstruction post tumour extirpation. J Plast Reconstr Aesthet Surg. 2009;62:539-41.
- [Google Scholar]
- Reconstruction of the ear after skin and perichondrium loss. Clin Plast Surg. 2002;29:187-200. vi
- [Google Scholar]
- Reconstruction of the ear after skin and cartilage loss. Clin Plast Surg. 2002;29:201-12. vi
- [Google Scholar]
- Technical innovations in ear reconstruction using a skin expander with autogenous cartilage grafts. J Plast Reconstr Aesthet Surg. 2008;61(Suppl 1):S59-69.
- [Google Scholar]
- Retroauricular skin: A flaps bank for ear reconstruction. J Plast Reconstr Aesthet Surg. 2008;61(Suppl 1):S44-51.
- [Google Scholar]






