Translate this page into:
Skin-saving modification of the rotation flap
*Corresponding author: Dr. Eckart Haneke, Department of Dermatology, Inselspital, University of Berne, 3010 Bern, Switzerland, Europe. haneke@gmx.net
-
Received: ,
Accepted: ,
How to cite this article: Haneke E. Skin-saving modification of the rotation flap. J Cutan Aesthet Surg. 2025;18:3-6. doi: 10.25259/JCAS_112_2024
“No flap creates new skin”
INTRODUCTION
The primary goal of dermatologic tumor surgery is complete removal of the neoplasm. The second aim is to provide good function with, third, as good a cosmesis as possible. However, in dermatologic oncology, particularly in individuals with light skin, one has always to keep in mind that a person with one primary skin cancer has a 30% risk to develop another primary cutaneous malignancy, and those with two or more primaries carry a risk of 65% or higher.1 Thus, skin-saving during cutaneous oncologic surgery and defect repair is of utmost importance. Local flaps are indicated where primary side-to-side closure is not possible, may it be due to the size of the defect or due to too much tension of the surrounding skin. If there is no axial artery, the flap is supplied by the vascular network at the base of the flap. These random pattern flaps should not exceed a length-to-width ratio of 2:1, as flap necrosis may occur.2 In areas of particular skin tension, like the back or lower leg, the venous backflow may be impaired by the tissue tension. Many flaps are available, meeting most demands to close small and large defects; however, no flap creates new tissue, and therefore, it is wise to save as much skin as possible. Rotation flaps have many advantages compared to simple advancement flaps as they are able to bring in more skin by moving the flap along a semicircular incision line.3,4 When operating on malignant tumors, it is important not to raise the flap from the area of lymphatic drainage to avoid potential metastases in the flap. Rotation flaps are useful for large defects of the trunk, scalp, face, and virtually all other regions of the body where defect closure is considered.3-5
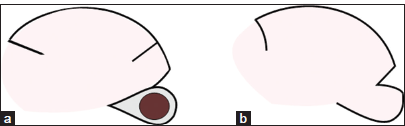
Graphic illustrations of flaps often show unnatural geometric figures and large Burow’s triangles, wasting a lot of skin [Figure 1 a and b]. Considering that many flaps can be seen as divided fusiform excisions [Figure 1a], one has to be aware that a simple fusiform excision with a width-to-length ratio of 3:1 wastes 73% (!) of skin in relation to the excised lesion,6 it is important to look for options to avoid this large skin loss. Some of these possibilities are special sutures and particular flap designs.3,7-9 Flaps can often be designed to avoid a Burow triangle either using a long pedicle that can be stretched out, by a back cut, or even by a Z plasty [Figure 2].7-10 A typical example of a flap without additional skin waste is the hatchet (kite) flap, which is a modified small rotation flap. Furthermore, the classical rotation flap can often be moved using a back cut instead of a Burow triangle as it has a broad flap base.5
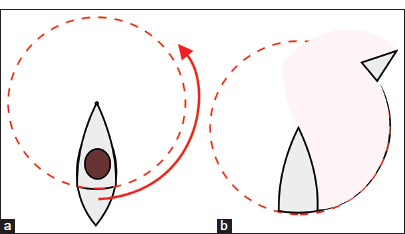
- (a) Classical design of a rotation flap. The flap can be seen as a divided fusiform excision whose one apical part is moved along a circular line, which is placed as a (b) Burow triangle into an area of skin availability. (a) The red arrow shows the direction of movement of the lower part of the fusiform excision, which thus becomes (b) the Burow triangle.
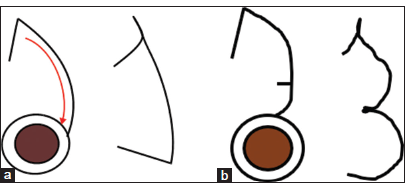
![The rotation flap has a broad base so that a back cut would not pose a risk to the blood supply of the flap. Rotation would result in a slightly shorter longitudinal side of the flap so that the flap incision should be a bit eccentrical [(a) black line and (b) dashed blue line].](/content/173/2025/18/1/img/JCAS-18-003-g002.png)
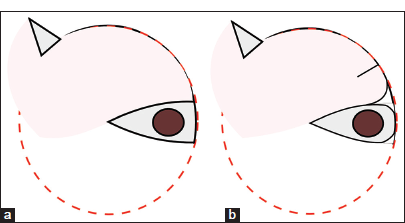
- The rotation flap has a broad base so that a back cut would not pose a risk to the blood supply of the flap. Rotation would result in a slightly shorter longitudinal side of the flap so that the flap incision should be a bit eccentrical [(a) black line and (b) dashed blue line].
We have used a small modification of the rotation flap11 that enables us to avoid some of the disadvantages of the classical rotation flap design.
METHODS
The classical rotation, as depicted in most textbooks and many articles, consists of an isosceles triangle with the acute angle at the pivot point (PP) in the center of a circle and two straight lines extending from the PP [Figures 1 and 2] to the circumference of the circle with the tumor to be removed in the center. This shows a triangle with two angles at the periphery that are roughly 90°. A Burow triangle is drawn at about 90° or more along the circular incision line according to the area of skin availability. The flap is then undermined from its tip to beyond the line connecting the PP with the far–most side of the Burow triangle [Figure 1b]. The extent of undermining determines the movability of the flap. Flap suture usually starts at the Burow triangle to avoid undue tension to the flap tip. However, this flap design does not take into account the particular shape of the tumor to be removed. The geometrical shape is not only unnecessary and unnatural but also it is a waste of valuable tissue. Further, the distal flap tip is at risk of vascular compromise at the end of the line of maximal skin tension.3
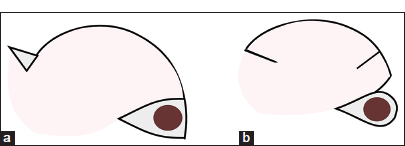
Considering this flap design, it was found that an acute angle at the tip of the triangle is not necessary for tumor removal and the rotation flap. Thus, the angle between the legs of the triangle and its base can be rounded off according to the shape of the lesion. The distal tip of the flap can now be adapted to the shape of the rounded “corner” or the flap’s opposite side [Figure 3]. This leaves a small triangular excess of skin at the outer circumference of the flap incision. With an incision of the flap opposite the excess skin, which is opened when the flap is rotated, it can then be fitted into place. This flap opening decreases the amount of necessary rotation, reduces the tension during rotation of the flap, avoids tip necroses, and saves skin [Figures 4-7]. This modification is also very useful for small rotation flaps like the kite flap [Figure 8].
- Direct comparison of the classical rotation flap design and the modification with flap incision. The extent of undermining of a rotation flap is shown in pink. (a) Common rotation flap. (b) Modified flap showing an incision of the flap at a distance approximately matching the width of the excision defect.
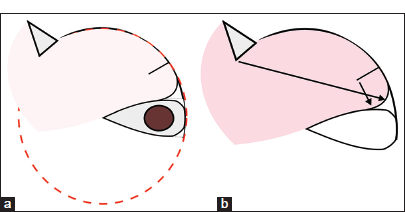
- (a) The excision of the lesion is drop-shaped with only one sharp angle at the pivot point of the rotation. (b) The line of maximum tension of the flap (black arrow) shows that there is no sharp-angled flap tip.
- (a) Direct comparison of the classical and (b) the modified rotation flaps, with (a) Burow triangle, with (b) back-cut.
- (a and b) Opening of the flap’s circumference reduces the tension along the flap margin.

- Large basal cell carcinoma of the right zygoma in an 84-year-old female patient. (a) Preoperatively. (b) End of Mohs surgery and defect repair with a modified cheek rotation flap. (c) One week after surgery, with a rotation flap with a notch. (d) Four weeks after the operation.
- Schematic illustration of a kite or hatchet flap. (a) “Classical” design. The red arrow indicates the direction of flap movement. (b) Modified hatchet flap.
DISCUSSION
Flaps are the indispensable tools of each dermatologic surgeon. Virtually all flaps, maybe except for free vascularized ones, are a daily routine in dermatosurgery. Many textbooks written by dermatologists lend strong evidence to this fact. Of the innumerable flaps described in the medical literature, quite a number were devised by dermatologists and they still strive for improvement of dermatologic surgery. Thanks to Burow’s invention, many flaps can be derived from fusiform excisions.12 In fact, whether it is linear or rotational advancement, they use the principle of dividing a spindle into two or more parts, of which the bigger one remains at its site and the smaller one, the Burow triangle, is moved along an incision line to an area of skin availability. Although there are many established patterns of advancement, there are virtually no limits to small modifications that make the flaps more versatile, safer, or more esthetically pleasing. The safety of a flap is very important as flap necrosis is often a catastrophe and irretrievably destroys important tissue. Rotation flaps are generally very safe because of their wide base, but there is always a place for improvement. We believe that this little modification is useful for flap repair in the face, head, and trunk and also in particularly difficult areas such as the lower extremities and the nail region.4 Its scar line is more natural as it is not a geometrical one but rather a broken line. The incision in the periphery of the flap shows a certain resemblance to a bilobed flap.
In summary, the modified rotation flap has proven to be a very useful and safe tool in the armamentarium of dermatologic surgeons for defect repair after cutaneous tumor removal.
References
- Treatment of skin tumors in the elderly. How to use flaps and grafts. Rev Med Liban. 1994;6:83.
- [Google Scholar]
- Indications for skin flaps and mechanism of flap survival In: Harahap M, ed. Principles of dermatologic plastic surgery. New York: PMA Publ Co; 1988. p. :145-55.
- [Google Scholar]
- Random pattern cutaneous flaps In: Robinson JK, Hanke CW, Sengelmann RD, Siegel DM, eds. Surgery of the skin: Procedural dermatology. Philadelphia, PA: Elsevier Mosby; 2005. p. :311-44.
- [CrossRef] [PubMed] [Google Scholar]
- Modifizierte Nahlappenplastiken zum Defektverschluß in spannungsreichen Hautarealen [Modified local flaps for defect closure in skin areas under tension] In: Mahrle G, Schulze HJ, Krieg T, eds. Wundheilung -Wundverschluß: Theorie und Praxis, chirurgische und konservative Maßnahmen [Wundhealing - Wound Closure: Theory and practice, surgical and conservative measures]. Fortschritte der operativen und onkologischen Dermatologie/Proceedings of surgical and oncologic dermatology. Vol 8. Berlin: Springer; 1994. p. :101-6.
- [CrossRef] [Google Scholar]
- Skin waste, vertex angle, and scar length in excisional biopsies: comparing five excision patterns--fusiform ellipse, fusiform circle, rhomboid, mosque, and S-shaped. Plast Reconstr Surg. 2004;113:857-61.
- [CrossRef] [PubMed] [Google Scholar]
- Recent developments and techniques in general cutaneous surgery. Surgery In: Dahl MV, Lynch PJ, Whitaker DC, eds. Current opinion in Dermatology. Vol 1. Philadelphia, PA: Current Science; 1994. p. :145-51.
- [Google Scholar]
- Developments and techniques in general cutaneous surgery. Surgery In: Dahl MV, Lynch PJ, Whitaker DC, eds. Current opinion in dermatology. Vol 2. Philadelphia, PA: Current Science; 1995. p. :129-36.
- [Google Scholar]
- Variationen der Flaschenzugnaht [Variations of the pulley suture] In: Mahrle G, Schulze HJ, Krieg T, eds. Fortschritte der operativen und onkologischen Dermatologie. 8 Wundheilung - Wundverschluß Heidelberg: Springer; 1994. p. :158-64.
- [CrossRef] [Google Scholar]
- Criteria and techniques of flaps In: Panconesi E, ed. Dermatology in Europe. Proceedings of the 1st Congress of the European Academy of Dermatology and Venereology. Florence 1989. Oxford: Blackwell Scientific Publications; 1992. p. :22-4.
- [Google Scholar]
- Advances in flaps and grafts in dermatologic surgery In: Roenigk RK, Roenigk HH, eds. Surgical dermatology - advances in current practice. London: M Dunitz Publ; 1993. p. :403-23.
- [Google Scholar]
- Beschreibung einer neuen Transplanationsmethode (methode der seitlichen Dreiecke) zum Wiederersatz verlorengegangener Theile des Gesichts [Description of a new transplantation method (method of lateral triangles) for the replacement of lost parts of the face] Berlin: Nauck; 1855.
- [Google Scholar]






