Translate this page into:
Keystone Island Flap for Reconstructive Surgery—A Novel Approach
Address for correspondence: Dr. Eswari Loganathan, Department of Dermatology and Venereology, No 52, Victoria Hospital, Bengaluru 560002, Karnataka, India. E-mail: eshwaril@yahoo.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Keystone island flaps have a growing array of applications in reconstructive surgeries for the closure of simple and complex defects following the excision of skin tumors. It is a trapezoidal-shaped flap based on fasciocutaneous perforators. We share our experience with a 79-year-old man, who underwent keystone island flap reconstruction after the excision of biopsy-proven Bowen’s disease. A good aesthetic and functional outcome was obtained. With an ever expanding repertoire of reconstructive surgical techniques, the individualization of defect closure is of paramount importance in ensuring good cosmesis.
Keywords
Bowen’s disease
keystone island flap
reconstructive surgery
INTRODUCTION
The reconstruction of defects after the excision of skin tumors is a significant challenge. Small defects can be closed by local transposition, but larger defects pose a definite problem. Flaps are considered a better option than grafts because of better color and contour match. Keystone flaps serve as a versatile, simple, less time-consuming option for reconstruction.
CASE REPORT
A 79-year-old healthy man presented with a solitary hyperpigmented raised lesion on the left thigh since eighteen months. It was insidious in the onset, gradually progressed in size, and was associated with mild itching. Dermatological examination showed a solitary, oval, well-defined, brownish-black hyperpigmented plaque of 5 × 3 cm with scaling and crusting over the surface, on the anterior aspect of the left thigh [Figure 1]. Skin biopsy from the plaque showed features consistent with Bowen’s disease. The patient was advised topical 5 fluorouracil cream once a day application. Since there was no improvement, the lesion was planned for wide excision and closure with a keystone island flap.

- Ellipse drawn along the lesion and trapezoidal-shaped flap contoured along the side with 90° angle at the limits
After oncologic resection, the tissue defect was tailored to a 3:1 ellipse. The trapezoid-shaped flap was contoured along the side of the excisional defect, with right angles between the wound and the flap. The width of the flap was equal to the width of the wound [Figure 2]. The fascia was incised with no undermining of the flap or periphery. The flap was advanced toward the edge of the wound, and a stay suture was placed across the greatest line of tension [Figures 3 and 4]. The ends of the flap were closed from a V to a Y [Figures 5 and 6]. This created tissue laxity in the center of the flap, at right angles to the Y, and narrowed the secondary defect. There was typically an area of tissue redundancy that required excision. It healed with a good color match and gave good cosmetic and functional outcome [Figure 7].

- Blunt excision of the lesion

- Advancement of the flap toward the edge of the wound

- Placement of a stay suture across the greatest line of tension
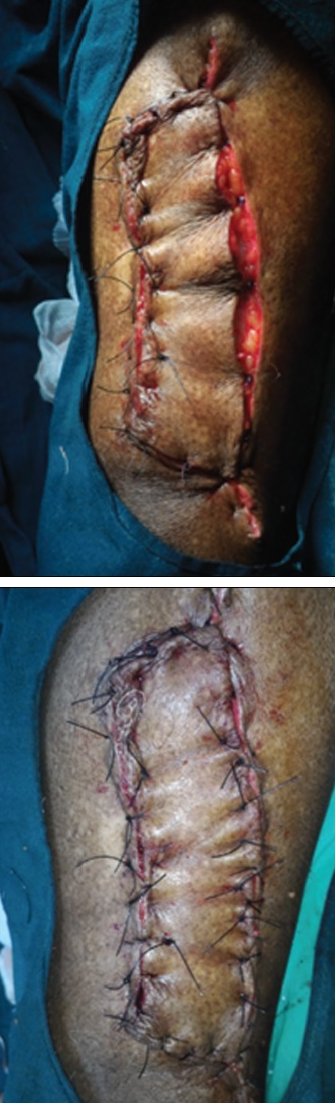
- Closure of ends of the flap from V to Y

- The final result of a keystone flap
DISCUSSION
The keystone island flap was described by Behan in 2003. It is a curvilinear-shaped, trapezoidal design flap, named after a stone called a keystone—a way of locking the Roman arches.[1] Based on fasciocutaneous perforators, the keystone island flap offers both the robust vascularity of perforator flaps and a relative ease and speed of local tissue rearrangement. It is based on the principle of converting soft-tissue defect in an area with no nearby tissue laxity into a secondary defect that has sufficient tissue laxity.[2]
The lesion should be excised in an elliptical manner with its axis along the line of cutaneous nerves, veins, or perforators. It is designed with a ratio of 1:1 between the width of the defect and the width of the flap. A right angle should be created at the ends of the excision to create the design of the keystone.[2]
Flap undermining is avoided to preserve the integrity of perforators, and all possible subcutaneous longitudinal venous and neural structures supporting the flap should be retained.
In the central portion, the flap is advanced parallel to the defect, whereas peripheral borders are advanced in a V-Y fashion. The direct apposition of the defect with a single layer of interrupted suture and V-Y advancement of the flap results in narrowing of the entire defect and creates tissue redundancy and laxity at the right-angle points, which may necessitate further excision.[1]
There are four different types of keystone flaps based on the depth and extent of dissection, which may be used in different locations based on skin laxity and defect size/depth: type I (direct closure), type II (with or without grafting), type III (double island flap), and type IV (rotation and advancement with or without grafting).[1]
We employed a type IIa flap with the division of deep fascia along the curvilinear line after the excision of Bowen’s disease. Therapeutic options for Bowen’s disease include medical and surgical methods. For lesions <2 cm, simple excision with minimum 4 mm margins and for larger lesions, and lesions at high-risk locations such as scalp, ears, eyelids, lips, and nose, wide excision with 6 mm margins are preferred.[3] The excision of larger lesions especially on the extremities poses a challenge for a proper wound closure. A keystone island flap is a simple, effective, and easily reproducible option.
Numerous advancements and modifications have been documented.[4] It has been used successfully for reconstruction after the excision of tumors like melanoma, squamous cell carcinoma, and basal cell carcinoma.[567]
Advantages of this technique include short operative time, high reproducibility, ease of use, and local tissue esthetic similarities. It employs immediately adjacent skin and soft tissue that provides a good color match in addition to reconstructing the contour of the defect, providing a far superior cosmetic result.[28]
CONCLUSION
A keystone flap is an easy and safe option for covering various limb defects with the least morbidity, provides a sensate cover, and minimizes the need for microsurgical techniques and long operative time. It offers additional advantages of good vascularity, ease of use, and good cosmetic coverage.[9]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- The keystone design perforator island flap in reconstructive surgery. ANZ J Surg. 2003;73:112-20.
- [Google Scholar]
- Evolving concepts of keystone perforator island flaps (KPIF): Principles of perforator anatomy, design modifications, and extended clinical applications. Plast Reconstr Surg. 2016;137:1909-20.
- [Google Scholar]
- Surgical margins for excision of primary cutaneous squamous cell carcinoma. J Am Acad Dermatol. 1992;27:241-8.
- [Google Scholar]
- Keystone flaps: Physiology, types, and clinical applications. Ann Plast Surg. 2019;83:226-31.
- [Google Scholar]
- Keystone flap reconstruction of primary melanoma excision defects of the leg-the end of the skin graft? Ann Surg Oncol. 2008;15:2867-73.
- [Google Scholar]
- A giant fungating metastatic basal cell carcinoma of the back and novel reconstruction using two large keystone design island perforator flaps. J Plast Reconstr Aesthet Surg. 2013;66:1015-8.
- [Google Scholar]
- Repair of a large lateral foot defect with a combination of keystone island flap and VY plasty. Eur J Dermatol. 2015;25:618-9.
- [Google Scholar]
- The keystone island flap: Use in large defects of the trunk and extremities in soft-tissue reconstruction. Plast Reconstr Surg. 2011;127:1212-21.
- [Google Scholar]






